Adolescent Physical Abuse: Risk for Adolescent Psychiatric Disorders
Abstract
OBJECTIVE: The present study examined whether physical abuse functions as an additional risk factor for adolescent psychopathology after other important known risk factors are controlled for. METHOD: The authors recruited 99 adolescents aged 12 to 18 years directly from the New York State Department of Social Services after official documentation of physical abuse. The abused adolescents were compared to 99 nonabused adolescents matched for age, gender, race, and community income. Diagnostic interviews and measures of selected risk factors for psychopathology were administered to the adolescents and their parents and then entered into a multiple logistic regression model testing the added risk contributed by physical abuse to adolescent psychopathology. RESULTS: Physical abuse added significantly to other risk factors in accounting for lifetime diagnoses of major depression, dysthymia, conduct disorder, drug abuse, and cigarette smoking. Physical abuse also contributed significantly to prediction of current adolescent unipolar depressive disorders, disruptive disorders, and cigarette smoking. CONCLUSIONS: Since physically abused adolescents are at greater risk for the development of psychiatric disorders, recognition of adolescent abuse and the provision of psychiatric and substance abuse services may reduce morbidity. (Am J Psychiatry 1998; 155:954–959)
This study assessed the association between physical abuse of adolescents and adolescent psychopathology. It tested the hypothesis that the prevalence of psychiatric disorders, adjusted for selected risk factors, including parental psychopathology, is greater in physically abused adolescents than in nonabused adolescents.
Adolescents are involved in approximately 21% of child maltreatment cases (1). Compared to child abuse, adolescent abuse has been reported as less strongly associated with poverty and ethnic minority status (2), childhood maltreatment of the abusive parent (3), and low levels of parental education (4). It has also been suggested that adolescent abuse is more prevalent in females (2) and is a particularly suburban phenomenon, often related to family dysfunction (5).
Systematic controlled studies of the association between physical abuse and mental disorder have been lacking. Empirical studies of psychiatric disturbance in physically abused children have been hampered by failure to use structured interviews, reliance on groups referred for mental health treatments, failure to exclude subjects with sexual abuse histories, and ambiguous definitions of abuse. In one of the few studies that used structured interviews, Famularo et al. (6) found significantly more psychopathology in maltreated children than in control subjects. However, adolescents were not included and victims of sexual abuse were not excluded.
The risk factors reported for adolescent psychopathology include parental psychopathology (7–9), lack of family cohesion and adaptability (10), lack of perceived parental supportiveness and protection (11), prolonged separation from parents (12), head trauma (13), only one biological parent in the home (14, 15), divorce (14), being reared in a single-parent family (16), age of the adolescent (17), and gender (18). Unlike previous investigations, the present study systematically controlled for these factors in statistical analyses to determine whether physical abuse contributes independently to risk for psychopathology.
The study's abuse group, in contrast to those in most studies, was recruited directly from the abuse register of a state department of social services after physical abuse was confirmed. The abused subjects were compared to a nonabused community group matched for age, gender, race, and community income.
Semistructured and structured diagnostic interviews were used for the assessment of psychopathology in the abused adolescents and their parents. The interviews were conducted by clinically experienced psychology graduate students who were blind with respect to the subjects' abuse status. Diagnoses were arrived at through best-estimate procedures (19) by two experienced clinical research~ers who were blind to abuse status. Exposure to sexual abuse was an exclusion criterion, allowing the study to focus specifically on the effects of adolescent physical abuse.
METHOD
Subjects
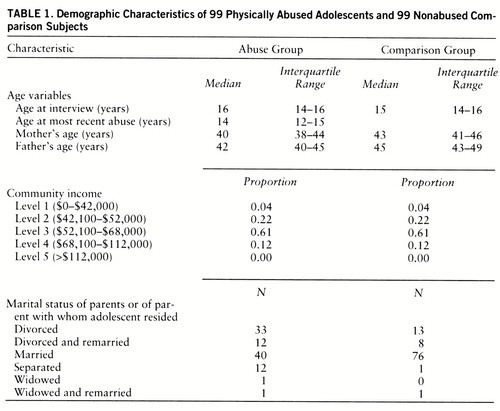
The study groups comprised 99 physically abused adolescents and their families and 99 comparison adolescents and their families, matched for age (one-half of the adolescents were in early adolescence—12–15 years old—and one-half were in late adolescence—16–18), gender (one-half were male, one-half were female), and community income (table 1). All of the subjects resided in suburban Long Island, New York. Only subjects who were Caucasian were included. The income for each subject was determined to be the median family income according to 1980 census data for the town in which that subject lived. A marketing search company matched potential comparison subjects to the abused subjects by using community residence as a proxy for socioeconomic status. The mothers of the abused adolescents were significantly younger than the mothers of the comparison adolescents (Mann-Whitney test, z=–2.90, p=0.004). There were no significant differences in the adolescents' or fathers' ages. The distribution of income for the pairs shows the study group to be middle to upper-middle class. The abused group contained fewer intact families than the comparison group and had significantly higher rates of parental divorce and separation (χ2=30.31, df=4, p=0.001).
All potential adolescent subjects were screened for sexual abuse by using a 12-item sexual behavior screen that assessed the adolescent's involvement in unwanted sexual contact. Any adolescent who reported sexual behavior with an adult at least 5 years older was excluded. Parents or adolescents with IQs of 70 or less, according to the vocabulary and block design subsets of the Wechsler Intelligence Scale (20), were also excluded. The Conflict Tactics Scale (21) was used to exclude physically abused comparison subjects.
Abused subjects. The abused subjects were adolescents aged 12 to 18 years who were confirmed as having been physically abused by a parent or stepparent. These subjects were drawn from a pool of 940 families meeting the study criteria who had been entered consecutively into the New York State Department of Social Services Central Register for Child Abuse in Nassau and Suffolk counties within the period from Jan. 1, 1989, through Dec. 31, 1991. The reports of child protective services included documented evidence of physical assault and/or injury (including excessive corporal punishment, bruises or welts, fractures, internal injuries, and/or burns). Of these families, 261 could not be located, reducing the pool to 679. These families were contacted in consecutive order until 124 families agreed to be in the study, a participation rate of 18.3%. However, 20 families were unable to complete the interviews and five did not meet the study criteria, resulting in a final group of 99 abuse cases.
Biological fathers were the perpetrators of abuse in 73% of the cases, mothers in 24%, and stepfathers in 12%. Multiple perpetrators were involved in 11% of the cases. Severity of abuse, based on an a priori scoring system, was calculated from agency records. Specifically, the algorithm consisted of a unit-weighted sum of points for specified types of injury, abusive behavior, and medical attention. Severity scores for the abuse group ranged from 1 to 36, with an interquartile range of 2–6. A score of 3 or less was received by 50% of the group, and 86% of the group fell at or below a severity score of 6. Although there was no difference in severity of adolescent abuse between the abuse group and the overall abuse pool, child protective services recommended treatment for 65% of the nonparticipating adolescents and 45% of the participating adolescents (χ2=7.35, df=1, p=0.007), suggesting that the adolescents in the overall pool were more disturbed than the participating subjects.
Comparison subjects. Comparison subjects were recruited from a pool of 219 adolescents residing in the same communities as the abused adolescents. The subjects in this pool were identified by a marketing research company using random-digit telephone dialing (a probability sampling procedure). The mothers of the participating comparison subjects had significantly more education than the mothers in the entire comparison pool (χ2=8.98, df=3, p=0.02). Of the participating comparison mothers, 20% had graduate or professional degrees, 51% reported some college education, 27% had completed high school, and 2% had not progressed beyond 8th grade. The educational levels of the mothers in the entire comparison pool were, respectively, 7%, 48%, 39%, and 6%, respectively. The fathers in the entire comparison pool had significantly lower occupational status than the participating comparison fathers (p=0.04, Fisher's exact test). The distribution of the occupational classes of the participating comparison fathers was as follows: 13% blue collar, 47% white collar, 30% professional, 6% entrepreneur, and 5% other; the distribution of the comparison pool was 26%, 34%, 21%, 17%, and 2%, respectively.
Procedures
Family members were assessed at home, and only one adolescent per family was interviewed. Although attempts were made to interview both biological parents, the fathers refused to participate in 48% of the abuse cases and 28% of comparison cases. Fathers were not recruited in cases where potential harm to the family could result. In these cases, information concerning the fathers' interactions within the family was obtained from the mothers' and adolescents' reports. The adolescents and family members each earned $50.00 per interview up to a maximum of $250.00 per family. Family identity was protected by a Federal Certificate of Confidentiality. The confidentiality of each family member's interview was strictly enforced; information was shared with other family members only if a risk of death was present. Written informed consent and assent were obtained from all adult participants and the adolescents, respectively. Ten percent of the families were deemed to be “at risk” or requested further feedback or referrals, and they were referred to the project social worker for follow-up.
Assessment Protocols
Adolescent and parental diagnoses were made independently by the first two authors, using a best-estimate procedure (19). The raters were blind to abuse status and to psychopathology among the subjects' family members. The following were reviewed for establishing the adolescents' diagnoses: the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Epidemiologic Version modified for DSM-III-R (22), the Conners' Teacher Rating Scale (23), the posttraumatic stress disorder (PTSD) module from the Structured Clinical Interview for DSM-III-R—Non-Patient Edition (SCID-NP) (24), and available school and medical information, except that which might reveal abuse status.
Parental axis I mental disorders were considered to be an important risk factor for adolescent psychopathology. The best-estimate procedures (19) for parental diagnosis were based on the SCID-NP (24), the Global Assessment Scale (GAS) (25), the Beck Depression Inventory (26), and the Wender-Utah Personality Inventory Hyperactive Syndrome Screen (27).
Other risk factors for adolescent psychopathology included the adolescents' perceptions of parental care and protection, measured by the Parental Bonding Instrument (28), and family cohesiveness and adaptability, assessed by using the Family Adaptability and Cohesion Evaluation Scale (29). Additional risk factors we considered were the number of biological parents in the home, reflecting divorce and single-parent status (14–16), separation of the adolescent from at least one biological parent for at least 6 months (12), adolescent age (17), gender (18), and history of head trauma (13). Although learning disability might also conceivably be considered a risk for psychopathology, the present study did not include measures allowing for accurate assessment of learning disabilities.
Statistical Analysis
An overall measure of risk for adolescent psychopathology was based on the total number of risk factors, calculated by assigning one point each for 1) any lifetime parental diagnosis of substance abuse, unipolar depression, anxiety disorder, and/or aggressive disorder, 2) a score on the Parental Bonding Instrument care scale below 15 or a score on the Parental Bonding Instrument protection scale below 7 for fathers, 3) a score on the Parental Bonding Instrument care scale below 20 or a score below 6 on the protection scale for mothers, 4) a score on the Family Adaptability and Cohesion Evaluation Scale lower than 32 or higher than 44 for family cohesion or lower than 20 or higher than 30 for adaptability, and 5) a single-parent family or the presence of only one biological parent in the home.
A multiple logistic regression model examined the effect of abuse on each adolescent psychiatric diagnosis. The model tested the additional risk for psychopathology due to abuse by simultaneously regressing all risk factors except abuse and then determining whether abuse contributed significantly to the prediction of the diagnosis.
Only risk factors present for at least 10 adolescents were modeled, excluding separation from a biological parent and head trauma. Diagnoses assigned to fewer than 10 adolescents were also not modeled, excluding bipolar disorder, schizophrenia, and anxiety disorders (other than PTSD).
The criteria for current diagnoses (within 6 months of the interview) were not generally met by enough subjects to allow for modeling. Therefore, the following current diagnoses were grouped together to allow for modeling: unipolar depression (dysthymia and/or major depression), substance abuse or dependence (alcohol abuse or dependence and/or drug abuse or dependence), and disruptive disorders (conduct disorder and oppositional defiant disorder). Current attention deficit hyperactivity disorder (ADHD) and cigarette smoking were sufficiently numerous to be modeled separately.
RESULTS
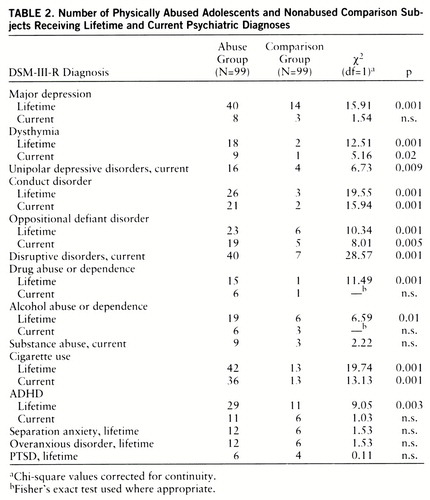
Without controlling for other risk factors, we carried out univariate comparisons on individual diagnoses. Table 2 presents the number of adolescents in each group diagnosed with each mental disorder, lifetime and current. Although these univariate results strongly suggest that psychiatric disorders are more prevalent in abused adolescents, the estimates are presented primarily for descriptive purposes, enabling comparisons with prevalence estimates from other studies of abused youth.
The univariate comparisons showed that the prevalence of disorders generally did not vary by gender. However, lifetime ADHD was more frequent among boys (N=27) than girls (N=13) (χ2=6.33, df=1, p=0.01). Cigarette use was more frequent among girls (N=36) than boys (N=19) (χ2=5.18, df=1, p=0.02).
There was a significant relationship between increasing age (categorized as 12–13, 14–15, and 16 years or older) and the following diagnoses: conduct disorder, both lifetime (χ2=6.33, df=2, p=0.05) and current (χ2=6.91, df=2, p=0.04); alcohol abuse or dependence, lifetime (χ2=15.41, df=2, p=0.001); drug abuse or dependence, lifetime (p=0.003, Fisher's exact test); substance abuse, current (p=0.04, Fisher's exact test); and cigarette use, both lifetime (χ2=27.57, df=2, p=0.001) and current (χ2=19.77, df=2, p=0.001). Therefore, age was controlled for in subsequent analyses.
As expected, more risk factors for psychopathology were present in the abuse group (median=3, interquartile range=2–5) than in the comparison group (median=1, interquartile range=0–2) (Mann-Whitney test, z=5.36, p=0.0001).
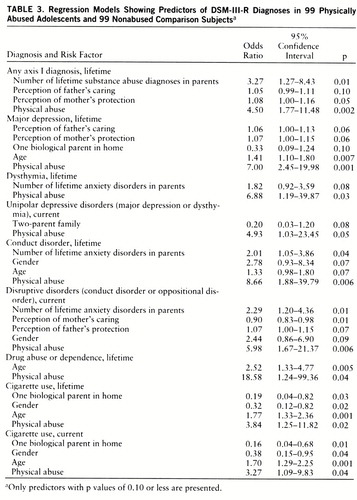
Logistic regression models also indicated higher rates of disorders in the abused adolescents after other risk factors were controlled for. Table 3 presents the lifetime and current disorders for which abuse contributed significantly to prediction after other risk factors were accounted for; risk factors with p values of 0.10 or less are reported.
With respect to lifetime psychiatric disorders, abuse increased the risk of being diagnosed with any axis I diagnosis. Other significant risk factors associated with lifetime axis I diagnoses were as follows: greater perception of mother's protection (i.e., overprotection), greater perception of father's caring, and higher number of parental substance abuse diagnoses.
For specific lifetime diagnoses, abuse increased the risk of being diagnosed with major depression, dysthymia, conduct disorder, drug abuse or dependence, and cigarette smoking. In addition to abuse, significant risk factors associated with lifetime major depression were as follows: greater perception of father's caring, greater perception of mother's protection, one biological parent in the home, and greater age. Number of lifetime parental anxiety disorders was an additional risk factor for dysthymia. Additional risk factors for conduct disorder were the following: male gender, number of parental anxiety disorders, and greater age. The one additional risk factor for drug abuse or dependence was greater age, while additional risk factors for cigarette use were the following: female gender, one biological parent in the home, and greater age.
With respect to current diagnoses, abuse increased the risk for being diagnosed with unipolar depressive disorders, disruptive disorders, and cigarette smoking. An additional significant risk factor for unipolar depressive disorders was living in a two-parent family. The additional risk factors for current disruptive disorders were as follows: less perception of mother's caring, greater perception of father's protection, male gender, and higher number of parental anxiety disorders. Additional risk factors for current cigarette use were the following: female gender, one biological parent in the home, and greater age.
Physical abuse did not contribute additionally to risk for lifetime or current ADHD or PTSD.
DISCUSSION
Although a cross-sectional study cannot, in and of itself, establish a causal relationship between physical abuse and psychopathology, this study controlled for important risk factors for adolescent psychopathology in two closely matched groups. In this context, the additional risk for adolescent psychopathology due to physical abuse was estimated. The results support the hypothesis that physical abuse during adolescence is associated with greater risk for developing adolescent psychiatric disorders. After we accounted for other important risk factors, which were more prevalent in the abuse group, physical abuse raised the risk for the occurrence of unipolar depressive disorders, disruptive disorders, drug abuse, and cigarette use.
Depression has long been associated with abuse (30). Our finding that abused adolescents were seven times as likely to develop a major depressive disorder is consistent with this. Two factors have been previously suggested to explain the prevalence of depression in survivors of physical abuse: a higher prevalence of affective disorders in the family histories of abuse victims (10) and learned helplessness, reported by Walker (31) to be characteristic of women in abusive households. It is notable that the abused boys in this study were as likely as the abused girls to be diagnosed with depressive disorders. This is in contrast to the expected higher rate of depression in adolescent girls (personal communication from S. Blumenthal, 1996).
In addition to the risk for major depression, the abused adolescents were seven times as likely to develop dysthymia. Kovacs et al. (32) reported that unipolar depressive disorders in children and adolescents often initially appear as dysthymia rather than major depressive disorder. Our results highlight the importance of addressing the full spectrum of depressive disorders in abuse victims.
The finding that conduct disorder is approximately nine times as likely to occur in abused subjects is consistent with a large body of literature documenting a strong association between abuse, delinquency, and aggressive behavior. However, whereas the general literature indicates a higher prevalence of conduct disorder in boys (15, 33), the abused girls in this study were almost as likely as the abused boys to receive the diagnosis.
Similarly, our finding that physically abused adolescents are nearly 19 times as likely to abuse drugs is consistent with previous findings on youth referred for substance abuse treatment (34), suggesting that adolescents may use drugs as an adaptive mechanism for coping with abuse (35). That girls were as likely as boys to receive diagnoses of drug abuse or dependence confirms other reports of the association between family violence exposure and substance abuse in females (32, 34).
The increasing recognition that cigarette smoking is associated with depressive disorders (36) led us to examine the association between abuse and smoking. The finding that abused adolescents, especially girls, were more likely to smoke suggests that this subgroup may be at particular risk for the physical and behavior problems associated with cigarette use.
The moderate severity of injury in the abuse group is typical of adolescent physical abuse reported elsewhere (1, 4) and is likely related to the fact that adolescents are better able to defend themselves than prepubertal children. The moderate level of violence experienced may account for the low occurrence of PTSD, characteristic of severe trauma, in this abuse group.
Concerning the issue of the generalizability of these findings, two sources of bias exist in our study. Cases handled by child protective services do not include all cases of abuse in the population, and abuse severity is probably less in cases not reaching public notice. Insofar as psychopathology is a function of abuse severity, our rates of psychopathology likely overestimate the rate in the general population of abused youth. However, abuse may be more severe in families declining participation. Although our severity estimates did not support this, the high refusal rate, although typical of other community-recruited abuse samples, and the higher incidence of referrals by child protective services for treatment in the overall abuse pool give rise to concern. To the extent that our index did not adequately estimate abuse severity, our findings of the greater risk for psychiatric disorders in abused adolescents is conservative.
Second, utilization of an all-white suburban sample may have yielded estimates of the relationship between abuse and psychiatric disorders that differ from those that would be found in other studies, especially studies sampling minorities or from urban settings. Conditions in inner-city neighborhoods produce high levels of parenting stress, contributing to increased abuse and a higher prevalence of psychiatric disorders, thereby affecting the relationship between physical abuse and mental disorder. To properly assess the mental health needs of all physically abused adolescents, it is necessary to conduct similarly rigorous diagnostic research with other homogeneous groups from both urban and suburban areas.
Drug abuse, conduct disorder, and depression have all been associated with aggressive behavior toward oneself and others (4, 37, 38). However, fewer than 5% of abuse victims receive mental health services (39). Our findings highlight the importance of increased identification of physically abused adolescents so that mental health and substance abuse services can be provided. Future research should more firmly establish the relationship between the provision of such services and the reduction of violence. Such interventions for abused adolescents would be expected to 1) reduce the occurrence of self-injury, 2) diminish the contribution of abused adolescents to violent crime in the general community, and 3) decrease the occurrence of future violent acts within the adolescents' own families.
 |
 |
 |
Received Aug. 26, 1996; revisions received May 29 and Dec. 3, 1997; accepted Jan. 15, 1998. From the Departments of Psychiatry and Biostatistics, North Shore University Hospital, New York University School of Medicine. Address reprint requests to Dr. Kaplan, Department of Psychiatry, North Shore University Hospital, 300 Community Dr., Manhasset, NY 11030. Funded by NIMH grant MH-43772.
1 Child Maltreatment 1994: Reports From the States to the National Center on Child Abuse and Neglect, US Department of Health and Human Services. Washington, DC, US Government Printing Office, 1996Google Scholar
2 Garbarino J, Schellenbach C, Sebes J: Troubled Youth, Troubled Families: Understanding Families at Risk for Adolescent Maltreatment. New York, Aldine, 1986Google Scholar
3 Berdie J, Berdie M, Wexler S, Fisher B: An Empirical Study of Families Involved in Adolescent Maltreatment: Final Report. Washington, DC, US Department of Health and Human Services, National Center on Child Abuse and Neglect, 1983Google Scholar
4 American Medical Association Council on Scientific Affairs: Adolescents as victims of family violence. JAMA 1993; 270:1850–1858Crossref, Medline, Google Scholar
5 Pelcovitz D, Kaplan S, Samit C, Krieger R, Cornelius D: Adolescent abuse: family structure and implications for treatment. J Am Acad Child Psychiatry 1984; 23:458–464Crossref, Medline, Google Scholar
6 Famularo R, Kinscherff R, Fenton T: Psychiatric diagnoses of maltreated children: preliminary findings. J Am Acad Child Adolesc Psychiatry 1992; 13:863–867Crossref, Google Scholar
7 Rutter M: Paternal mental disorder as a psychiatric risk factor, in Psychiatry Update: American Psychiatric Association Annual Review, vol 6. Edited by Hales RE, Frances AJ. Washington, DC, American Psychiatric Press, 1987, pp 647–661Google Scholar
8 Weissman MM, Prusoff BA, Gammon GD, Merikangas KR, Leckman JF, Kidd KK: Psychopathology in the children (ages 6–18) of depressed and normal parents. J Am Acad Child Psychiatry 1984; 23:78–84Crossref, Medline, Google Scholar
9 Kaplan S, Pelcovitz D, Salzinger S: Psychopathology of parents of abused and neglected children. J Am Acad Child Adolesc Psychiatry 1983; 22:238–244Crossref, Medline, Google Scholar
10 Wolkind S, Rutter M: Separation, loss and family relationships, in Child and Adolescent Psychiatry: Modern Approaches, 2nd ed. Edited by Rutter M, Hersov L. Oxford, England, Blackwell Scientific, 1985, pp 34–57Google Scholar
11 Keller M, Beardslee W, Dorer D: Impact of severity and chronicity of parental affective illness on adaptive functioning and psychopathology in children. Arch Gen Psychiatry 1986; 43:930–937Crossref, Medline, Google Scholar
12 Rutter M: Parent-child separation: psychological effects on the children. J Child Psychol Psychiatry 1971; 12:233–260Crossref, Medline, Google Scholar
13 Rutter M, Chadwich O, Shaffer O: Head injury, in Developmental Neuropsychiatry. Edited by Rutter M. New York, Guilford Press, 1983, pp 83–111Google Scholar
14 Barber BL, Eccles JS: Long-term influence of divorce and single parenting on adolescent family- and work-related values, behaviors, and aspirations. Psychol Bull 1992; 111:108–126Crossref, Medline, Google Scholar
15 Pearson JL, Ialongo NS, Hunter AG, Kellam SG: Family structure and aggressive behavior in a population of urban elementary school children. J Am Acad Child Adolesc Psychiatry 1994; 33:540–548Crossref, Medline, Google Scholar
16 Velez CN, Johnson J, Cohen PA: Longitudinal analysis of selected risk factors for childhood psychopathology. J Am Acad Child Adolesc Psychiatry 1989; 28:861–864Crossref, Medline, Google Scholar
17 Lewinsohn PM, Clarke GN, Seeley JR, Rohde P: Major depression in community adolescents: age at onset, episode duration and time to recurrence. J Am Acad Child Adolesc Psychiatry 1994; 33:809–818Crossref, Medline, Google Scholar
18 Bird HR, Gould M, Yager T, Gould M, Staghezza B, Canino G: Risk factors for maladjustment in Puerto Rican children. J Am Acad Child Adolesc Psychiatry 1989; 28:847–850Crossref, Medline, Google Scholar
19 Leckman J, Sholkomskas O, Thompson W, Belanger A, Weissman M: Best estimate of lifetime psychiatric diagnosis. Arch Gen Psychiatry 1982; 39:879–883Crossref, Medline, Google Scholar
20 Silverstein AB: Two- and four-subtest short forms of the Wechsler Adult Intelligence Scale—Revised. J Consult Clin Psychol 1982; 50:415–418Crossref, Google Scholar
21 Straus M: Measuring intrafamily conflict and violence: the Conflict Tactics Scale. J Marriage and the Family 1979; 41(1):75–88Google Scholar
22 Orvaschel H, Puig-Antich J, Chambers W, Tabrizi MA, Johnson R: Retrospective assessment of prepubertal major depression with the Kiddie-SADS-E. J Am Acad Child Psychiatry 1982; 21:4:392–397Google Scholar
23 Conners CK: A teacher rating scale for use in drug studies with children. Am J Psychiatry 1969; 126:884–888Link, Google Scholar
24 Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R—Non-Patient Edition (SCID-NP, Version 1.0). Washington, DC, American Psychiatric Press, 1990Google Scholar
25 Endicott J, Spitzer RL, Fleiss JL, Cohen J: The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry 1976; 33:766–771Crossref, Medline, Google Scholar
26 Beck AT, Steer RA: Manual for the Revised Beck Depression Inventory. San Antonio, Psychological Corp, 1987Google Scholar
27 Gomez RL, Janowsky D, Zeitin M, Huey L, Clopton R: Adult psychiatric diagnoses and symptoms compatible with the hyperactive child syndrome: a retrospective study. J Clin Psychiatry 1981; 42:389–394Medline, Google Scholar
28 Parker G, Tupling H, Brown LB: A parental bonding instrument. Br J Med Psychol 1979; 52:1–20Crossref, Google Scholar
29 Olsen D, Portner J, Lavee J: FACES III. St Paul, Family Social Sciences, 1985Google Scholar
30 Kazdin A, Moser J, Colbus D, Bell R: Depressive symptoms among physically abused and psychiatrically disturbed children. J Abnorm Psychol 1985; 94:298–307Crossref, Medline, Google Scholar
31 Walker LE: The Battered Woman's Syndrome. New York, Springer, 1984Google Scholar
32 Kovacs M, Akiskal HS, Gatsonis C, Parrone PL: Childhood-onset dysthymic disorder: clinical features and prospective naturalistic outcome. Arch Gen Psychiatry 1994; 51:365–374Crossref, Medline, Google Scholar
33 Bauermeister JJ, Canino G, Bird H: Epidemiology of disruptive behavior disorders. Child Adolesc Psychiatr Clin North Am 1994; 3:177–194Crossref, Google Scholar
34 Cavaiola AA, Schiff M: Behavioral sequelae of physical and/or sexual abuse in adolescence. Child Abuse Negl 1988; 12:181–188Crossref, Medline, Google Scholar
35 Goodwin J: Post-traumatic symptoms in incest victims, in Post-Traumatic Stress Disorder in Children. Edited by Eth S, Pynoos RS. Washington, DC, American Psychiatric Press, 1985, pp 155–168Google Scholar
36 Glassman AH: Cigarette smoking: implications for psychiatric illness. Am J Psychiatry 1983; 150:546–553Google Scholar
37 Kaufman J, Zigler E: Do abused children become abusive parents? Am J Orthopsychiatry 1987; 67:186–192Google Scholar
38 Harrington MRC, Fudge H, Rutter M, Pickles A, Hill J: Adult outcomes of childhood and adolescent depression, II: links with antisocial disorders. J Am Acad Child Adolesc Psychiatry 1991; 30:434–439Crossref, Medline, Google Scholar
39 United States Advisory Board Report on Child Abuse and Neglect: Critical First Steps in Response to a National Emergency. Washington, DC, US Department of Health and Human Services, 1990Google Scholar



