Association Between Cognitive Functioning and Employment Status of Persons With Bipolar Disorder
Abstract
OBJECTIVE: The purpose of this study was to identify variables associated with employment status among persons with bipolar disorder, including cognitive functioning, severity of symptoms, demographic variables, and variables related to course of illness. METHODS: The authors assessed the current employment status of 117 persons with bipolar disorder. Study participants' cognitive functioning was evaluated with the Repeatable Battery for the Assessment of Neuropsychological Status, the information and letter-number sequencing subtests of the Wechsler Adult Intelligence Scale III, and part A of the Trail Making Test. Symptoms were rated by using the Brief Psychiatric Rating Scale, the Hamilton Depression Scale, and the Young Mania Rating Scale. A stepwise multivariate logistic regression analysis was used to predict employment status. RESULTS: Fifty-one percent of the study participants had no current work activity, 21 percent worked part-time or as volunteers, and 27 percent had full-time competitive employment. Current employment status was significantly associated with cognitive performance, especially immediate verbal memory, total symptom severity, history of psychiatric hospitalization, and maternal education. No association was found between employment status and history of psychotic symptoms, number of years of education, or age at onset of illness. CONCLUSIONS: Vocational programs for persons with bipolar disorder would benefit from inclusion of a formal cognitive assessment to better assess work potential and to study the predictors of work-related outcomes.
Bipolar disorder is a pervasive psychiatric illness of unknown etiology. Although the study of persons with bipolar disorder has traditionally focused on the characteristic mood symptoms, interest has been increasing in psychosocial outcomes, including employment, interpersonal relationships, and overall quality of life. The results of recent studies suggest that there is wide variability in psychosocial outcomes among affected individuals. It is estimated that as many as 30 to 60 percent of persons with bipolar disorder do not regain full social or occupational functioning after the onset of their illness (1). Functional recovery often lags behind recovery from symptoms and may still be incomplete when acute mood symptoms have subsided (2,3,4).
Impairment in employment status is an important aspect of psychosocial disability. In a six-month follow-up of 67 patients who were hospitalized for a manic episode, Dion and colleagues (3) found that only 43 percent of the patients were employed, even though 80 percent were symptom free or only mildly symptomatic. In a prospective study of 73 patients hospitalized for mania who were evaluated 1.7 years later, Harrow and colleagues (5) found that only 42 percent had steady employment throughout the follow-up period and that 23 percent had been continuously unemployed. Similar findings emerged from a five-year follow-up study by Coryell and colleagues (2) of 148 patients with bipolar disorder. Sixty-two percent of the patients were employed in the year before the study, a rate that was significantly lower than that in a comparison sample of persons without a mood disorder.
Cognitive functioning has been postulated as a determinant of psychosocial and employment outcomes in bipolar disorder but has not been the focus of systematic investigation (1,6). The purpose of the cross-sectional study reported here was to identify the variables associated with employment status among persons with bipolar disorder, including cognitive functioning, severity of symptoms, demographic variables, and variables related to course of illness.
Methods
The study cohort consisted of 117 persons with bipolar disorder from the Baltimore area. Participants were recruited through announcements posted at psychiatric treatment centers and a self-help organization for persons with mood disorders. All participants were aged 18 to 65 years; had a diagnosis of bipolar disorder confirmed by the Structured Clinical Interview for DSM-IV (SCID) (7,8); did not have current substance abuse (previous month) or any history of intravenous substance use; did not have mental retardation; did not have a clinically significant medical disorder that would affect cognitive performance, including stroke or another neurologic disorder; and were not currently receiving inpatient care.
The study was approved by the institutional review board of the Sheppard Pratt Health System in accordance with established guidelines. Participants provided written informed consent and were seen for one study session that lasted up to 90 minutes. A structured interview included questions about the course of illness and previous hospitalizations, educational level of the participant and his or her parents, the presence of psychotic symptoms currently or in the past, current psychiatric symptoms and psychosocial functioning, and current medications. Current employment status was categorized as unemployed or no current work activity; current participation in volunteer work, sheltered work, or part-time competitive work (less than 20 hours per week) or part-time student status; or current participation in full-time competitive work (at least 20 hours per week) or full-time student status. Symptoms were rated by using the Brief Psychiatric Rating Scale (BPRS) (9), the Hamilton Depression Scale (10), and the Young Mania Rating Scale (11).
To assess cognitive functioning, participants were administered form A of the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) (12). The RBANS comprises 12 subtests that yield five indexes and a total RBANS score. The test indexes are immediate memory (list learning and story memory), visuospatial and constructional (figure copy and line orientation), language (picture naming and fluency), attention (digit span and coding), and delayed memory (list recall, story recall, figure recall, and list recognition). Each index score is expressed as an age-adjusted standard score with a mean of 100 and a standard deviation of 15. Participants were also administered two subtests from the Wechsler Adult Intelligence Scale III (WAIS-III) (13)—the information subtest and the letter-number sequencing test—as well as part A of the Trail Making Test (14). The study data were collected between June 1, 2001, and October 31, 2002.
Univariate analyses of variance were used to identify relationships between employment status and continuous demographic, symptomatic, and cognitive variables. Chi square analyses were used to determine the relationship between employment status and dichotomous or categorical variables. Variables that showed a significant relationship with employment status in the univariate analyses (p<.05) were entered into a stepwise multivariate logistic regression analysis using three levels of employment status (15). All the analyses were performed with use of STATA, version 7.0.
Results
The study cohort of 117 persons comprised 35 men (30 percent) and 82 women (70 percent). The mean±SD age of the participants was 41.4±12.2 years (range, 18 to 64 years). A total of 98 participants (84 percent) were Caucasian, 16 (14 percent) were African American, and three (3 percent) were Asian American. The mean number of years of education was 14.3±2.9. The mean age at onset of mood disorder was 20±9.4 years, with a mean duration of mood disorder of 21.6±12.5 years. A total of 98 participants (84 percent) had been hospitalized for their psychiatric illness; the mean time since the last hospitalization among those who had been hospitalized was 49.7±69.8 months.
Diagnoses in the sample were divided among bipolar I, most recent episode manic (24 patients, or 21 percent); bipolar I, most recent episode depressed (44 patients, or 38 percent); bipolar I, most recent episode mixed (19 patients, or 16 percent); bipolar II, most recent episode hypomanic (13 patients, or 11 percent); bipolar II, most recent episode depressed (16 patients, or 14 percent); and bipolar disorder not otherwise specified (one patient, or 1 percent). A total of 115 study participants (98 percent) reported that they were currently receiving psychotropic medications: 67 (57 percent) were receiving an antipsychotic agent, six (5 percent), an anticholinergic agent; 33 (28 percent), lithium; 103 (88 percent), a mood stabilizer, including lithium; and 74 (63 percent), an antidepressant.
Sixty participants (51 percent) had no work activity; 25 (21 percent) were involved in volunteer work, sheltered employment, or part-time competitive employment; and 32 (27 percent) had full-time competitive employment.
The results of the univariate analyses showed a significant relationship between employment status and many of the cognitive and symptom variables as well as several demographic variables and variables related to course of illness, as can be seen in Table 1. For all the cognitive and symptom variables shown in the table, there was an ordinal relationship between employment status and the clinical measure. Greater cognitive functioning and lower severity of symptoms were associated with a better employment status.
The following variables were not significantly associated with employment status in the univariate analyses: history of psychotic symptoms, Hamilton Depression Scale score, score on the information subscale of the WAIS-III, duration of mood disorder; number of years of education, current anticholinergic medication, age, gender, race, diagnostic subtype, age at onset of mood disorder, age at first psychiatric hospitalization, and time since last hospitalization.
Stepwise ordered logistic regression of employment status defined a model in which the following variables contributed independently to employment status by the likelihood ratio test: RBANS total score (χ2=11.08, df=1, p≤.001), Brief Psychiatric Rating Scale total score (χ2=8.18, df=1, p=.004), previous hospitalization for psychiatric illness (χ2=13.49, df=1, p≤.001), and maternal education (χ2=3.83, df=1, p=.05). The overall model was significant (χ2=45.95, df=4, p<.001). The logistic regression was used to predict employment status from these variables and correctly predicted the employment status of 70 (64 percent) of 110 participants for whom there were complete data on the four variables. Young Mania Rating Scale score, letter-number subtest score, current antipsychotic medication, and score on part A of the Trail Making Test were removed from the model by the stepwise logistic regression.
To identify the components of the RBANS that independently contributed to the relationship between the RBANS and employment status, a stepwise ordered logistic regression was performed on employment status with the RBANS index scores. Only the immediate memory subscale of the RBANS contributed independently to employment status (χ2=16.82, df= 2, p≤.001).
Discussion
We determined the effects of demographic, cognitive, and symptom variables on the point prevalence of employment status in a cohort of 117 persons with bipolar disorder. Several variables were independently associated with current employment status in this sample: performance on a brief neuropsychological test battery, total severity of symptoms, a history of psychiatric hospitalization, and the level of maternal education.
Our study provides data about a question that has been identified as important by investigators—the degree to which cognitive factors may contribute to psychosocial and work outcomes among patients with bipolar disorder (1,6). We found that cognitive performance was significantly associated with employment status apart from the effects of severity of symptoms and other variables. As a group, our study participants demonstrated a range of performances on the RBANS and other cognitive measures. Their mean scores were below those that would be expected for nonpsychiatric patients, a finding that is consistent with the observation that some patients with bipolar disorder have relative deficits in cognitive performance (16,17,18,19).
Cognitive factors have also been found to contribute to the employment status of persons with schizophrenia. In vocational rehabilitation programs for patients with schizophrenia, cognitive variables have been identified as predictors of employment outcomes (20,21,22,23). Cognitive factors may operate in a similar manner in bipolar disorder, even though the overall level of cognitive impairment is not as great as that seen with schizophrenia (24,25,26).
Among the cognitive indexes that make up the RBANS total score, immediate verbal memory made the greatest contribution to employment status in our sample. This salience of immediate verbal memory is consistent with the association between verbal memory and functional outcomes across different studies of schizophrenia (27). One study found that verbal memory was strongly associated with baseline work performance among persons with schizophrenia who were participating in a rehabilitation program (21). The extent to which verbal memory ability is correlated with specific work behaviors has not been examined among persons with bipolar disorder receiving vocational services.
Total symptom severity as measured by the BPRS was also significantly associated with employment status in our study. Our results are consistent with those of Altshuler and colleagues (28), who found that residual symptoms of depression were significantly and inversely correlated with global ratings on the Global Assessment of Functioning Scale, even though no patient had a depression score high enough to indicate clinical depression. Looking specifically at the predictors of work functioning in a sample of 52 outpatients with bipolar disorder, Hammen and colleagues (29) found that total symptom scores summed over repeated assessments during a one-year period were associated with work functioning. However, the association between symptoms and work status was not significant in a multivariate analysis that included interpersonal functioning and personality characteristics. Gitlin and colleagues (30) also looked at cumulative psychopathology, operationalized as average symptom ratings over a follow-up period of 4.3 years. The measure of psychopathology was predictive of overall psychosocial outcome and was a better predictor than was the number of illness episodes.
Having ever been hospitalized for psychiatric illness emerged as an independent predictor of poorer employment status in our study. This finding is interesting in that most individuals in the sample (84 percent) had had a psychiatric hospitalization at some point. However, almost all the persons in the unemployed group had been hospitalized, compared with 66 percent in the competitively employed group. An absence of previous hospitalizations may indicate a more benign course of illness with less severe symptoms or fewer relapses over the history of the illness. It is also possible that persons who are hospitalized are more likely to lose their jobs as a result of being absent from the workplace or because of the stigma associated with mental illness.
Of note, neither diagnostic subtype nor the distinction between bipolar I and II disorder was significantly associated with history of hospitalization in our sample. Nor did we find a significant association between employment status and either time since the last hospitalization or the age of the first admission among those who had been hospitalized. Although we do not have data on the number or duration of hospitalizations of study participants, these variables are likely to be influenced by factors other than clinical ones, given the inconsistent and changing standards for length of hospital stay. Our findings contrast with those of Hammen and associates (29), who found that history of hospitalization was not independently associated with a measure of vocational adjustment in a sample of persons with bipolar I disorder. Differences between that study and ours in sample size and selection, as well as in the measure of vocational functioning, may account for the different results.
Maternal educational level was used in our study as a proxy for premorbid family socioeconomic status and was marginally significant in the multivariate analysis. The educational level of participants themselves was not associated with employment status. Several other studies have found that premorbid socioeconomic status was related to psychosocial outcomes among patients with bipolar disorder (5,31,32), but these studies did not examine employment outcomes specifically. The mechanism of the effect of premorbid socioeconomic status is not clear. Perhaps premorbid socioeconomic status is associated with a person's expectations about his or her employment potential when faced with a serious mental illness or with the availability of social and vocational opportunities.
Although receipt of antipsychotic medication at the time of the study was associated with poorer employment status in the univariate analysis, this variable did not emerge as an independent predictor in the multivariate analysis. The study participants were taking a variety of medications and combinations of medications. We analyzed medication data only by major medication classes. Like Levine and colleagues (33), we found no significant difference in employment status by the type of medication prescribed when we controlled for other variables that also affect employment status.
The results of our study are consistent with those of previous studies in showing a high rate of unemployment and a relatively low rate of competitive employment among persons with bipolar disorder (2,3,5). This finding is all the more striking given that all the participants in our study were outpatients and, among those who had previously been hospitalized, had a long interval since the last hospital admission—on average, 50 months. As noted by Coryell and colleagues (2), the consequences of bipolar disorder are severe, enduring, and persistent.
Our study sample may not be representative of persons with bipolar disorder. Study announcements were posted in psychiatric centers and also distributed through a self-help organization. Both of these approaches to recruitment may have led to selection bias in favor of more severely ill and more impaired individuals. In addition, we do not know the number of persons in our sample who were receiving Social Security disability payments. Such payments may serve as a disincentive to seeking competitive employment among persons with mental illness. Information about Social Security income has not been provided in other studies (2,3,29) and would be an important variable to include in future investigations of employment outcomes.
Limitations of the study include the fact that the design was cross-sectional. Our data did not enable us to analyze the temporal sequence of events leading to employment outcomes or the cause-and-effect relationship among the variables that we studied. Nor could we assess the role of the participants' vocational motivation. In addition, our measure of employment status did not provide a fine-tuned measure of vocational adjustment and did not address the degree to which participants' work was consistent with their preparation, interests, and salary expectations.
Another limitation is that we assessed cognitive functioning on the basis of a relatively brief screening battery. A more detailed and comprehensive cognitive assessment would enable a more thorough evaluation of the role of cognitive variables associated with work outcomes. Finally, there may be other factors that we did not measure that are related to employment status. For example, drug and alcohol abuse, comorbid medical illness, and medication noncompliance may all have an adverse effect on employment outcomes among persons with bipolar disorder and were not included as variables in our study.
Conclusions
The results of this study underscore the extent of employment impairment among persons with bipolar disorder. The severity of residual symptoms is only one factor of several that are associated with employment status. Cognitive functioning, especially verbal memory abilities, appears to play a significant role and merits further investigation. Vocational programs for persons with bipolar disorder would benefit from inclusion of a formal cognitive assessment to better assess employment potential and to study the predictors of employment-related outcomes. Longitudinal studies are needed to define the relationship between cognitive functioning and the response to vocational interventions.
Acknowledgment
This study was supported by the Stanley Medical Research Institute.
All authors except Dr. Yolken are affiliated with the Sheppard Pratt Stanley Research Center in Baltimore. Dr. Yolken is with the department of pediatrics at Johns Hopkins University in Baltimore. Send correspondence to Dr. Dickerson at Sheppard Pratt, 6501 North Charles Street, Baltimore, Maryland 21204 (e-mail, [email protected]).
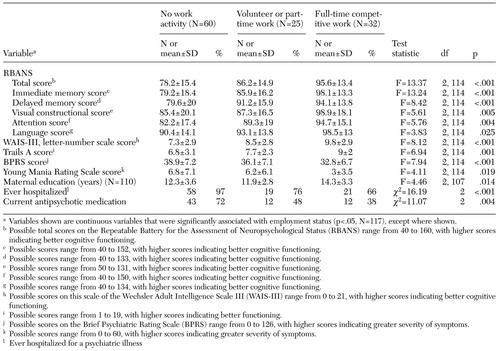 |
Table 1. Results of univariate analyses of clinical and demographic variables and employment status in a sample of persons with bipolar disorder
1. MacQueen GM, Young LT, Joffe RT: A review of psychosocial outcome in patients with bipolar disorder. Acta Psychiatrica Scandinavica 103:163–170, 2001Crossref, Medline, Google Scholar
2. Coryell W, Scheftner W, Keller M, et al: The enduring psychosocial consequences of mania and depression. American Journal of Psychiatry 150:720–727, 1993Link, Google Scholar
3. Dion GL, Tohen M, Anthony WA, et al: Symptoms and functioning of patients with bipolar disorder six months after hospitalization. Hospital and Community Psychiatry 39:652–656, 1988Abstract, Google Scholar
4. Tohen M, Hennen J, Zarate CM Jr, et al: Two-year syndromal and functional recovery in 219 cases of first-episode major affective disorder with psychotic features. American Journal of Psychiatry 157:220–228, 2000Link, Google Scholar
5. Harrow M, Goldberg JF, Grossman LS, et al: Outcome in manic disorders: a naturalistic follow-up study. Archives of General Psychiatry 47:665–671, 1990Crossref, Medline, Google Scholar
6. Zarate CA Jr, Tohen M, Land M, et al: Functional impairment and cognition in bipolar disorder. Psychiatric Quarterly 71:309–329, 2000Crossref, Medline, Google Scholar
7. First MB, Spitzer RL, Gibbon M, et al: Structured Clinical Interview for DSM-IV Axis I Disorders: Patient Edition (SCID-I/P). New York, Biometrics Research, New York State Psychiatric Institute, 1998Google Scholar
8. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
9. Overall JE, Gorham DR: Brief Psychiatric Rating Scale. Psychological Reports 10:799–812, 1962Crossref, Google Scholar
10. Hamilton M: Development of a rating scale for primary depressive illness. British Journal of Social and Clinical Psychology 6:278–296, 1967Crossref, Medline, Google Scholar
11. Young RC, Biggs JT, Ziegler VE, et al: A rating scale for mania: reliability, validity, and sensitivity. British Journal of Psychiatry 133:429–435, 1978Crossref, Medline, Google Scholar
12. Randolph C: RBANS Manual: Repeatable Battery for the Assessment of Neuropsychological Status. San Antonio, Tex, Psychological Corporation (Harcourt), 1998Google Scholar
13. Wechsler D: Wechsler Adult Intelligence Scale III. San Antonio, Tex, Psychological Corp, 1997Google Scholar
14. Reitan RM: Manual for Administration of Neuropsychological Test Batteries for Adults and Children. Tucson, Ariz, 1979Google Scholar
15. Fu VK: Estimating generalized ordered logit models. Stata Technical Bulletin 44:27–30, 1988Google Scholar
16. Martinez-Aran A, Vieta E, Colom F, et al: Cognitive dysfunctions in bipolar disorder: evidence of neuropsychological disturbances. Psychotherapy and Psychosomatics 69:2–18, 2000Crossref, Medline, Google Scholar
17. Quraishi S, Frangou S: Neuropsychology of bipolar disorder: a review. Journal of Affective Disorders 72:209–226, 2000Crossref, Google Scholar
18. Tham A, Engelbrektson K, Mathe AA, et al: Impaired neuropsychological performance in euthymic patients with recurring mood disorders. Journal of Clinical Psychiatry 58:26–29, 1997Crossref, Medline, Google Scholar
19. Van Gorp WG, Altshuler L, Theberge DC, et al: Cognitive impairment in euthymic bipolar patients with and without prior alcohol dependence: a preliminary study. Archives of General Psychiatry 55:41–46, 1998Crossref, Medline, Google Scholar
20. Bell MD, Bryson G: Work rehabilitation in schizophrenia: does cognitive impairment limit improvement? Schizophrenia Bulletin 27:269–279, 2001Google Scholar
21. Bryson G, Bell MD, Kaplan E, et al: The functional consequences of memory impairments on initial work performance in people with schizophrenia. Journal of Nervous and Mental Disease 186:610–615, 1998Crossref, Medline, Google Scholar
22. Gold JM, Queern C, Iannone VN, et al: Repeatable Battery for the Assessment of Neuropsychological Status as a screening test in schizophrenia: I. sensitivity, reliability, and validity. American Journal of Psychiatry 156:1944–1950, 1999Abstract, Google Scholar
23. Gold JM, Goldberg RW, McNary SW, et al: Cognitive correlates of job tenure among patients with severe mental illness. American Journal of Psychiatry 159:1395–1402, 2002Link, Google Scholar
24. Dickerson FB, Sommerville J, Origoni AE, et al: Outpatients with schizophrenia and bipolar I disorder: do they differ in their cognitive and social functioning? Psychiatry Research 10:21–27, 2001Google Scholar
25. Hawkins KA, Hoffman RE, Quinlan DM, et al: Cognition, negative symptoms, and diagnosis: a comparison of schizophrenic, bipolar, and control samples. Journal of Neuropsychiatry and Clinical Neurosciences 9:81–89, 1997Crossref, Medline, Google Scholar
26. Hobart MP, Goldberg R, Bartko JJ, et al: Repeatable Battery for the Assessment of Neuropsychological Status as a screening test in schizophrenia: II. convergent/discriminant validity and diagnostic groups comparisons. American Journal of Psychiatry 156:1951–1957, 1999Abstract, Google Scholar
27. Green MF: What are the functional consequences of neurocognitive deficits in schizophrenia? American Journal of Psychiatry 153:321–330, 1996Google Scholar
28. Altshuler LL, Gitlin MJ, Mintz J, et al: Subsyndromal depression is associated with functional impairment in patients with bipolar disorder. Journal of Clinical Psychiatry 63:807–811, 2002Crossref, Medline, Google Scholar
29. Hammen C, Gitlin M, Altshuler L: Predictors of work adjustment in bipolar I patients: a naturalistic longitudinal follow-up. Journal of Consulting and Clinical Psychology 68:220–225, 2000Crossref, Medline, Google Scholar
30. Gitlin MJ, Swendsen J, Heller TL, et al: Relapse and impairment in bipolar disorder. American Journal of Psychiatry 152:1635–1640, 1995Link, Google Scholar
31. Solomon DA, Ristow WR, Keller MB, et al: Serum lithium levels and psychosocial function in patients with bipolar I disorder. American Journal of Psychiatry 153:1301–1307, 1996Link, Google Scholar
32. Strakowski SM, Keck PE Jr, McElroy SL, et al: Twelve-month outcome after a first hospitalization for affective psychosis. Archives of General Psychiatry 55:49–55, 1998Crossref, Medline, Google Scholar
33. Levine J, Chengappa KN, Brar JS, et al: Illness characteristics and their association with prescription patterns for bipolar I disorder. Bipolar Disorder 3:41–49, 2001Crossref, Medline, Google Scholar



