Mapping the Depressed Brain Under Stress Using Multimodal Neuroimaging
Establishing the biological signatures of human emotions, thoughts, and behavior has long been the holy grail of neuroscience research. Advancements in brain imaging and computational sciences offered an exciting opportunity to unravel the underlying mechanisms and correlates of our psyche in health and disease. Over three decades of research, neuroimaging studies provided an unprecedented insight into brain structure and function, with promising leads directly linking biomarkers to psychopathology. Unfortunately, replicating many of these brain–behavior association findings, often identified in small cohorts of a few dozen per group, has proved to be challenging. In fact, it was shown that the true effect sizes of brain–behavior associations in cross-sectional designs are much smaller than previously thought, requiring cohort sizes to be in the thousands to ensure reproducible results (1). Thus, considering the complexity of neuroimaging studies and the challenges of recruiting large cohorts of psychiatric patients, our field is contending with the dilemma of how to move forward and find the optimal approach for conducting small-sample neuroimaging studies.
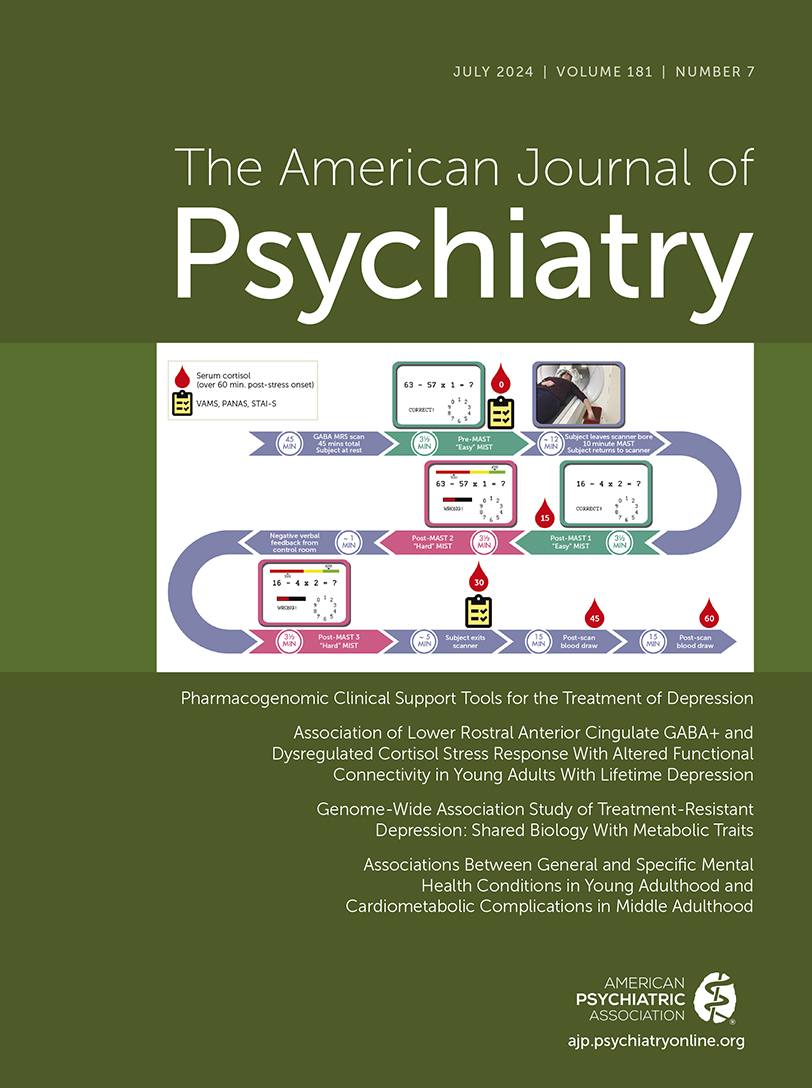
As often is the case, new challenges bring new opportunities. One futuristic approach to address this issue is to first establish foundational models of the brain using generative artificial intelligence and publicly available data repositories, and then fine-tune these models to detect a phenotype of interest in smaller cohorts. For example, BrainLM is an artificial intelligence foundational model that was established using 80,000 brain scans from the general population (2). BrainLM can now be adapted to use the knowledge acquired from the thousands to detect the brain signature of a specific behavior in a few dozen individuals. Another astute approach is to conduct multimodal experimental studies that capitalize on the higher effects of both the intervention (e.g., a task or treatment) and the within-subject gain of longitudinal design. In this issue of the Journal, Ironside and colleagues (3) provide an excellent example of an experimental design to gain new insights using a combination of multimodal neuroimaging, network modeling, and stress induction in young adults with current major depressive disorder (MDD) or remitted MDD (rMDD) and healthy control subjects. The study included a total of 130 participants across the three groups (44 with current MDD, 42 with rMDD, and 44 healthy control subjects). While this sample size may be considered modest compared with the proposed thousands of participants needed for robust brain–behavior associations in cross-sectional designs (1), the study’s multimodal approach and experimental design help to mitigate some of the challenges of smaller sample sizes. By integrating multiple biological levels of analysis, the study sheds new light on how disruptions in cortisol signaling, GABA levels, and large-scale brain network dynamics may contribute to maladaptive stress responses in depression.
Compared with the control group, both the MDD and rMDD groups showed lower levels of the inhibitory neurotransmitter GABA in the rostral anterior cingulate cortex (rACC), a key hub for emotion regulation and top-down control of limbic regions (4). This reduction in GABA was accompanied by altered activation and connectivity patterns in three core intrinsic brain networks implicated in depression and stress pathophysiology (5, 6). Specifically, depressed participants exhibited reduced activation of the frontoparietal control network (FPN), which is involved in cognitive control and emotion regulation, along with heightened engagement of the threat-sensitive salience network (SN) and the internally focused default mode network (DMN). This finding of increased DMN engagement aligns with a substantial body of research implicating DMN hyperactivity in MDD (7, 8). This pattern points to excessive rumination and maladaptive self-referential processing, which are key features of depression. Interestingly, stress reduces DMN connectivity in posttraumatic stress disorder (PTSD)—a disorder of chronic stress (9). This divergence suggests that distinct neural mechanisms may underlie maladaptive internal states in different stress-related psychopathologies, a finding that may hold potential in differentiating between specific conditions.
Critically, these aberrations in neural network function were coupled with distinct profiles of peripheral stress hormone reactivity. Individuals with current MDD exhibited a blunted cortisol response to acute psychosocial stress, whereas those with rMDD showed increased cortisol levels relative to control subjects. Furthermore, the positive coupling between cortisol and connectivity of the FPN and amygdala-related networks typically seen in healthy participants was absent or reversed in the clinical groups. Together, these findings provide a rich picture of the disturbances in inhibitory neurotransmission, neuroendocrine signaling, and large-scale brain network function that characterize the depressed brain under stress.
The deficit in rACC GABA emerged as a shared feature of both current and remitted MDD, implying a trait-like downregulation of cortical inhibition that could promote overactivity in limbic regions involved in threat reactivity and self-referential processing. Interestingly, rACC GABA levels were linked to the degree of decoupling between the SN and DMN following stress in control subjects but not patients. This suggests a key role for GABA in the adaptive reconfiguration of these depression-relevant networks in the healthy brain and points to a breakdown of this mechanism in MDD.
The opposing profiles of cortisol hypoactivity in acute MDD and hyperactivity in rMDD are also noteworthy, as they suggest distinct neuroendocrine mechanisms at different stages of the illness. Disentangling the mechanisms will require longitudinal studies that track changes in stress hormone profiles and brain network function over the course of MDD and into recovery.
Another intriguing aspect of the study was the evidence for sex differences in stress reactivity and neural network dynamics. Compared with females, males showed heightened cortisol levels and less suppression of the DMN under stress. While preliminary, these results highlight the need to consider sex-dependent vulnerabilities in the physiological and neural regulation of stress as a potential contributor to the well-established sex differences in depression prevalence. An important challenge for future research will be to unpack how these sex differences emerge over development and interact with sociocultural factors to shape depression risk across the lifespan.
The study by Ironside et al. sets the stage for several exciting translational applications. First, the findings suggest that rACC GABA levels and stress-induced patterns of frontolimbic connectivity could serve as promising biomarkers for identifying at-risk individuals and predicting clinical outcomes. Second, they reinforce the hypothesis that the anterior cingulate cortex is a key target for novel interventions, aimed at restoring inhibitory control over limbic and salience networks (10). Third, they provide a plausible mechanism for a new class of antidepressant GABA modulators—restoring inhibitory control and recalibrating frontolimbic circuits in depression (11). Examining the impact of existing antidepressant drugs and behavioral interventions on these neurochemical and circuit-level abnormalities could also yield valuable mechanistic insights and identify predictors of treatment response. More broadly, the study highlights the power of multimodal neuroimaging combined with carefully designed stress challenge paradigms for probing the neural underpinnings of emotional dysregulation across the spectrum of internalizing disorders. Extending this approach to other conditions marked by altered stress reactivity, such as anxiety disorders and PTSD, could help elucidate common and distinct pathophysiological processes and identify transdiagnostic targets for prevention and treatment.
Despite the general concerns about utility and reproducibility of cross-sectional small neuroimaging studies, the work by Ironside and colleagues capitalizes on the strength of the multimodal and experimental design to advance our mechanistic understanding of how perturbations in GABA signaling, hypothalamic-pituitary-adrenal axis function, and large-scale brain network dynamics contribute to the maladaptive stress response in depression. By demonstrating impairments in rACC GABA and top-down frontolimbic circuit function coupled with distinct profiles of neuroendocrine dysregulation in current versus remitted MDD, the study charts a promising course for neurobiologically informed approaches to the diagnosis and treatment of mood disorders. As we look to the future of psychiatric neuroscience, comparable approaches that combine a compelling theoretical framework with cutting-edge methodologies will be essential for improving our understanding of the stressed brain and for developing a new generation of more precise and effective interventions for depression and related disorders.
1. : Reproducible brain-wide association studies require thousands of individuals. Nature 2022; 603:654–660Crossref, Medline, Google Scholar
2. : BrainLM: a foundation model for brain activity recordings. BioRxiv, January 13, 2024 (https://doi.org/10.1101/2023.09.12.557460) Google Scholar
3. : Association of lower rostral anterior cingulate GABA+ and dysregulated cortisol stress response with altered functional connectivity in young adults with lifetime depression: a multimodal imaging investigation of trait and state effects. Am J Psychiatry 2024; 181:639–650Abstract, Google Scholar
4. : The neural bases of emotion regulation. Nat Rev Neurosci 2015; 16:693–700Crossref, Medline, Google Scholar
5. : Specific alterations of resting-state functional connectivity in the triple network related to comorbid anxiety in major depressive disorder. Eur J Neurosci 2024; 59:1819–1832Crossref, Medline, Google Scholar
6. : A network-based neurobiological model of PTSD: evidence from structural and functional neuroimaging studies. Curr Psychiatry Rep 2017; 19:81Crossref, Medline, Google Scholar
7. : All roads lead to the default-mode network: global source of DMN abnormalities in major depressive disorder. Neuropsychopharmacology 2020; 45:2058–2069Crossref, Medline, Google Scholar
8. : Resting-state functional connectivity in major depressive disorder: a review. Neurosci Biobehav Rev 2015; 56:330–344Crossref, Medline, Google Scholar
9. : Default mode network abnormalities in posttraumatic stress disorder: a novel network-restricted topology approach. Neuroimage 2018; 176:489–498Crossref, Medline, Google Scholar
10. : Cingulate dynamics track depression recovery with deep brain stimulation. Nature 2023; 622:130–138Crossref, Medline, Google Scholar
11. : Understanding the mechanism of action and clinical effects of neuroactive steroids and GABAergic compounds in major depressive disorder. Transl Psychiatry 2023; 13:228Crossref, Medline, Google Scholar