Early-life Adversity and Genetics Associated With the Risk to Develop Psychiatric Illnesses
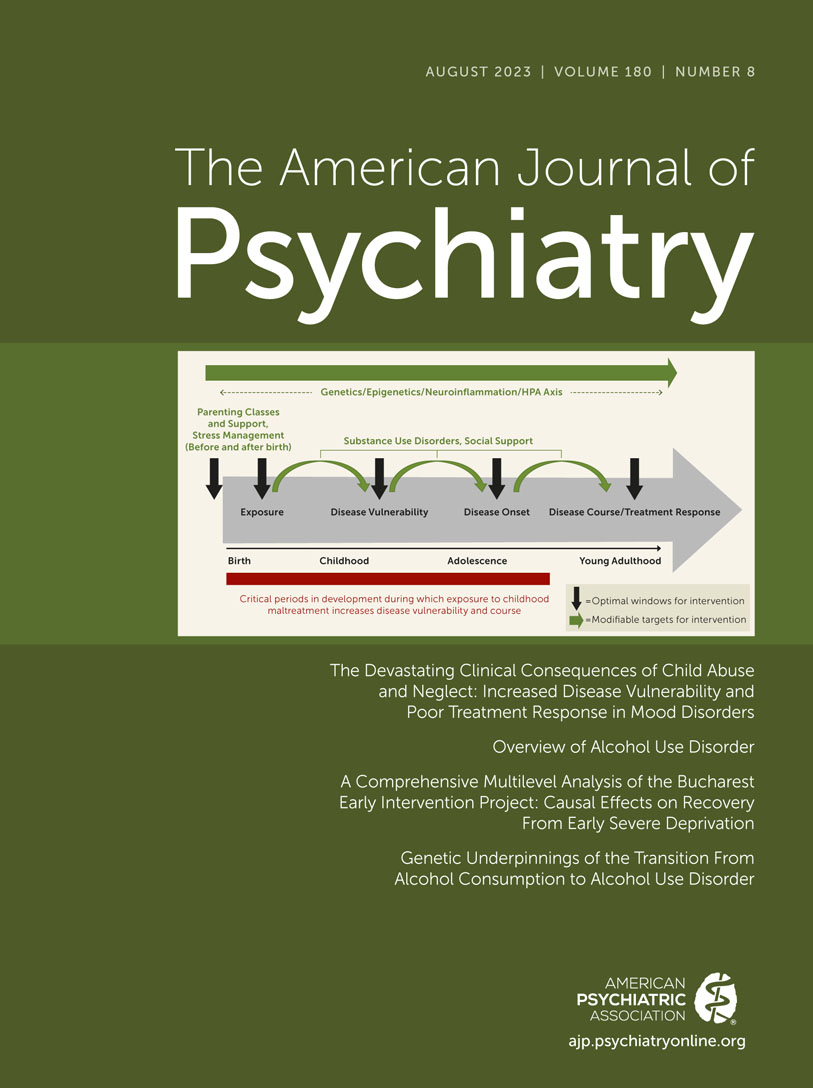
The factors that determine the risk for most psychiatric disorders are present early in life even though the symptoms of these disorders may not emerge until later childhood, adolescence, or adulthood. This issue of the Journal pursues this neurodevelopmental theme by focusing on early-life factors that confer the risk for the later development of psychopathology. We begin the issue by revisiting two previously published overviews that are highly relevant for this issue. The first of these reviews advances in developmental neuroscience as they relate to understanding childhood psychopathology. The second is focused on the impact of childhood maltreatment on the vulnerability to develop depression and how a history of maltreatment relates to treatment response. These overviews are accompanied by a new overview that provides an update on alcohol use disorder. In line with these overviews, another important paper in this issue examines and compares the genetics underlying alcohol use with that of alcohol use disorder. Complementing the overviews on developmental neuroscience and the consequences of childhood neglect and abuse, we also include a very meaningful paper that demonstrates the long-term efficacy of a family-based intervention on IQ and psychopathology in orphaned Romanian children.
Developmental Neuroscience, Early-Life Trauma, the Risk of Developing Psychopathology, Including Alcohol Use Disorder
Two overviews in this issue integrate the most recent findings that link preclinical neuroscience research to clinical issues focused on early-life trauma and neglect. Drs. Heidi Meyer and Francis Lee from Cornell University present a framework to understand how the maturation of specific brain circuits relates to normal development as well as the risk to develop various psychiatric illnesses (1). More specifically, they discuss the childhood development of fear, threat responses, and motivated responding and how early-life stress can alter the development of the circuitry underlying these responses. Drs. Elizabeth Lippard and Charles Nemeroff from the University of Texas at Austin review the literature associating childhood maltreatment with the risk to develop mood disorders (2). In addition to linking maltreatment to more severe and difficult to treat depressive episodes, the authors discuss potential hypothalamic-pituitary-adrenal axis and inflammatory cytokine mechanisms mediating the effects of early-life neglect.
We also include a new overview in this issue on alcohol use disorder that is authored by Dr. Henry Kranzler from the University of Pennsylvania (3). In addition to discussing the demographics, neurobiology, and etiology of alcohol use disorder, this overview includes a helpful review of current treatment strategies.
Mitigating the Effects of Early Neglect and Deprivation on Orphaned Romanian Infants
Neglect is a common form of early adversity that has major negative consequences on children’s physical, cognitive, and emotional development. In his early nonhuman primate studies, Harry Harlow (4) provided important insights into the social mechanisms underlying the effects of neglect by identifying social support and physical contact, in the form of what he termed “contact comfort,” as being critical for normal social and emotional development. While considerable work has been performed studying neglected children, and many other papers have been published from the Romanian sample used in this study, King et al. (5) report on the long-term, longitudinal follow-up of individuals that participated in the Bucharest Early Intervention Project. This unique and highly valuable project began in 2001 and was designed as a randomized controlled trial to assess the effects of foster care versus ongoing institutional care for children in Bucharest, Romania who had been abandoned and placed in orphanages. While the physical needs of these orphaned children were met, due to various factors the children in these orphanages suffered from social neglect. The clinical trial involved 136 children, 68 who remained in orphanages, and 68 children who were raised in high-quality foster care settings. The children that received foster care were placed in their foster families at an average of 22.6 months of age. Assessments in the children were performed repeatedly up to the ages of 16–18 and consisted of IQ, growth, psychopathology, and relative EEG alpha wave power. Results demonstrated, across the multiple assessments, that foster care had significant positive effects on enhancing IQ and physical growth and in reducing psychopathology. More specifically, in relation to psychopathology, the children in the foster care group had significantly fewer symptoms associated with attachment disorders (e.g., reactive attachment disorder, disinhibited social engagement disorder) and internalizing disorders but did not significantly differ from the children that remained in the orphanages in symptoms related to externalizing disorders. In general, within the foster care group the children that remained with their original foster family tended to have better outcomes. In her editorial (6), Dr. Helen Minnis from the University of Glasgow provides her perspective on this study and emphasizes its importance in promoting change at a policy level, which has resulted in a substantial improvement in the well-being of Romanian children who have lost their parents.
Understanding the Genetics of Alcohol Use and Alcohol Use Disorder
Why do some individuals who drink alcohol ultimately develop alcohol use disorder (AUD) while others can maintain a level of alcohol consumption that does not progress to AUD? Kember et al. (7) address this question from a genetics perspective by using genomic data from 409,630 individuals in the Million Veterans Project. Importantly, this sample was constituted with a reasonable number of non-White participants that included 80,764 African American individuals and 31,877 Hispanic American individuals. And the analyses that were performed were across all individuals, as well as specifically in relation to one’s ancestry. Alcohol use was assessed with the Alcohol Use Disorders Identification Test (AUDIT-C), and alcohol use disorder diagnoses, which were attributed to 24.7% of the participants, were classified from the electronic health record using the International Classification of Disease criteria. Overall, the GWAS studies found 26 genetic variants that were associated with AUD and some variants that were ancestry-specific. In relation to alcohol consumption, 24 variants were identified and again some variants were found to be ancestry-specific. It is important to note that novel genetic variants were identified that were associated with both alcohol consumption and AUD. Also of importance, the analyses revealed that some genetic variants appeared to statistically mediate the relation between alcohol consumption and AUD, whereas 12 variants were identified that were independently associated with AUD and not one’s level of alcohol consumption. Genetic correlations were also performed that showed considerable relatedness between the genetics of consumption and disorder and between European Americans and African Americans. It is noteworthy that these correlations were higher when the analyses were performed by leaving out individuals that were alcohol abstainers. While there is much that is shared between alcohol consumption and AUD, the authors point out that their data also demonstrate some important differences in the genetics underlying alcohol consumption versus AUD. The authors also suggest novel molecular targets that may be relevant to developing new interventions aimed at preventing the transition from alcohol use to disorder. Dr. Julie White from Research Triangle Institute International and Dr. Laura Beirut from Washington University School of Medicine contribute an editorial (8) that delves into the findings and presents data from other studies examining genetic correlations. They argue that what is shared between alcohol consumption and AUD is more robust than what differs.
Conclusions
Most psychiatric disorders are neurodevelopmental in nature, with genetic predispositions and early experiences setting the stage for one’s vulnerability or resilience. This issue of the Journal, on the neurodevelopmental origins of psychopathology, is focused on early-life adversity and genetics as mediators of the risk to develop psychiatric illnesses. For many disorders that emerge during childhood (e.g., autism and ADHD), neurodevelopmental mechanisms are clear, whereas this may not be so obvious for disorders that have their onset later in adulthood. Schizophrenia is a prime example of this, as the major symptoms of schizophrenia typically emerge in late adolescence or early adulthood, and yet considerable research provides convincing evidence linking the risk to develop schizophrenia to aberrant in utero and early neonatal cortical and neural pathway development.
The major points to take away from the papers in this issue include: 1) the worldwide and astounding prevalence of neglected and traumatized children and how this early-life adversity interacts with developing neural systems to increase the risk to develop depression via altered maturation of neural, endocrine, and immune systems; 2) empirical data supporting early family-based interventions to alleviate the effects of childhood social neglect; an important example of how relevant research data can inform policy change; 3) maladaptive alcohol use is highly prevalent, and alcohol use disorder is markedly undertreated despite evidence based pharmacological and psychosocial treatments; and 4) insights into how the genetics of alcohol use are similar to, and differ from, those of alcohol use disorder.
The papers in this issue of the Journal, in addition to providing important new insights, are a reminder of the necessity to deepen our understanding of the interactions between genetic and environmental neurodevelopmental factors that predispose to psychiatric illnesses. Such research is fundamental to achieving the goal of identifying high-risk individuals who will benefit from novel interventions aimed at critical neurodevelopmental processes.
1. : Translating developmental neuroscience to understand risk for psychiatric disorders. Am J Psychiatry 2023; 180:540–547Abstract, Google Scholar
2. : The devastating clinical consequences of child abuse and neglect: increased disease vulnerability and poor treatment response in mood disorders. Am J Psychiatry 2023; 180:548–564Abstract, Google Scholar
3. : Overview of alcohol use disorder. Am J Psychiatry 2023; 180:565–572Abstract, Google Scholar
4. : The nature of love. Am Psychol 1958; 13:673–685Crossref, Google Scholar
5. : A comprehensive multilevel analysis of the Bucharest early intervention project: causal effects on recovery from early severe deprivation. Am J Psychiatry 2023; 180:573–583Link, Google Scholar
6. : Science into policy for the benefit of children: the Bucharest early intervention project. Am J Psychiatry 2023; 180:528–529Abstract, Google Scholar
7. : Genetic underpinnings of the transition from alcohol consumption to alcohol use disorder: shared and unique genetic architectures in a cross-ancestry sample. Am J Psychiatry 2023; 180:584–593Abstract, Google Scholar
8. : Alcohol consumption and alcohol use disorder: exposing an increasingly shared genetic architecture. Am J Psychiatry 2023; 180:530–532Abstract, Google Scholar