Focusing on Substance Use Disorders, Opioids, and Craving
Maladaptive substance use and substance use disorders are highly comorbid with psychiatric illnesses and are frequently associated with the onset and/or exacerbation of these illnesses. This issue of the Journal is focused on substance use disorders and how they relate to psychiatric illnesses, providing new insights into their diagnosis and treatment. The toll that opioid misuse has taken on our society is immeasurable and, in this regard, three papers in this issue address topics important for treating patients with opioid use disorder. First, Drs. Carlos Blanco and Nora Volkow (1) from the National Institute on Drug Abuse provide an overview updating us on current treatments for this disorder. This overview is accompanied in this issue by a study that addresses the association between prescribed opiates and suicide at a regional level within the United States and another study demonstrating the value of using performance-based measurements to aid in the treatment of opioid use disorder.
An extremely important concern related to the management of individuals with substance use disorders is the significant racial and ethnic disparities that exist in the diagnosis and treatment of these disorders. To this point, in this issue we include a study that highlights such disparities in the care of veterans with alcohol use disorder by examining racial and ethnic differences in how self-reports of alcohol use relate to receiving the diagnosis of alcohol use disorder. Another study uses data from a very large sample to explore the complex relation between maladaptive substance use and psychiatric illnesses in which the authors determined the risk to develop bipolar disorder and schizophrenia spectrum disorder after individuals experience episodes of substance-induced psychosis. An additional study in this issue investigates the neural correlates of craving, a psychological process that is fundamentally related to addiction. By using machine learning with resting-state functional connectivity data, the authors demonstrate the ability to predict individual differences in subjective ratings of craving.
The Relation Between Prescribed Opiates and Suicide Deaths
Over the past several years, health care systems and providers have made it a goal to decrease the number of opioid prescriptions, with the hope that this would result in a decline in the incidence of opioid abuse and deaths related to opioid overdose. Olfson and colleagues (2) present regional data from the United States that was collected from 2009–2017 to assess whether such efforts have been effective. Data for this study came from different sources, with the opioid prescription data coming from IQVIA Real World Prescription Database. Analyses were designed to assess effects at a regional level by using the 886 commuting zones within the United States. Commuting zones are defined as being related to travel-work areas and usually are regions that are constituted by adjacent counties. Opioid prescription patterns were characterized by 1) number of prescriptions filled per individual, 2) percent with ≥1 prescription per year, 3) percent with ≥1 prescription per year receiving a high dose of over 120 mg morphine equivalents, 4) percent with long-term (≥60 days) prescriptions, and 5) percent receiving prescriptions from multiple providers (≥3 per year). Opioid prescribing, as reflected in the above metrics, decreased from 2009–2017 and importantly, at a regional level, opioid prescribing was predictive of overall suicides as well as opioid-related suicides. However, the data also demonstrated that at the younger age range, 10- to 44-year-olds, reductions in opioid prescriptions were associated with increases in opioid deaths that were not attributed to suicide. In their editorial, Drs. Jenna McCauley and Kathleen Brady (3) from the Medical University of South Carolina discuss the importance of this study emphasizing an analytic strategy that is focused on the regional level and other factors associated with prescribing levels that may be contributing to the findings reported by Olfson and colleagues. They also explore explanations for the counterintuitive findings reported for the younger age group.
Using Performance-Based Assessments to Evaluate Opioid Use Disorder Treatment Outcomes
Williams et al. (4) use electronic medical record data from a multisite opioid use disorder buprenorphine maintenance treatment program to understand the extent to which performance measures endorsed by the Centers for Medicare and Medicaid Services (CMS) are helpful in predicting treatment outcomes. The primary performance measure used was aimed at assessing initial engagement in treatment—the Health Effectiveness and Data Information Set (HEDIS) measure of Engagement of Alcohol and Other Drug Abuse or Dependence Treatment. This measure defines treatment engagement as having two outpatient visits or other professional interactions within 34 days of an initial intake. A National Quality Forum (NQF) metric for medication treatment for opioid use disorder was used to assess treatment retention, which defines retention as continuous treatment for a minimum of 6 months. Of the 19,487 patients followed, 82.4% engaged in care as defined by the HEDIS definition of engagement. Of patients that engaged in care, 47% were retained in treatment when assessed at 6 months, whereas only 2.9% of individuals that did not successfully initially engage in treatment remained in care at 6 months. 31.8% of individuals that initially engaged in treatment were still being treated at the 1-year follow-up, compared to 1.2% of individuals that did not successfully initially engage in treatment. Interestingly, individuals that tested positive for cocaine or had hepatitis C at entry were less likely to be retained in treatment. These data demonstrate the value of using performance-based measures to assess medication treatment outcomes for opioid use disorder, and, not surprisingly, show that initial treatment engagement is critical in determining successful outcomes.
Assessing Biases in Diagnosing Alcohol Use Disorder Among Black, Hispanic, and White Veterans
Biases in diagnosing and treating patients exist throughout medicine resulting in inequities in health care, the most important of which may be related to treatment access, treatment selection, and treatment outcomes. Using data from the Million Veteran Program sample, Vickers-Smith and colleagues (5) address the question as to whether racial and ethnic biases can account for the increased prevalence of alcohol use disorder diagnoses observed in Black and Hispanic veterans as compared to White veterans. In this regard, data from 739,411 veterans was used to compare self-reported alcohol use, assessed with the Alcohol Use Disorders Identification Test—Consumption (AUDIT-C), with clinical diagnoses obtained from VA medical records. The sample was largely constituted of males, 91%, and to assess sex differences in relation to potential biases, data from males and females were analyzed separately. The data demonstrated that with similar amounts of self-reported alcohol use, Black and Hispanic veterans were more likely than White veterans to be diagnosed with alcohol use disorder. While the results varied somewhat in relation to the amount of drinking individuals engaged in, the most dramatic discrepancies were found at levels of reported drinking indicative of unhealthy alcohol use. For example, at this level of alcohol intake, White male veterans were 1/3 less likely than Black male veterans to receive a diagnosis of alcohol use disorder. The results indicated similar discrepancies between reported alcohol use and alcohol use disorder diagnoses for Black female veterans compared to White female veterans. These findings remained significant when controlling for other variables that might influence the effect. Taken together, these findings point to, and uncover, racial and ethnic biases experienced by veterans when being assessed for alcohol use and when receiving a diagnosis of alcohol use disorder. Drs. Karen Abram, María Luna, and Linda Teplin from Northwestern University (6) contribute an editorial that underscores the general importance of understanding racial and ethnic biases in medicine, specifically addresses methodological issues in this study, and provides a brief literature review related to racial and ethnic biases in psychiatric diagnoses.
From Substance-Induced Psychosis to Schizophrenia Spectrum Disorder or Bipolar Disorder
It is well known that persistent and excessive use of various substances can be associated with the later development of psychiatric illnesses, especially psychotic disorders. Rognli and colleagues (7) use a large database from the Norwegian Patient Registry to assess the likelihood of conversion to schizophrenia spectrum disorder or bipolar disorder after experiencing a substance-induced psychosis. More specifically, this database is used to understand the risk to develop schizophrenia spectrum or bipolar disorder that is associated with different types of substance-induced psychoses as well as other factors, such as gender and age, that may add to this risk. The investigators identified 3,187 individuals with the diagnosis of substance-induced psychosis, from the 2010–2015 registry database of all psychiatric patients. 14.2% of individuals had alcohol-induced psychosis, 17.6% cannabis-induced psychosis, 22% amphetamines-induced psychosis, and 38.8% multiple substance-induced psychosis. 636 individuals with a history of substance-induced psychosis later developed schizophrenia spectrum disorder, with a median time interval between substance-induced psychosis and schizophrenia spectrum disorder of 9.6 months. Cannabis-induced psychosis was associated with the greatest risk, whereas alcohol-induced psychosis was associated with the lowest risk. The overall estimated cumulative 6-year risk of developing schizophrenia spectrum disorder after an episode of substance-induced psychosis was 27.6% and the greatest risk was associated with cannabis-induced psychosis (36% conversion rate). In general, younger men with substance-induced psychoses were found to be at greatest risk to develop schizophrenia spectrum disorders and in both men and women more substance-induced psychoses emergency room admissions conferred increased risk. Considerably fewer individuals (N=100) went on to develop bipolar disorder, with a median time interval of 1 year. Females with prior substance-induced psychoses were at greater risk than males with an overall 6-year cumulative risk for males and females of 4.5%. Together, these data help understand the magnitude of the association between substance-induced psychosis and the later development of schizophrenia spectrum disorder and bipolar disorder. However, it is important to emphasize that the data do not speak to causality, as many other factors may account for the associations between substance-induced psychoses and these illnesses. In his editorial, Dr. Evangelos Vassos from King’s College London (8) addresses the issue of causality and based on the high conversion rate to psychosis, emphasizes the need for early interventions in individuals experiencing substance-induced psychoses.
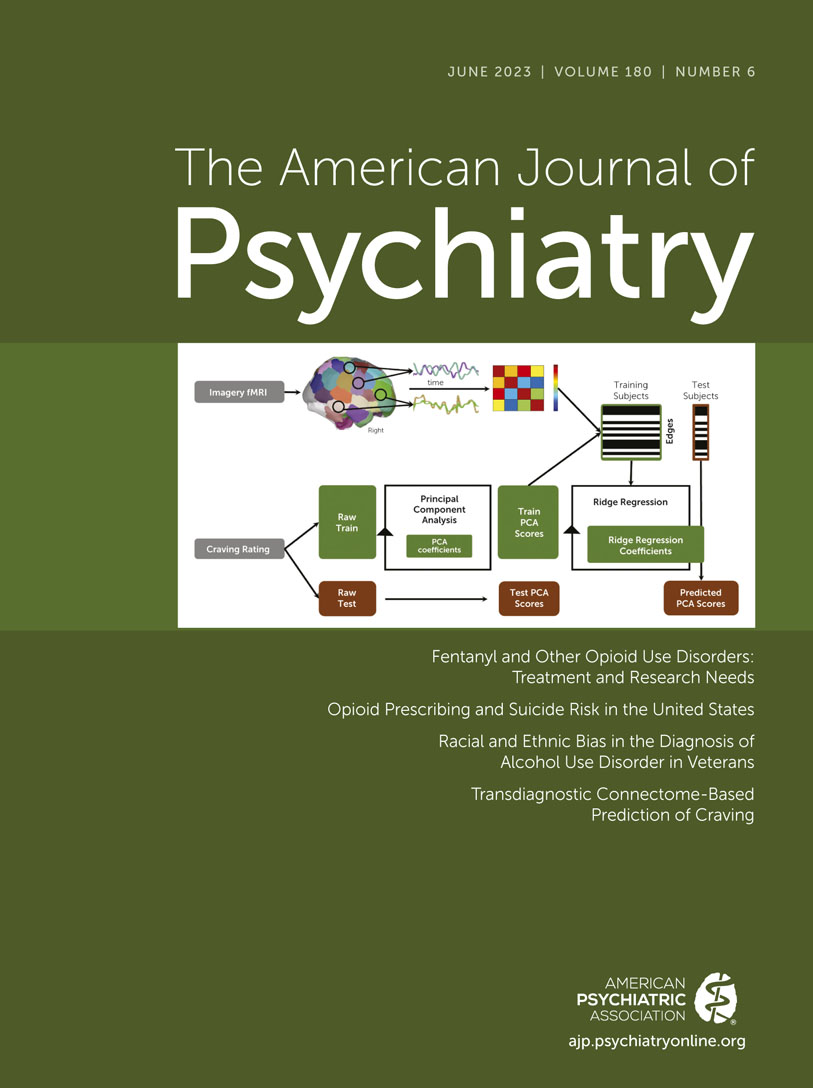
Identifying a Neural Network Associated With Craving
Craving, a state of mind that is related to appetitive drives and enhanced by deprivation, is a common experience and most of the time not pathological. However, when excessive, craving can be associated with maladaptive behaviors and, in many cases, this is associated with psychopathology. Substance use disorders and eating disorders are prime examples of how maladaptive craving can drive and reinforce harmful behaviors. To better understand the neural underpinnings of craving, Garrison et al. (9) present data that uses a machine learning approach called connectome-based predictive modeling to analyze functional MRI data from 274 individuals. The sample studied included normal individuals as well as individuals with cocaine or alcohol use disorders, users of cocaine or alcohol, and adolescents who were prenatally exposed to cocaine. Imaging data were acquired concomitantly with subjective ratings of craving when participants were exposed to six different personalized guided imagery scripts: two designed to activate appetitive processes associated with ones’ favorite food or drug, two related to stressors, and two others that were neutral or relaxing. The machine learning strategy used derived a model in which the imaging data significantly predicted individual differences in craving measures. The so called “craving network” involved numerous brain regions, with the default mode network appearing to make the most robust contributions. The findings also highlighted involvement of motor-sensory, visual, and subcortical networks. To confirm the reliability of the findings, the researchers used data from an independent sample of 32 control participants who were imaged with a different task before and after a 10 hour fast. These results demonstrated that individual differences in the previously characterized “craving network” predicted deprivation-related measures of food craving. In their editorial, Anna Konova and Emma M. Schweitzer from Rutgers University (10) provide an in-depth discussion of the paper focusing on the methods, the magnitude of the findings, and their implications for clinical treatment.
Conclusions
This issue of the Journal is focused on opiate use disorders as well as other substance use disorders and their interactions with psychiatric illnesses. The major findings from the papers in this issue include: 1) an overview on current and future treatments for opiate use disorder; 2) demonstrating, at a regional level within the United States, that a reduction in the number of opiate prescriptions is predictive of decreases in opioid-related suicides as well as overall suicides; 3) the value of performance-based measures in the medical management of individuals with opioid use disorders; 4) evidence for racial/ethnic biases in the diagnosis and treatment of veterans with alcohol use disorder; 5) the risk to develop schizophrenia spectrum disorders or bipolar disorder in relation to prior episodes of substance-induced psychoses; and 6) characterization of a neural signature that is predictive of individual differences in subjective assessments of craving.
In addition to the informative findings provided by these papers, it is important to recognize that substance use disorders are highly comorbid with psychiatric disorders and that the care of individuals with these comorbidities is often fragmented. From a clinical perspective, the first step is to accurately diagnose and document maladaptive substance use in relation to psychiatric illnesses. This then should be followed by a comprehensive treatment strategy aimed at concurrently targeting substance use and psychiatric issues and importantly focusing on their deleterious interactions.
1. : Fentanyl and other opioid use disorders: treatment and research needs. Am J Psychiatry 2023; 180:410–417 Abstract, Google Scholar
2. : Opioid prescribing and suicide risk in the United States. Am J Psychiatry 2023; 180:418–425Abstract, Google Scholar
3. : Association between opioid prescribing and suicide risk in the United States. Am J Psychiatry 2023; 180:400–401 Abstract, Google Scholar
4. : Performance measurement for opioid use disorder medication treatment and care retention. Am J Psychiatry 2023; 180:454–457Link, Google Scholar
5. : Racial and ethnic bias in the diagnosis of alcohol use disorder in veterans. Am J Psychiatry 2023; 180:426–436 Link, Google Scholar
6. : Racial and ethnic biases and psychiatric misdiagnoses: toward more equitable diagnosis and treatment. Am J Psychiatry 2023; 180:402–403 Abstract, Google Scholar
7. : Transition from substance-induced psychosis to schizophrenia spectrum disorder or bipolar disorder. Am J Psychiatry 2023; 180:437–444 Link, Google Scholar
8. : What is the link between substance-induced psychosis and primary psychotic disorders? Am J Psychiatry 2023; 180:404–406 Abstract, Google Scholar
9. : Transdiagnostic connectome-based prediction of craving. Am J Psychiatry 2023; 180:445–453 Abstract, Google Scholar
10. : Decoding craving: insights from a brain-based connectome predictive model of subjective reports. Am J Psychiatry 2023; 180:407–409 Abstract, Google Scholar