Thyroid Hormone Levels and Recurrence of Major Depression
Abstract
OBJECTIVE: The relationship between basal thyroid hormone levels and acute antidepressant response has been studied, but any relationship between basal thyroid hormone levels and long-term course of depressive illness has not been evaluated. METHOD: The authors used a Cox regression survival analysis to evaluate the relationship between life course of depressive illness and basal levels of thyroid hormones (triiodothyronine [T3], thyroxine [T4,], and thyrotropin) in 75 outpatients with unipolar major depressive disorder. RESULTS: Time to recurrence of major depression was inversely related to T3 levels but not to T4 levels. CONCLUSIONS: These data may be of clinical interest in view of the fact that T3 is used to augment antidepressant response.
It is generally accepted that unipolar major depression tends to run a chronic or recurrent course (1–3). Although clinical (1–3) and biological (4, 5) predictors of episode recurrence have been identified, the mechanism remains poorly understood.
Thyroid hormones have been extensively studied in major depressive illness. It is well established that thyroxine (T4) levels are higher in treatment responders (6) and decrease with antidepressant response (7) but are not associated with degree of treatment resistance. Studies of thyroid hormones in major depression have largely been confined to acute episodes and not to the long-term course, although it has been shown that perturbations of the thyroid axis may influence the course of illness in bipolar disorder (8). Therefore, we studied the relationship between basal thyroid hormone levels and recurrence of illness in a group of patients with unipolar depression.
Method
Seventy-five outpatients (25 men and 50 women) whose mean age was 37.9 years (SD=11.3) gave written and oral consent to be included in a database of subjects treated under usual clinical conditions. All had a diagnosis of nonpsychotic unipolar major depressive disorder, determined by using the Schedule for Affective Disorders and Schizophrenia—Lifetime Version (SADS-L) (9), a structured interview that uses Research Diagnostic Criteria (RDC) (10). All subjects had a minimum score of 16 on the 17-item Hamilton Rating Scale for Depression (11) at study entry. At that time, blood was drawn for measurement of T4 and triiodothyronine (T3) by standard radioimmunoassays and for measurement of thyrotropin (TSH) by ultrasensitive assay.
Patients were treated by clinician choice and were evaluated in the clinic at 1–3-month intervals. Response to treatment was defined as the absence of an RDC-defined major depressive episode and a score of 1 or 2 on a 5-point clinical global improvement scale (1=remission, 2=marked improvement, 3=moderate improvement, 4=minimal improvement, 5=no response). Recurrence was defined as follows: 1) stable response for a minimum of 2 months, 2) occurrence of RDC-defined major depressive episodes determined by the SADS-L, and 3) need for further treatment intervention and/or hospitalization.
Thyroid hormone levels were collected at the beginning of the index episode just before antidepressant treatment was given and were recorded separate from course of illness data. The study period extended over a 10-year period; patients were followed as long as possible or until recurrence. Data were analyzed by using Cox regression survival analysis, with each thyroid hormone (T4, T3, and TSH), comorbid anxiety, sex, age, duration of current episode, duration of illness, and number of previous episodes entered as covariates. A stepwise method was used with an inclusion value of p<0.05 and a removal value of p>0.10.
Results
The survival curve for the study group (including positions of “censored” cases; i.e., patients who had not suffered a recurrence by the end of the study period) is shown in Figure 1. The significant positive predictors of recurrence were presence of comorbid anxiety (Wald χ2=21.6, df=1, p<0.0001), higher numbers of previous episodes (Wald χ2=7.0, df=1, p<0.01), and increased durations of current episodes (Wald χ2=5.3, df=1, p<0.03). Furthermore, T3 was significantly related to recurrence (Wald χ2=43, df=1, p<0.04) but T4 was not. Specifically, each 0.10-μg increase in T3 level was associated with a 22% decrease in risk of recurrence.
Discussion
In addition to well-described predictors of recurrence in unipolar depression, such as number of previous episodes, duration of current episode, and comorbidity (1–3), we found that serum T3 levels but not T4 levels were inversely related to time to recurrence of a depressive episode. Our data are of interest because T3 is more commonly used to augment antidepressant response (reviewed in reference 7), suggesting that elevation of T3 levels in the circulation and presumably in the brain may have a beneficial effect on depression.
Our study is limited by several methodological problems, including the relatively small number of subjects and the lack of precise measures of depressive symptoms. Moreover, the studies to date of T3 augmentation (reviewed in reference 7) have been of very short duration. On the basis of the findings from our study, it would be of interest to see whether long-term T3 treatment may have a beneficial effect on not only acute episodes but also the risk of future recurrence of depression.
Received Nov. 16, 1999; revision received March 15, 2000; accepted May 10, 2000. From the Mood Disorders Program and Department of Psychiatry, Faculty of Health Sciences, McMaster University. Address reprint requests to Dr. Joffe, McMaster University, 1200 Main St. West, Rm. 2E1, Hamilton, Ont., L8N 3Z5, Canada; [email protected] (e-mail).
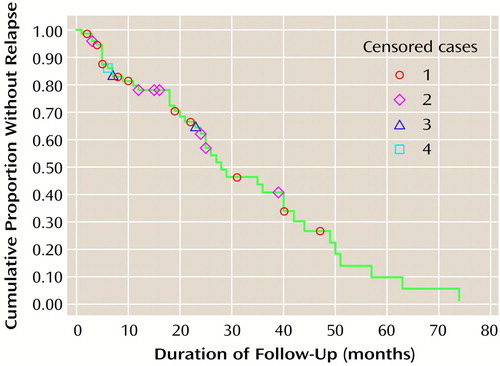
Figure 1. Survival Curve for 75 Outpatients With Unipolar Major Depressive Disorder Over 80 Months of Antidepressant Treatmenta
aPositions of “censored” cases (ie., patients who had not suffered a recurrence by the end of the study period) are shown
1. Keller MB, Klerman GL, Lavori PW, Coryell W, Endicott J, Taylor J: Long-term outcome of episodes of major depression: clinical and public health significance. JAMA 1984; 252:788–792Crossref, Medline, Google Scholar
2. Keller MB, Boland RJ: Implications of failing to achieve successful long-term maintenance treatment of recurrent unipolar major depression. Biol Psychiatry 1998; 44:348–360Crossref, Medline, Google Scholar
3. Maj M, Veltro F, Pirozzi R, Lobrace S, Magliano L: Pattern of recurrence of illness after recovery from an episode of major depression: a prospective study. Am J Psychiatry 1992; 149:795–800Link, Google Scholar
4. Arana GW, Baldessarini RJ, Ornsteen M: The dexamethasone suppression test for diagnosis and prognosis in psychiatry. Arch Gen Psychiatry 1985; 42:1193–1204Google Scholar
5. Kupfer DJ, Frank E, McEachran AB, Grochocinski VJ: Delta sleep ratio: a biological correlate of early recurrence in unipolar affective disorder. Arch Gen Psychiatry 1990; 47:1100–1105Google Scholar
6. Whybrow PC, Coppen A, Prange AJ Jr: A hypothesis of thyroid-catecholamine-receptor interaction. Arch Gen Psychiatry 1981; 38:106–113Crossref, Medline, Google Scholar
7. Joffe RT, Levitt AJ: The thyroid and depression, in The Thyroid Axis and Psychiatric Illness. Edited by Joffe RT, Levitt AJ. Washington, DC, American Psychiatric Press, 1993, pp 195–253Google Scholar
8. Cowdry RW, Wehr TA, Zis AB, Goodwin FK: Thyroid abnormalities associated with rapid-cycling bipolar illness. Arch Gen Psychiatry 1983; 40:414–420Crossref, Medline, Google Scholar
9. Spitzer RL, Endicott J: Schedule for Affective Disorders and Schizophrenia—Lifetime Version, 3rd ed. New York, New York State Psychiatric Institute, Biometrics Research, 1979Google Scholar
10. Spitzer RL, Endicott J, Robins E: Research Diagnostic Criteria: rationale and reliability. Arch Gen Psychiatry 1978; 35:773–782Crossref, Medline, Google Scholar
11. Hamilton M: A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56–62Crossref, Medline, Google Scholar