Back to the Future: Esmethadone, the (Maybe) Nonopiate Opiate, and Depression
The need for novel agents for the treatment of major depression is evidenced by the relatively low remission rates reported with all the FDA-approved antidepressants as well as after treatment with evidence-based psychotherapies such as cognitive behavior therapy (1). After a remarkable hiatus in which no new drugs with any novel mechanisms of action were approved distinct from the SSRI and SNRI classes, a veritable explosion of novel treatments has recently emerged. These include novel neuromodulation approaches such as accelerated theta burst transcranial magnetic stimulation (TMS) (2) and a host of new pharmacological approaches including the recently approved esketamine (3), which followed on a series of studies of intravenously administered ketamine in treatment-resistant depression (4). A number of ketamine-like compounds are being developed with the goal of a more optimal safety and efficacy profile. Moreover, much attention recently has been focused on psilocybin and related compounds, with much publicity surrounding the initial results in patients with major depression (5). Other findings of great interest are the approval of the neurosteroid brexanolone for the treatment of postpartum depression and the recent studies of the oral formulation of zuranolone (6), in part exciting because like ketamine and accelerated theta burst TMS, many responders apparently have an extended response that persists for weeks after completion of the active treatment period. There are also novel combination drug therapies under investigation that are currently being evaluated by the FDA including dextromethorphan/bupropion (7).
In this issue of the Journal, Fava and colleagues report that 1 week of treatment with d-methadone (esmethadone) studied in a placebo-controlled, double-blind, randomized inpatient clinical trial of treatment-resistant patients with major depression exhibited clear efficacy at day 4, 7, and 14 (7 days after the last dose) (8). d-Methadone is described as the opioid inactive isomer of racemic methadone that acts primarily as a low-affinity, low-potency NMDA receptor antagonist, although it has micromolar affinity for the serotonin and norepinephrine transporters. The patients were maintained on their stable regimen of antidepressants and were randomized to 25 or 50 mg of esmethadone. A total of 62 patients were enrolled and randomized in the study, and 57 completed the study, rendering approximately 20 patients per treatment arm. Both doses of esmethadone exhibited evidence of antidepressant efficacy (no difference between them) with remission rates at day 14 of 31% and 36% for the low and high doses of esmethadone, respectively, compared with 5% with placebo treatment. The side effect profile was benign with no characteristic opiate effects or withdrawal after day 7.
The use of opioid agonists in the treatment of depression has a very long and noteworthy history, with both Hippocrates and Galen being prescribers of opioids for depression (9) and the “opium cure” being widely used in the latter part of the 19th century. More recently antidepressant effects of buprenorphine were reported (10). More pertinent to the present discussion are the reports of the effectiveness of methadone in treating depression among opiate addicts (11) now confirmed in a meta-analysis (12). These findings, taken together, raise a number of important issues and questions. First, it is entirely possible that the reported antidepressant effects of racemic methadone could be largely due to the effects of esmethadone. To clarify this, a comparison of the antidepressant effects of l-methadone versus d-methadone would need to be conducted, which is quite unlikely in view of the addictive properties of the former compound. Second, the hypothesis that the observed effects of esmethadone are primarily mediated by its action at the NMDA receptor is, of course, just that—a hypothesis. As reviewed by Kassenbrock et al. (13), there are currently no PET radioligands available for monitoring NMDA receptor occupancy in vivo. This severely hampers the ability to determine whether esmethadone is acting primarily at this site as well as elucidating much needed dose response relationships, as has, for example, been demonstrated with antipsychotic drugs and the D2 and 5-HT2A receptors. Third is the issue of whether esmethadone is devoid of opiate activity. In the company press release of July 27, 2021 (14) a study comparing “likeability” of esmethadone compared with oxycodone in recreational opioid users addressed the effects of three doses of esmethadone (25, 75, and 150 mg) compared with oxycodone 40 mg and placebo. Placebo scored at 51.7 (50 is neutral with higher numbers more “likeable”), with esmethadone 25, 75, and 150 mg rated at 53.0, 58.2, and 64.9, respectively, compared with oxycodone 40 mg, with a likeability rating of 85. However, the chosen oxycodone dose of 40 mg might be considered inordinately high; a dose of 20 mg could have easily been utilized as it is known to be quote “likeable” by experienced recreational drug users (15) and might have provided valuable information about comparative drug abuse liability of esmethadone. Fourth is the question as to whether the increase in blood levels of methadone by certain SSRIs (9) may have influenced the results obtained, an issue not described in the publication. Fifth, the treatment period was extremely brief, 7 days, and it is unclear whether longer treatment periods would result in a similar efficacy and safety profile. Finally, there is the issue of the primary mechanism of action of esmethadone. There is substantial preclinical evidence that esmethadone acts primarily at the NMDA receptor (16). The fact that its antinociceptive actions are not antagonized by the mu-opiate antagonists naloxone suggests that this pharmacological property of esmethadone is not mediated by the mu opiate receptor (17). The fact that esmethadone is not a mu opiate agonist, does not, however, rule out the possibility that it possesses drug abuse liability. Indeed, it is noteworthy that another primary NMDA receptor antagonist, dextromethorphan, is well known to be a drug of abuse, as is ketamine (18).
In conclusion, the results of this small pilot study are novel, exciting, and certainly worth exploring as are additional, well powered studies of longer duration. The search for novel treatments for major depression remains of paramount importance.
1 : A Delphi-method-based consensus guideline for definition of treatment-resistant depression for clinical trials. Mol Psychiatry (in press)Google Scholar
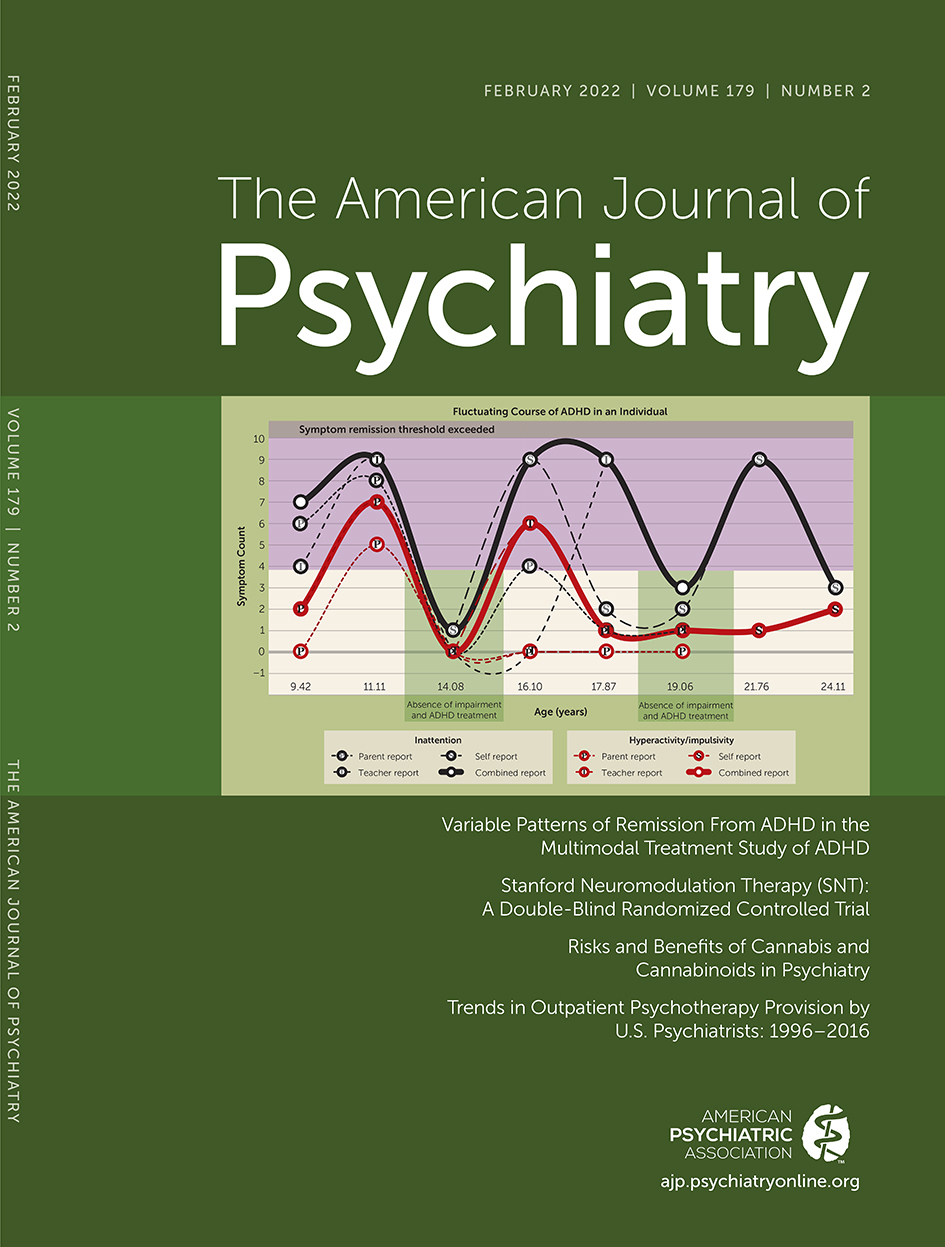
2 Stanford Neuromodulation Therapy (SNT): A double-blind randomized controlled trial. Am J Psychiatry 2022; 179:132–141Link, Google Scholar
3 : Efficacy and safety of intranasal esketamine for the rapid reduction of symptoms of depression and suicidality in patients at imminent risk for suicide: results of a double-blind, randomized, placebo-controlled study. Am J Psychiatry 2018; 175:620–630Link, Google Scholar
4 : Synthesizing the evidence for ketamine and esketamine in treatment-resistant depression: an international expert opinion on the available evidence and implementation. Am J Psychiatry 2021; 178:383–399Link, Google Scholar
5 : Trial of psilocybin versus escitalopram for depression. N Engl J Med 2021; 384:1402–1411Crossref, Medline, Google Scholar
6 : Trial of SAGE-217 in patients with major depressive disorder. N Engl J Med 2019; 381:903–911Crossref, Medline, Google Scholar
7 : Dextromethorphan/bupropion: a novel oral NMDA (N-methyl-d-aspartate) receptor antagonist with multimodal activity. CNS Spectr 2019; 24:461–466Crossref, Medline, Google Scholar
8 : REL-1017 (esmethadone) as adjunctive treatment in patients with major depressive disorder: a phase 2a randomized double-blind trial. Am J Psychiatry 2022; 179:122–131Link, Google Scholar
9 : Psychotherapeutic benefits of opioid agonist therapy. J Addict Dis 2008; 27:49–65Crossref, Medline, Google Scholar
10 : Buprenorphine treatment of refractory depression. J Clin Psychopharmacol 1995; 15:49–57Crossref, Medline, Google Scholar
11 : The effectiveness of methadone maintenance treatment in the reduction of anxiety and depression among drug-related prisoners. Jundishapur J Health Sci 2014; 6:e23475Crossref, Google Scholar
12 : The effect of methadone on depression among addicts: a systematic review and meta-analysis. Health Qual Life Outcomes 2020; 18:373Crossref, Medline, Google Scholar
13 : Selected PET radioligads for ion channel linked neuroreceptor imaging: focus on GABA, NMDA, and nACh receptors. Curr Top Med Chem 2016; 16:1830–1842Crossref, Medline, Google Scholar
14 Relmada Therapeutics announces top-line results of study evaluating REL-1017 vs oxycodone for abuse potential. Relmada Therapeutics. July 27, 2021. [https://www.relmada.com/investors/news/press-releases/detail/237/relmada-therapeutics-announces-top-line-results-of-study]Google Scholar
15 : Human abuse liability assessment of oxycodone combined with ultra-low-dose naltrexone. Psychopharmacology (Berl) 2010; 210:471–480Crossref, Medline, Google Scholar
16 : N-Methyl-D-aspartate receptor antagonist d-methadone produces rapid, mTORC1-dependent antidepressant effects. Neuropsychopharmacology 2019; 44:2230–2238Crossref, Medline, Google Scholar
17 : d-Methadone is antinociceptive in the rat formalin test. J Pharmacol Exp Ther 1997; 283:648–652Medline, Google Scholar
18 : Dextromethorphan in cough syrup: the poor man’s psychosis. Psychopharmacol Bull 2017; 47:59–63Medline, Google Scholar