Adult Outcomes of Youth Irritability: A 20-Year Prospective Community-Based Study
Abstract
Objective: Irritability is a widely occurring DSM-IV symptom in youths. However, little is known about the relationship between irritability in early life and its outcomes in mid-adulthood. This study examines the extent to which youth irritability is related to adult psychiatric outcomes by testing the hypothesis that it predicts depressive and generalized anxiety disorders. Method: The authors conducted a longitudinal community-based study of 631 participants whose parents were interviewed when participants were in early adolescence (mean age=13.8 years [SD=2.6]) and who were themselves interviewed 20 years later (mean age=33.2 years [SD=2.9]). Parent-reported irritability in adolescence was used to predict self-reported psychopathology, assessed by standardized diagnostic interview at 20-year follow-up. Results: Cross-sectionally, irritability in adolescence was widely associated with other psychiatric disorders. After adjustment for baseline emotional and behavioral disorders, irritability in adolescence predicted major depressive disorder (odds ratio=1.33, 95% confidence interval [CI]=1.00–1.78]), generalized anxiety disorder (odds ratio=1.72, 95% CI=1.04–2.87), and dysthymia (odds ratio=1.81, 95% CI=1.06–3.12) at 20-year follow-up. Youth irritability did not predict bipolar disorder or axis II disorders at follow-up. Conclusions: Youth irritability as reported by parents is a specific predictor of self-reported depressive and anxiety disorders 20 years later. The role of irritability in developmental psychiatry, and in the pathophysiology of mood and anxiety disorders specifically, should receive further study.
Although irritability is an element in the criteria for a wide range of DSM-IV disorders, research focusing on the role of irritability in psychiatric nosology is scarce. In this study, we use data from a 20-year follow-up of a community sample to assess associations between irritability in youth and later psychiatric outcomes as well as income and educational attainment outcomes.
In psychiatric nosology, irritability is usually defined as a propensity to react with anger, grouchiness, or tantrums disproportionate to the situation (1 – 3) . No formal definition is presented in DSM-IV, although in youths, irritability features in the criteria for oppositional defiant disorder (i.e., tantrums, anger, touchiness). Also, in youths, but not adults, irritable mood is a criterion for major depressive disorder and dysthymic disorder. For both children and adults, irritability is included in the criteria for bipolar disorder, generalized anxiety disorder, posttraumatic stress disorder, antisocial personality disorder, and borderline personality disorder.
Although the exact population prevalence of irritability is not known, indirect evidence suggests that it may be very common. Data from the Great Smoky Mountains Study show that severe mood dysregulation, a syndrome in which severe, impairing irritability is a defining characteristic, has a lifetime prevalence of 3.3% in youths 9–19 years of age (4) . In a recent community study from the United Kingdom, a construct of mood lability that included irritability as one of its prominent symptoms showed a prevalence of about 5% in youths 8–19 years of age (5) . These data and the relatively high prevalence (6) of disorders in which irritability is a criterion, such as oppositional defiant disorder, suggest that irritability may be common in youths. In adults, although exact prevalence estimates of irritability are lacking, the 12-month prevalence of intermittent explosive disorder, which is typically operationalized as presenting with anger attacks, has been estimated to be 3.9% (7) .
These findings point to a central position of irritability in psychopathology and raise an important question: Is the presence of irritability in youth predictive of later psychiatric disorders, and if so, is this prediction specific or diffuse? An answer to this question can provide important clues about diagnosis and treatment in developmental psychiatry (8) .
In this study, we use data from a community-based study of youths followed over 20 years to address this question. At baseline, we use a parent-reported construct of irritability consisting of items about temper outbursts and anger. The main outcome measure is presence of psychiatric disorders at 20-year follow-up, diagnosed on the basis of structured clinical interviews with the study participants themselves. This cross-informant design has two advantages. First, it reflects the information typically available in clinical settings: parents are the main source of information on youths, and self-report is the most common source of information on adults. Second, it presents a particularly stringent test of predictions as it minimizes the influence of shared method variance (9) .
We tested two hypotheses. Our first hypothesis, based on previous findings (4 , 10 – 12) , was that although irritability in youths would be associated with a number of disorders cross-sectionally, longitudinally it would predict depressive disorders (major depression and dysthymia) and generalized anxiety disorder. This hypothesis is based on three previous analyses. First, in longitudinal studies of community-based samples in Britain, we demonstrated that the irritable symptoms of oppositional defiant disorder were associated with depression and generalized anxiety at 3-year follow-up (11 , 12) . Second, in an analysis of the Great Smoky Mountains Study (4) , we demonstrated that children with severe mood dysregulation at mean age 11 years were at increased risk for depression at age 18; the defining clinical symptom of severe mood dysregulation is severe, persistent irritability. Finally, in a previous report on this sample (10) , we found that chronic irritability predicted depression at 10-year follow-up. Here, we extend the latter work by reporting outcomes predicted by irritability in childhood after 20 years of follow-up. In addition, we tested whether irritability in youth predicts low income and educational attainment in adulthood, even after controlling for associations between adolescent irritability and adult psychiatric diagnoses.
Our second hypothesis was that irritability, but not other symptoms of youth oppositionality, such as arguing with one’s parents or teachers, would be associated with later depressive disorders and generalized anxiety disorder. This differential prediction is based on our previous findings (11 , 12) , noted above, that the irritable symptoms of oppositional defiant disorder, but not its headstrong or hurtful symptoms, predicted depression and generalized anxiety at 3-year follow-up. Here, we test this differential prediction in an independent data set with a much longer longitudinal follow-up by comparing childhood irritability and arguing with respect to their longitudinal associations with adult psychiatric diagnosis.
Method
Sample
As previously described (10 , 13 , 14) , the sample was selected randomly from households in upstate urban and rural New York and first assessed for psychiatric diagnosis in 1983. Participants were reassessed in 1985, 1992, and 2002. At the baseline assessment (N=776), the mean age of participants was 13.8 years (SD=2.6) (13 , 14) . A total of 680 participants (87.6%) were included in the 20-year follow-up, when participants’ mean age was 33.2 years (SD=2.9), and all study-related information was available for 631 of them, for a retention rate of 81.3% for the present study. Men were significantly more likely to have dropped out of the study, and the final sample was 46% male. Age and having any diagnosis at baseline were not significant predictors of dropout.
Assessment
The Diagnostic Interview Schedule for Children (15) was administered in its entirety and used to make DSM-III diagnoses at baseline. Interviews were conducted by trained lay interviewers (14) , and parent and child were interviewed independently. At the 20-year follow-up, axis I disorders were assessed using the Structured Clinical Interview for DSM-IV Axis I Disorders–Non-Patient Edition (16) , and axis II diagnoses were assessed using the Structured Clinical Interview for DSM-IV Personality Disorders (17) . Diagnoses were made by an experienced clinician.
Items used to measure irritability and arguing were derived from the parent-rated Diagnostic Interview Schedule for Children and from parent responses to a scale called the Disorganized Poverty index (DIPOV— d ependency [welfare], i ncomplete family, p remature birth, o ut-of-wedlock birth, v enereal disease under age 20) (18) , designed to capture the Thomas and Chess (19) conceptions of basic childhood temperament dimensions.
The parent-rated irritability measure was the sum of the responses from three items from the Diagnostic Interview Schedule for Children and the DIPOV index:
When parent makes [name of child] do things, does [name of child] have tantrums? (possible responses: no, sometimes, yes)
When teacher makes [name of child] do things, does [name of child] have tantrums? (possible responses: no, sometimes, yes)
How often is [name of child] angry on an average day? (possible responses: never, once in a while, often, constantly)
The Cronbach alpha coefficient of internal consistency was 0.49 for this three-item scale.
The parent-rated arguing measure was of the sum of the responses from three items from the Diagnostic Interview Schedule for Children and the DIPOV index:
Does [name of child] often argue or talk back to parents? (possible responses: no, sometimes, yes)
Does [name of child] argue a lot or talk back to teacher? (possible responses: no, sometimes, yes)
How often does [name of child] argue or talk back to you? (possible responses: never, once in a while, often, constantly)
The Cronbach alpha coefficient was 0.61 for this three-item scale.
For a self-rated construct of irritability, we used the sum of the responses of the following items:
From the Youth Questionnaire:
I feel like losing my temper at people (possible responses: true; mostly true, but not completely true; mostly false, but not completely false; false)
Often have temper outbursts I cannot control (possible responses: not at all, a little, somewhat, quite a bit, extremely)
I am often said to be hot-headed or bad tempered (possible responses: true; mostly true, but not completely true; mostly false, but not completely false; false)
Often feeling easily annoyed or irritated (possible responses: not at all, a little, somewhat, quite a bit, extremely)
From the Youth Diagnostic Interview Schedule for Children:
When your parents make you do something you do not want to do, you get real mad or throw things or run out of the room (possible responses: no, sometimes, yes)
If your teachers make you do something you do not want to do, you get real mad or throw things or run out of the room (possible responses: no, sometimes, yes)
The Cronbach alpha coefficient was 0.66 for this six-item scale.
Educational attainment was assessed using a scale (0=no high school degree; 8=postgraduate university degree) previously described (20) . Income was coded using a 20-point scale ranging from $0 to more than $100,000 pretax annual earnings.
Statistical Analysis
Logistic regression analyses were used to test the first hypothesis, with DSM-IV diagnoses as the dependent variable. The standardized measure of irritability was the independent variable, and all models included age, gender, and socioeconomic status as covariates. Models predicting longitudinal outcomes were adjusted for baseline disorders: emotional disorders (major depressive disorder, overanxious disorder, simple phobia, social phobia, panic disorder, and bipolar disorder) and behavioral disorders (conduct disorder, oppositional defiant disorder, and attention deficit hyperactivity disorder [ADHD]). To ensure that subsyndromal symptoms of psychiatric disorders at baseline did not account for the association between irritability and 20-year outcomes, we also used scaled symptoms for major depressive disorder, overanxious disorder, oppositional defiant disorder, and conduct disorder as covariates in additional analyses.
To test our second hypothesis, comparing the predictions of irritability to those of arguing, z scores for irritability and arguing were entered as independent variables in the same logistic regression models. In addition, we tested our second hypothesis using a formalized mediation test (21) as implemented in Stata 10 (Stata Corp, College Station, Tex.). This included the outcome variable (e.g., major depression at 20-year follow-up), the z score of arguing as an independent predictor, and the z score of irritability as a mediator variable.
The income variable was reflected, log transformed, reflected back to meet normality assumptions, and then used in linear regression models. The educational attainment variable was analyzed using ordinal logistic regression after ensuring that the parallel regression assumption was met.
Unless otherwise indicated, multiple imputation as implemented in Stata was used under the missing-at-random assumption to create 10 imputed data sets. The results obtained from the imputed data sets were compared to those nonimputed. Differences were small; the estimates for the odds ratios and confidence intervals of predictions from irritability to psychiatric outcomes at 20-year follow-up did not deviate by more than 10%. Models were checked for the presence of collinearity by calculating the variance inflation factor.
Ethical Approval
Study procedures were approved by the institutional review boards of Columbia University and the New York State Psychiatric Institute. After study procedures were explained, written consent was obtained from parents and participants over age 18, and written assent was obtained from children under age 18.
Results
Associations Between Adolescent Irritability and Adult Diagnoses and Attainment
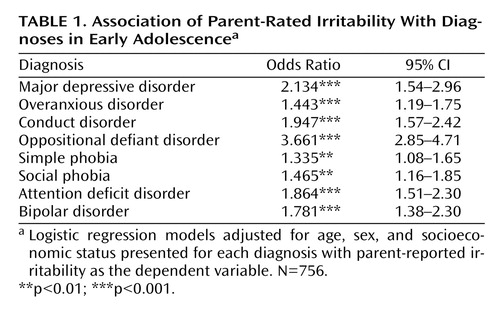
Parent-rated irritability showed wide-ranging cross-sectional associations with psychiatric disorders at baseline ( Table 1 ).
At 20-year follow-up, past-year prevalence rates for psychiatric disorders were as follows: major depressive disorder, 12.4%; dysthymic disorder, 2.1%; bipolar disorder, 1.6%; generalized anxiety disorder, 2.9%; obsessive-compulsive disorder, 4%; agoraphobia, 4.3%; and any DSM-IV axis II disorder, 15.4%. Table 2 lists the predictions from youth irritability to psychiatric disorders at 20-year follow-up, unadjusted, adjusted for emotional disorders, and adjusted for emotional and behavioral disorders. Parent-reported irritability predicted major depressive disorder, generalized anxiety disorder, and dysthymia.
In adjusted or unadjusted models, irritability did not predict bipolar disorder or other anxiety disorders other than generalized anxiety disorder, either individually or as a composite category. Irritability at baseline was not a significant predictor of borderline personality disorder after adjustment for emotional and behavioral disorders, nor of antisocial personality disorder after controlling for baseline emotional disorders, nor of ADHD (conduct problems in adolescence were not entered as a predictor as they form part of the definition of antisocial personality disorder). Irritability also did not predict any other axis II cluster or substance abuse or dependence.
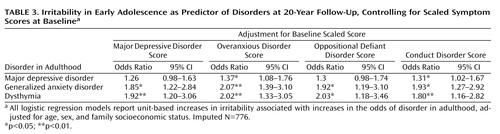
The adjusted models indicated that psychiatric diagnoses at baseline did not account for associations between irritability in early adolescence and major depressive disorder, generalized anxiety disorder, or dysthymia in adulthood. To strengthen this conclusion, we covaried for baseline measures on scales for overanxious disorder, major depressive disorder, oppositional defiant disorder, and conduct disorder. After adjustment for symptom scores, youth irritability remained a significant predictor of generalized anxiety disorder and dysthymia; however, controlling for baseline scores of major depressive disorder and oppositional defiant disorder rendered the relationship between irritability and major depression nonsignificant ( Table 3 ).
In addition, we asked whether the presence of irritability at baseline would be predictive of lower attainment at 20-year follow-up. Irritability at baseline was significantly negatively associated with income and educational attainment at follow-up. This relationship was not mediated through the presence of major depressive disorder, generalized anxiety disorder, or dysthymia at follow-up ( Table 4 ).
Predictive Value of Irritability Versus Arguing
We sought to establish whether the relationship between irritability and major depression, dysthymia, and generalized anxiety disorder is specific, or whether arguing with one’s parents or teachers would have similar predictions. Irritability and arguing were strongly correlated with each other (r=0.50, p<0.001). In univariate models, arguing predicted major depression at 20-year follow-up (odds ratio=1.36, 95% CI=1.07–1.74, p<0.05), but not generalized anxiety disorder or dysthymia. Furthermore, the results of the Sobel test showed that approximately 71% of the association between arguing and later major depression was mediated through the association between arguing and irritability (Sobel coefficient=0.025, p<0.01; indirect to direct effect ratio=2.46).
Moving from univariate to multivariate models, we performed logistic regressions in which z scores for both irritability and arguing were entered as independent variables into the same model ( Table 5 ). Associations between arguing and major depressive disorder, dysthymia, or generalized anxiety disorder were not significant when both irritability and arguing were entered into the same model. We also wanted to ensure that the predictions seen using the scales for irritability and arguing held even when the individual items comprising each scale were compared to each other. Indeed, anger or tantrums in reaction to parents’ requests were significant predictors of major depressive disorder, generalized anxiety disorder, and dysthymia when compared to frequency of arguing, arguing with one’s parents, or arguing with one’s teachers. Only arguing with one’s teachers was a significant predictor (over having tantrums in response to teachers’ requests) of major depressive disorder and generalized anxiety disorder, but not dysthymia. (Details are available in a data supplement that accompanies the online edition of this article.)
Results Using Self-Reported Irritability
We asked whether the predictions from youth irritability to later outcomes were unique to parent report, or whether self-reported youth irritability is similarly predictive. After adjustment for baseline emotional and behavioral disorders, self-rated irritability at baseline did not predict any axis I disorder at 20-year follow-up, nor did it predict cluster A or cluster B axis II disorders. Self-rated irritability at baseline did predict cluster C axis II disorders (odds ratio=1.38, 95% CI=1.04–1.82, p<0.024), although this finding became nonsignificant when adjusted for scale measures of major depressive disorder, overanxious disorder, conduct disorder, or oppositional disorder at baseline.
Discussion
We used data from a 20-year community follow-up study to investigate the extent to which youth irritability is a risk for adult psychiatric disorders. Parent-reported irritability in youths at a mean age of 13.8 years predicted major depression, dysthymia, and generalized anxiety disorder at 20-year follow-up, even after adjustment for baseline emotional and behavioral disorders. The prediction of major depression and dysthymia from irritability is unlikely to be due to item overlap, since irritability is not a criterion for these diagnoses in adulthood. However, the possibility of item overlap cannot be excluded for generalized anxiety disorder. Irritability at baseline predicted lower educational achievement and income at follow-up; this relationship was direct and not mediated through major depression, generalized anxiety disorder, or dysthymia at follow-up. We also found that only parent-reported, but not self-reported, irritability predicted later psychiatric outcomes. Finally, we compared irritability and arguing and found that the prediction of depressive disorders and generalized anxiety disorder was specific to irritability.
Irritability was associated with a wide range of youth psychiatric disorders cross-sectionally. However, as hypothesized, in spite of irritability’s diffuse cross-sectional associations, its longitudinal predictions were specific, in that it increased the risk only for depressive disorders and generalized anxiety disorder. A one-standard-deviation increase in adolescent irritability nearly doubled the risk of generalized anxiety disorder 20 years later, even after adjusting for emotional disorders at baseline. The adjustment for baseline psychopathology using scaled symptoms of major depression or oppositional defiant disorder attenuated the prediction of irritability to major depression at 20-year follow-up, rendering it nonsignificant, perhaps because of overlap of oppositional defiant disorder symptoms with irritability items. However, irritability remained predictive of generalized anxiety disorder and dysthymia even when baseline symptoms were controlled for. Our results also show that adolescent irritability is associated with lower income and educational attainment in adulthood; this relationship is not mediated by major depression, generalized anxiety disorder, or dysthymia at follow-up. Notably, irritability did not predict adult bipolar disorder or any axis II disorder, even in models unadjusted for baseline psychopathology.
Our second hypothesis was that irritability, defined as temper tantrums and anger, would predict depressive disorders or generalized anxiety disorder in adulthood but that arguing with others would not. Irritability and arguing are both symptoms of oppositional defiant disorder, but in previous work (11 , 12) we found that irritability forms a dimension of oppositional defiant disorder that specifically predicts depressive disorders and generalized anxiety disorder. Conversely, symptoms such as arguing with others appear to form a headstrong symptom-dimension of oppositional defiant disorder that predicts ADHD and conduct disorder but not emotional disorders (11 , 12) . We found that despite a high correlation between arguing and irritability at baseline, irritability, rather than arguing, predicted later depressive disorders and generalized anxiety disorder. The data presented here add to a growing body of literature (11 , 12) suggesting that irritability and arguing in youth, both of which are components of oppositional defiant disorder, may have differential predictions. This distinction may be relevant for pathophysiological studies of youth oppositionality.
Several points about irritability are worth noting when considering its relationship with psychiatric disorders. The hallmark emotion of irritability—anger—is thought to be one of the earliest appearing in human development (23) . Anger is also thought to occupy a central position between internalizing and externalizing problems. While anger and fear together are regarded as part of a negative affect personality dimension (24 , 25) that is a risk factor for internalizing problems (26 , 27) , in factor analyses anger also separates from fear (27 , 28) and predicts externalizing, aggressive behaviors (26 , 29) . In particular, irritability appears to be associated with a specific, impulsive form of hostile behavior (30) that may be differentiated from other forms of aggression by quantitative-genetic (31) and neurobiological findings (32) . These data suggest that irritability occupies a position at the interface between emotional and disruptive behavior problems.
Our results show that irritability is significantly associated with both emotional and behavioral disorders cross-sectionally during adolescence but is related only to depressive disorders and generalized anxiety disorder at age 33. This could suggest that the relationship between irritability and behavioral problems is pronounced in adolescence and diminishes thereafter, while the link between irritability and emotional problems persists. Alternatively, these results might be explained by the lack of an adult equivalent of oppositional defiant disorder. That is, adults with depression and anger episodes might receive a diagnosis of depression (33 , 34) , whereas such a presentation in youth might lead to the diagnoses of both oppositional defiant disorder and major depression. In this context it is important to note that intermittent explosive disorder, a disorder that appears to occur frequently in the general population (7) , is strongly associated with mood and anxiety disorders, suggesting a link between impulse control and affect regulation in adults. Unfortunately, the present study did not ascertain intermittent explosive disorder. It seems particularly important that future longitudinal studies collect data on intermittent explosive disorder outcome and on adult measures of irritability. This would help in establishing whether the prediction from baseline to depressive disorders and generalized anxiety disorder is mediated by the persistence of irritability into adulthood.
Our study has a number of limitations that should be taken into account. First, our irritability scale consisted of only three items and thus had only modest internal consistency, which constrained the upper bound of the predictive value (35) . However, the fact that such a short scale strongly predicted a specific set of disorders over 20 years could be seen as evidence of the robustness of the construct. Second, while some participants were lost to follow-up, the attrition rate is well within what is considered reasonable for such a long follow-up period, and we used a multiple-imputation approach to minimize the likelihood of inaccurate estimates.
1. Bleueler E: Lehrbuch der Psychiatrie. Berlin, Springer, 1916Google Scholar
2. Buss AH, Durkee A: An inventory for assessing different kinds of hostility. J Consulting Psychol 1957; 21:343–349Google Scholar
3. Snaith RP, Taylor CM: Irritability: definition, assessment, and associated factors. Br J Psychiatry 1985; 147:127–136Google Scholar
4. Brotman MA, Schmajuk M, Rich BA, Dickstein DP, Guyer AE, Costello EJ, Egger HL, Angold A, Pine DS, Leibenluft E: Prevalence, clinical correlates, and longitudinal course of severe mood dysregulation in children. Biol Psychiatry 2006; 60:991–997Google Scholar
5. Stringaris A, Goodman R: Mood lability and psychopathology in youth. Psychol Med (Epub ahead of print, Dec 11, 2008)Google Scholar
6. Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A: Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry 2003; 60:837–844Google Scholar
7. Kessler RC, Coccaro EF, Fava M, Jaeger S, Jin R, Walters E: The prevalence and correlates of DSM-IV intermittent explosive disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry 2006; 63:669–678Google Scholar
8. Costello EJ, Pine DS, Hammen C, March JS, Plotsky PM, Weissman MM, Biederman J, Goldsmith HH, Kaufman J, Lewinsohn PM, Hellander M, Hoagwood K, Koretz DS, Nelson CA, Leckman JF: Development and natural history of mood disorders. Biol Psychiatry 2002; 52:529–542Google Scholar
9. Bank L, Dishion TJ, Skinner M, Patterson GR: Method variance in structural equation modeling: living with “glop,” in Depression and Aggression in Family Interaction. Edited by Patterson GR. Hillsdale, NJ, Lawrence Erlbaum Associates, 1990, pp 247–280Google Scholar
10. Leibenluft E, Cohen P, Gorrindo T, Brook JS, Pine DS: Chronic versus episodic irritability in youth: a community-based, longitudinal study of clinical and diagnostic associations. J Child Adolesc Psychopharmacol 2006; 16:456–466Google Scholar
11. Stringaris A, Goodman R: Three dimensions of oppositionality in youth. J Child Psychol Psychiatry 2009; 50:216–223Google Scholar
12. Stringaris A, Goodman R: Longitudinal outcome of youth oppositionality: irritable, headstrong, and hurtful behaviors have distinctive predictions. J Am Acad Child Adolesc Psychiatry 2009; 48:404–412Google Scholar
13. Pine DS, Cohen E, Cohen P, Brook J: Adolescent depressive symptoms as predictors of adult depression: moodiness or mood disorder? Am J Psychiatry 1999; 156:133–135Google Scholar
14. Pine DS, Cohen P, Gurley D, Brook J, Ma Y: The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch Gen Psychiatry 1998; 55:56–64Google Scholar
15. Costello EJ, Edelbrock CS, Costello AJ: Validity of the NIMH Diagnostic Interview Schedule for Children: a comparison between psychiatric and pediatric referrals. J Abnorm Child Psychol 1985; 13:579–595Google Scholar
16. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders—Non-Patient Edition (SCID-I/NP), version 2.0. New York, New York State Psychiatric Institute, Biometrics Research, 1996Google Scholar
17. First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin L: Structured Clinical Interview for DSM-IV Personality Disorders (SCID-II). New York, Biometrics Research Department, New York State Psychiatric Institute, 2000Google Scholar
18. Kogan LS, Jenkins S: Indicators of Child Health and Welfare: Development of the DIPOV Index. New York, Columbia University Press, 1974Google Scholar
19. Thomas A, Chess S: Temperament and Development. New York, Bruner/Mazel, 1977Google Scholar
20. Crawford TN, Cohen P, First MB, Skodol AE, Johnson JG, Kasen S: Comorbid axis I and axis II disorders in early adolescence: outcomes 20 years later. Arch Gen Psychiatry 2008; 65:641–648Google Scholar
21. Sobel ME: Asymptotic confidence intervals for indirect effects in structural equation models. Sociol Methodol 1982; 13:290–312Google Scholar
22. Royston P: Multiple imputation of missing values: update. Stata Journal 2005; 5:1–14Google Scholar
23. Buss AH, Plomin R: The EAS approach to temperament, in The Study of Temperament: Changes, Continuities, and Challenges. Edited by Plomin R, Dunn J. Hillsdale, NJ, Lawrence Erlbaum Associates, 1986Google Scholar
24. Tellegen A: Structures of mood and personality and their relevance to assessing anxiety, with an emphasis on self-report, in Anxiety and the Anxiety Disorders. Edited by Tuma A, Maser J. Hillsdale, NJ, Lawrence Erlbaum Associates, 1985Google Scholar
25. Watson D, Clark LA: Negative affectivity: the disposition to experience aversive emotional states. Psychol Bull 1984; 96:465–490Google Scholar
26. Ormel J, Oldehinkel AJ, Ferdinand RF, Hartman CA, De Winter AF, Veenstra R, Vollebergh W, Minderaa RB, Buitelaar JK, Verhulst FC: Internalizing and externalizing problems in adolescence: general and dimension-specific effects of familial loadings and preadolescent temperament traits. Psychol Med 2005; 35:1825–1835Google Scholar
27. Rothbart MK: Temperament, development, and personality. Curr Dir Psychol Sci 2007; 16:207–212Google Scholar
28. John OP, Caspi A, Robins RW, Moffitt TE, Stouthamer-Loeber M: The “little five”: exploring the nomological network of the five-factor model of personality in adolescent boys. Child Dev 1994; 65:160–178Google Scholar
29. Arsenio WF, Cooperman S, Lover A: Affective predictors of preschoolers’ aggression and peer acceptance: direct and indirect effects. Dev Psychol 2000; 36:438–448Google Scholar
30. Vitiello BS, Stoff DM: Subtypes of aggression and their relevance to child psychiatry. J Am Acad Child Adolesc Psychiatry 1997; 36:307–315Google Scholar
31. Coccaro EF, Bergeman CS, Kavoussi RJ, Seroczynski AD: Heritability of aggression and irritability: a twin study of the Buss-Durkee Aggression Scales in adult male subjects. Biol Psychiatry 1997; 41:273–284Google Scholar
32. Coccaro EF, Kavoussi RJ, Cooper TB, Hauger RL: Central serotonin activity and aggression: inverse relationship with prolactin response to d -fenfluramine, but not CSF 5-HIAA concentration, in human subjects. Am J Psychiatry 1997; 154:1430–1435 Google Scholar
33. Dougherty DD, Rauch SL, Deckersbach T, Marci C, Loh R, Shin LM, Alpert NM, Fischman AJ, Fava M: Ventromedial prefrontal cortex and amygdala dysfunction during an anger induction positron emission tomography study in patients with major depressive disorder with anger attacks. Arch Gen Psychiatry 2004; 61:795–804Google Scholar
34. Fraguas R Jr, Papakostas GI, Mischoulon D, Bottiglieri T, Alpert J, Fava M: Anger attacks in major depressive disorder and serum levels of homocysteine. Biol Psychiatry 2006; 60:270–274Google Scholar
35. Lord FM, Novick MR: Statistical Theories of Mental Test Scores. Reading, Mass, Addison-Wesley, 1968Google Scholar