Dr. Jayaram Replies
To the Editor: We thank Dr. Weiss for his observations on our article. The six Ps that he recommends are indeed an easy way to analyze critical incidents. Vincent et al. (1) summarized the approach to not blaming individuals and to examining systems that permit errors to occur, with an emphasis toward improving performance by correcting organizational lapses, oversights, and policies.
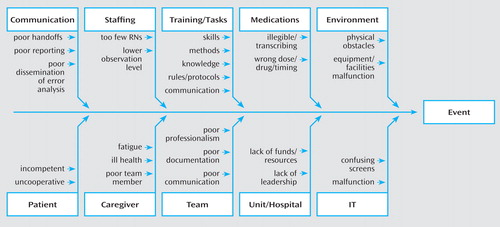
The APA Patient Safety Committee has described a team approach to reviewing factors that contribute to adverse incidents (2 – 6) . Dr. Weiss advocates such an approach with his mnemonic. The publications of the APA Patient Safety Committee are pertinent to the process of analyzing adverse events in psychiatry and may be of interest to those who are in leadership positions at psychiatric care facilities (2 – 6) . Additionally, the APA Patient Safety Committee has developed guidelines similar to those of Vincent et al. and others and has produced a handbook of patient safety that is available to all its members on the APA website (7) . In a chapter on root-cause analysis (7) , the process of examining adverse events is discussed as well as various entities/variables that may impact the care process. One way to answer the “why did this happen” question and pursue possible areas for intervention is to use the root-cause analysis diagram ( Figure 1 ), until the “why” question can no longer by asked.
We welcome collaborative efforts by Dr. Weiss and others toward advancing patient safety in the field of psychiatry.
1. Vincent C, Taylor-Adams S, Chapman E, Hewett D, Prior S, Strange P, Tizzard A: How to investigate and analyse clinical incidents: clinical risk unit association of litigation and risk management protocol. Br Med J 2000; 320:777–781Google Scholar
2. Jayaram G: Patient safety forum: developing a strategic plan. Psychiatr Serv 2004; 55:259–263Google Scholar
3. Grasso BC, Rothschild JM, Jordan CW, Jayaram G: What is the measure of a safe hospital? medication errors missed by management, clinical staff and surveyors. J Psychiatr Prac 2005; 11:1–7Google Scholar
4. Jayaram G: Psychiatrists strive to assure patient safety. Direct Psychiatr 2006; 4:185–196Google Scholar
5. Jayaram G: Implementing performance improvement and measuring psychiatric care quality. Psychiatry 2007; 4:58–61Google Scholar
6. Jayaram G: Medication errors in psychiatric treatment: Where do we go from here? Psychiatry 2007; 4:63–64Google Scholar
7. Jayaram G, Herzog AL: Handbook on Patient Safety: SAFEMD: Practical Applications and Approaches to Safe Psychiatric Practice. Arlington, Va, American Psychiatric Publishing, 2008Google Scholar



