Prevalence and Correlates of Shoplifting in the United States: Results From the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC)
Abstract
Objective: This study presented nationally representative data on the lifetime prevalence, correlates, and comorbidity of shoplifting among adults in the United States. Method: Data were derived from a large national sample of the United States population. Face-to-face surveys of more than 43,000 adults ages 18 years and older residing in households were conducted during the 2001–2002 period. Diagnoses of mood, anxiety, and drug disorders as well as personality disorders were based on the Alcohol Use Disorder and Associated Disabilities Interview Schedule—DSM-IV Version. Results: The prevalence of lifetime shoplifting in the U.S. population was 11.3%. Associations between shoplifting and all antisocial behaviors were positive and significant. Besides stealing, the behaviors more strongly associated with shoplifting were making money illegally and scamming someone for money. Strong associations between shoplifting and all 12-month and lifetime comorbid psychiatric disorders were also found. The strongest associations with shoplifting were with disorders often associated with deficits in impulse control, such as antisocial personality disorder, substance use disorders, pathological gambling, and bipolar disorder. High rates of mental health service use were also identified in this population. Conclusions: Shoplifting is a relatively common behavior. A history of shoplifting is associated with substantial rates of comorbid disorders, psychosocial impairment, and mental health service use. Future research should identify the biological and environmental underpinnings of shoplifting and develop effective screening tools and interventions for individuals with shoplifting problems.
The National Association of Shoplifting Prevention estimates that one in 11 people has shoplifted during his or her lifetime and that men are as likely to shoplift as women (1) . In fact, more than $13 billion worth of goods are stolen from retailers in the United States each year (2) . Shoplifting results in significant costs to the legal system and commerce. Despite these costs, shoplifting has historically received relatively little attention from clinicians and researchers. As such, our understanding of the basic aspects of this behavior is incomplete.
Shoplifting and kleptomania are sometimes used synonymously, yet there are important differences between them. Shoplifting is a behavior defined by the theft of an item from a store, regardless of motivation or desire for the items (3) . By contrast, kleptomania refers to a psychiatric diagnosis characterized by recurrent failure to resist impulses to steal objects that are not needed for personal use or for their monetary value. Individuals with kleptomania experience an increasing sense of tension immediately before committing the theft and gratification or release at the time of committing the theft. Furthermore, the stealing is not committed to express anger or vengeance. Thus, although shoplifting can be due to kleptomania, it can also be simply criminal behavior or a manifestation of conduct disorder, antisocial personality disorder, or bipolar disorder, among others. More generally, the relationship of shoplifting to other behaviors is poorly understood, and the prevalence of psychiatric disorders among people who shoplift is unknown.
Research on kleptomania suggests that this disorder is associated with several domains of psychopathology, including impulsivity, psychopathy, mood disorders (4 – 6) , and obsessive-compulsive spectrum disorders (7 , 8) , although empirical data examining these associations is sparse. Similarly, individuals with kleptomania are thought to seek treatment only rarely because of social stigma (5 , 9) , although they may seek treatment for other reasons (10) . However, given the differences between shoplifting and kleptomania, the applicability of even the limited literature on kleptomania to shoplifting is unknown. To date, to our knowledge, no study has reported the rates of psychiatric disorders or mental health service use among individuals with a lifetime history of shoplifting.
The purpose of this study was to fill these gaps in knowledge. Specifically, with the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a nationally representative sample of the adult population of the United States, we sought to 1) examine the prevalence and sociodemographic correlates of shoplifting in the general population, 2) document the prevalence of other impulsive and antisocial behaviors in people who have shoplifted, 3) investigate the lifetime and 12-month prevalence of psychiatric disorders associated with shoplifting and the current levels of psychosocial functioning in several domains, and 4) estimate lifetime and 12-month rates of mental health treatment-seeking among individuals with a lifetime history of shoplifting.
Method
Sample
The 2001–2002 NESARC is a nationally representative sample of the adult population of the United States conducted by the U.S. Census Bureau under the direction of the National Institute on Alcoholism and Alcohol Abuse, as described in detail elsewhere (11 , 12) . The NESARC target population was the civilian noninstitutionalized population, 18 years and older, residing in households and group quarters in the 50 states and the District of Columbia. The final sample included 43,093 respondents drawn from individual households and group quarters. African Americans, Latinos, and young adults (ages 18 to 24 years) were oversampled. Data were adjusted to account for oversampling and respondent and household nonresponse. The overall survey response rate was 81%. The weighted data were then adjusted with the 2000 decennial census to be representative of the U.S. civilian population for a variety of sociodemographic variables.
All potential NESARC respondents were informed in writing about the nature of the survey, the statistical uses of the survey data, the voluntary aspect of their participation, and the federal laws that rigorously provided for the strict confidentiality of the identifiable survey information. The respondents consenting to participate after receiving this information were interviewed. The research protocol, including informed consent procedures, received full ethical review and approval from the U.S. Census Bureau and the U.S. Office of Management and Budget.
Interviewer Training
Interviews were conducted by approximately 1,800 professional interviewers from the U.S. Census Bureau. Training was standardized under the direction of the National Institute of Alcoholism and Alcohol Abuse. For quality control purposes and to verify the accuracy of the interviewers’ performance, 2,657 respondents were readministered one to three sections of the NESARC interview to verify answers. These interviews also formed the basis of a test-retest reliability study of NESARC measures (11) .
Diagnostic Assessment
Sociodemographic measures included age, sex, race/ethnicity, nativity, marital status, place of residence, and region of the country. Socioeconomic measures included education, insurance type, and individual and family income.
All psychiatric diagnoses were made according to the DSM-IV criteria with the National Institute of Alcoholism and Alcohol Abuse Alcohol Use Disorder and Associated Disabilities Interview Schedule—DSM-IV Version (AUDADIS-IV), a valid and reliable fully structured diagnostic interview designed for use by professional interviewers who are not clinicians. AUDADIS-IV diagnoses can be separated into five groups: 1) substance use disorders (alcohol abuse/dependence, drug abuse/dependence, and nicotine dependence), 2) mood disorders (major depressive disorder, dysthymia, and bipolar disorder), 3) anxiety disorders (panic disorder, social anxiety disorder, specific phobia, and generalized anxiety disorder), 4) personality disorders (avoidant, dependent, obsessive-compulsive, paranoid, schizoid, histrionic, and antisocial personality disorders), and 5) other (conduct disorder and pathological gambling). Diagnoses of personality disorders required long-term patterns of social and occupational impairment and exclusion of substance-induced cases, as detailed elsewhere (13) . The test-retest reliability and validity of AUDADIS-IV measures of DSM-IV disorders is good to excellent (14 – 17) . Owing to concerns about the validity of psychotic diagnoses in general population surveys as well as the length of the interview, possible psychotic disorders were assessed by asking the respondent if the respondent was ever told by a doctor or other health professional that he or she had schizophrenia or a psychotic disorder.
Embedded in the antisocial personality disorder section was the following question: “In your entire life, did you ever shoplift?” All NESARC participants were asked this question. Individuals who answered affirmatively were defined in this article as having a history of shoplifting. They were further asked, “Has this happened since you were 15?” Test-retest reliability of the entire antisocial personality disorder section in the NESARC is 0.69 (18) . Although test-retest reliability of individual items is unavailable, we computed Cronbach’s alpha for the antisocial personality disorder symptoms, which was 0.86, indicating excellent internal consistency of the antisocial personality disorder section. This value was unchanged when the shoplifting item was excluded, suggesting high reliability for the item. Functioning was assessed with the physical component summary and the social, emotional, and mental health scores of the Short-Form-12v2, a reliable and valid impairment measure in population surveys (19) . Each Short-Form-12v2 norm-based disability score is a continuous variable with a mean of 50 in the general population, an SD of ±10, and a range of 0–100. Lower scores indicate more disability. To assess family history of antisocial behavior, individuals were also asked whether any first- or second-degree relatives had engaged in antisocial personality disorder symptoms, such as being cruel to people or animals, destroying property, lying or conning people, or being arrested.
To estimate the rates of mental health service use, separate questions were asked for each major substance use, mood, and anxiety disorder assessed in the NESARC. Respondents were classified as receiving treatment if they sought mental health treatment from a counselor, therapist, doctor, psychologist, or an emergency room; if they were hospitalized at least one night for psychiatric reasons; or if they were prescribed medications to treat psychiatric symptoms.
Statistical Analyses
Weighted percentages and means were computed to derive sociodemographic and clinical characteristics of respondents with and without a lifetime history of shoplifting. Standard errors and 95% confidence intervals (CIs) for all analyses were estimated by using SUDAAN (20) , a software package that uses Taylor series linearization to adjust for the design effects of complex sample surveys such as the NESARC. Because the combined SE of two means (or percents) is always equal to or less than the sum of the standard errors of those two means, we conservatively consider that two CIs that do not overlap are significantly different from one another (21) . We consider significant odds ratios those whose CI does not include 1. Two sets of logistic regressions examined associations between shoplifting and lifetime and 12-month comorbid psychiatric disorders. The first set adjusted only for sociodemographic characteristics that differed between individuals with and without a lifetime history of shoplifting. The second set further adjusted for the presence of other comorbid psychiatric disorders to identify common and unique factors underlying the associations of comorbid disorders with shoplifting.
To examine whether the correlates of shoplifting were different among the individuals who shoplifted past childhood, all analyses were repeated, restricting the group of shoplifters to those who shoplifted after the age of 15. Similar analyses were conducted excluding individuals with a diagnosis of antisocial personality disorder. Because these two sets of analyses resulted in a nearly identical pattern of significant odds ratios to those reported with the lifetime history of shoplifting and the inclusion of individuals with antisocial personality disorder, only the results associated with the lifetime history grouping and antisocial personality disorder are presented.
Results
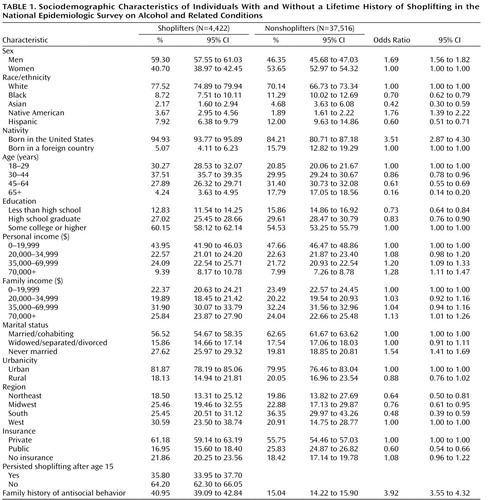
Sociodemographic and Socioeconomic Characteristics ( Table 1 )
The overall lifetime prevalence of shoplifting in the general population was 11.3% (95% CI=10.6%–12.1%). The odds of shoplifting were significantly higher in men than in women. Native Americans had higher odds than whites, although blacks, Hispanics, and Asian Americans had lower odds of shoplifting than non-Hispanic whites. Being U.S.-born, never married, or in the youngest cohort (ages 18–29) also increased the risk for shoplifting. Shoplifting was significantly more common in individuals with at least some college education, among those with individual incomes over $35,000 and family incomes over $70,000, and among those living in the West, but less common among those with public insurance. Individuals with a history of shoplifting were more likely than those without a history of shoplifting to have a family history of antisocial behaviors. In over one-third of the cases, shoplifting persisted after age 15.
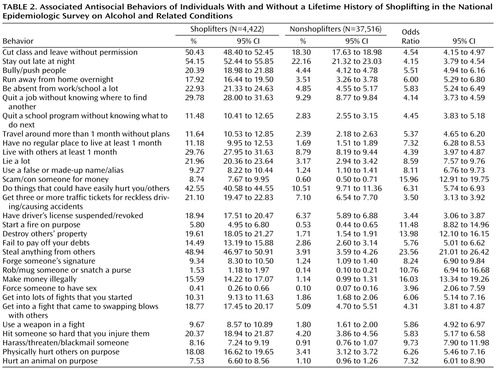
Associated Antisocial Behaviors ( Table 2 )
The prevalence of all antisocial behaviors was higher among individuals with a history of shoplifting than among those with no self-reported history of shoplifting. For both groups, the most common behavior was staying out at night against parental advice, the prevalence of which was 54.15% (95% CI=52.44%–55.85%) among individuals with a history of shoplifting versus 22.16% (CI=21.32%–23.03%) among those with no history of shoplifting. Besides stealing, the behaviors more strongly associated with shoplifting, as measured by the odds ratio, were making money illegally (odds ratio=16.03, 95% CI=13.34–19.26) and scamming somebody for money (odds ratio=15.96, 95% CI=12.91–19.75).
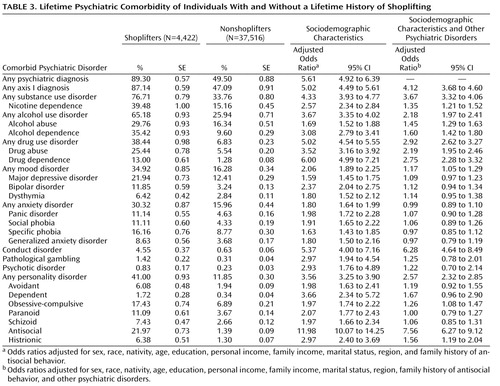
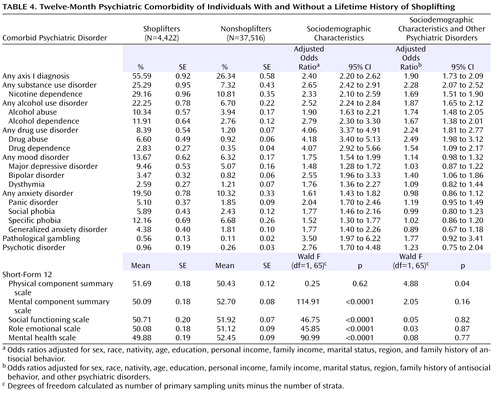
Lifetime and Current Comorbidity ( Table 3 and Table 4 )
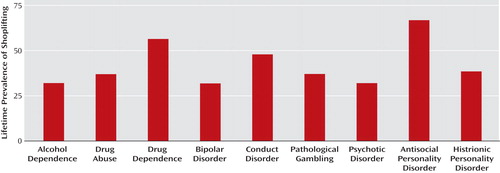
The vast majority of individuals with a lifetime history of shoplifting (89.30%, CI=87.20%–89.60%) had a lifetime history of at least one psychiatric diagnosis, compared to 49.50% in nonshoplifters. Shoplifters were significantly more likely than nonshoplifters to have a lifetime axis I disorder (87.14%, CI=85.91%–88.28%, versus 47.09%, CI=45.29%–48.91%) and a personality disorder (41.00%, CI=39.15%–42.88%, versus 11.85%, CI=11.26%–12.45%). In both groups, the most prevalent disorders were nicotine dependence and alcohol use disorders, which carried an increased risk of 2.57 and 3.67, respectively, among shoplifters compared with nonshoplifters, after adjustment for sociodemographic characteristics. Although all psychiatric conditions were significantly associated with shoplifting, the strongest associations were found for antisocial personality disorder (odds ratio=11.98, CI=10.07–14.25) and substance use disorders (odds ratio=4.33, CI=3.93–4.77). Other disorders often associated with deficits in impulse control, such as pathological gambling (odds ratio=2.97, CI=1.94–4.54) and bipolar disorder (odds ratio=2.37, CI=2.04–2.75), were also strongly associated with shoplifting, whereas association with mood and anxiety disorders, although also significant, was of smaller magnitude (odds ratio <2.0). A similar pattern was observed when we examined current, rather than lifetime, diagnoses of axis I disorders. During adjustment for the presence of other psychiatric disorders, associations with lifetime conduct disorder, antisocial personality disorder, obsessive-compulsive personality and histrionic disorders, and lifetime and 12-month substance use disorders remained positive and statistically significant. The lifetime prevalence of shoplifting was also high, with rates often above 25%, among those with psychiatric disorders ( Figure 1 ).
Individuals with a lifetime history of shoplifting had higher scores on the physical component summary score but lower scores on the social, emotional, and mental health scale of the Short-Form Health Survey—12. When we adjusted for the presence of other psychiatric disorders, the scores on the Short-Form Health Survey—12 social, emotional, and mental subscales lost their statistical significance, whereas the physical component summary score became significant.
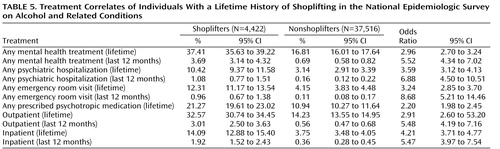
History of Psychiatric Treatment ( Table 5 )
Lifetime rates of treatment seeking for psychiatric disorders were significantly higher among shoplifters than nonshoplifters across all treatment settings and regardless of whether lifetime or past year timeframe was considered. Over a third of shoplifters had a lifetime history of mental health treatment, compared with only 16.81% of nonshoplifters. Any psychiatric hospitalization, emergency room visit, and even past-12-month outpatient or inpatient psychiatric treatment rate was five or more times higher among shoplifters than nonshoplifters.
Additional Analyses
To examine the impact of age at shoplifting on our results, we examined the subsample of individuals with a history of shoplifting after age 15. The associations with other antisocial behaviors and psychiatric disorders remained significant and of similar magnitude when we restricted the analyses to those who shoplifted after age 15. Similarly, exclusion of individuals with a diagnosis of antisocial personality disorder did not alter the direction or strength of the findings (results available upon request from the first author).
Discussion
To our knowledge, this is the first national study to report on rates of shoplifting in the United States. We found that a lifetime history of shoplifting was common and associated with high rates of other antisocial behaviors, lifetime and current psychiatric disorders, significant decreases in levels of psychosocial functioning, and elevated use of mental health services.
Our study found that the lifetime prevalence of shoplifting is approximately 10% in the U.S. population, lower than estimates in some surveys of adolescents (22 , 23) but similar to other recent national estimates in the adult population (1 , 2) . Failure to use nationally representative samples and validated instruments may have resulted in inflated estimates in the adolescent surveys (22 , 23) . Alternatively, recall bias in the adult surveys may have led to underestimating of past behaviors. The NESARC estimate may represent a lower boundary of the true prevalence of shoplifting.
Shoplifting occurred across all sociodemographic strata. However, it was more common among those with higher education and income, suggesting that financial considerations are unlikely to be the main motivator for shoplifting in most cases. It was also more common among Native Americans and non-Hispanic whites, possibly indicating a racial/cultural dimension not previously documented.
To date, to our knowledge, there are no published reports of the psychopathology associated with shoplifting. We found that shoplifting was associated with a broad range of antisocial behaviors (many of which can also be understood as a manifestation of impulsivity) and, in fact, about one-quarter of individuals with a lifetime history of shoplifting met criteria for antisocial personality disorder. However, removing individuals with antisocial personality disorder from the sample and reanalyzing the data did not alter the direction or strength of our findings, indicating our results were not solely driven by features associated with antisocial personality disorder. Shoplifting was also more common among men and among individuals with other disorders associated with impaired impulse control, such as substance use disorders, bipolar disorder, and pathological gambling, although those associations were weakened after adjustment for the presence of other comorbid psychiatric disorders. Overall, and converging with recent findings in alcohol (24) and drug use disorders (25) , our comorbidity analyses suggest that although a lifetime history of shoplifting is associated with a general vulnerability to psychopathology, that vulnerability is increased for certain disorders. In particular, our findings are most consistent with the understanding of shoplifting as a behavioral manifestation of impaired impulse control and possibly as a symptom of a broader impaired control syndrome with an underlying common factor. Future studies should attempt to delineate the potential boundaries of this syndrome, the phenomenological similarities and genetic overlap of its manifestations, and the unique factors that determine the presence of specific behavioral manifestations in each individual and to identify possible common treatment approaches to behaviors associated with impaired impulse control. Previous work by our group and others has identified the similarities and shared genetics of pathological gambling and substance use disorders (26 – 28) and their response to similar treatments (29 , 30) . This strategy could easily be extended to capture the broader range of behaviors that might encompass this syndrome. Furthermore, shoplifting often occurs at an earlier age than other impulsive behaviors and may serve as a marker to identify individuals at risk for impulse control disorders.
The NESARC did not collect data on obsessive-compulsive disorder, but it did collect data on obsessive-compulsive personality disorder. Although the odds ratios of obsessive-compulsive personality disorder were elevated among individuals with a history of shoplifting compared to nonshoplifters, it was not as strongly associated as antisocial personality disorder or even histrionic personality disorder. Similarly, although the association with bipolar disorder was high, the association of shoplifting with major depressive disorder and dysthymia was substantially weaker, suggesting that shoplifting is unlikely to represent a behavioral manifestation of a broader affective spectrum.
Our study found that although about two-thirds of the cases of shoplifting occur before age 15, over a third of the cases persisted after that age, representing 4% of the adult population. Thus, although in the majority of cases, shoplifting has a limited time course, a substantial proportion of individuals engage in this behavior during their late adolescence or adulthood. A lifetime history of shoplifting appears to be a more important predictor of psychopathology than the age at which shoplifting took place.
Our study also identified higher rates among those with a history of shoplifting of lifetime and past-year use of psychiatric treatment across a broad range of service settings. Participants in the NESARC study were not specifically asked whether they sought treatment for shoplifting but if they sought treatment for any DSM-IV axis I disorder. To the extent that prior reports on kleptomania and other impulse control disorders (5 , 10 , 31) apply to shoplifting per se, prior research suggests that very few individuals seek treatment for shoplifting, and when they seek treatment for other reasons, they are rarely asked about their history of shoplifting. In conjunction with their high rates of comorbidity, the high rates of treatment use found in our study by individuals with a lifetime history of shoplifting are probably best understood as an indicator of the overall severity of their psychopathology. The high rates of mental health service use present opportunities for clinicians to identify individuals with shoplifting problems and provide specific interventions in this regard.
Our study has the limitations common to most large-scale surveys. First, the NESARC did not examine the reliability of individual items. However, the antisocial personality disorder module of the AUDADIS, which contained the shoplifting questions, had a kappa=0.67, which compares favorably with other standardized assessments of antisocial personality disorder (18) . Furthermore, the reliability of the antisocial personality disorder module, as measured by Cronbach’s alpha, is 0.86 and does not change whether or not the shoplifting questions are included in the calculation, supporting the reliability of the shoplifting questions. Second, because the NESARC sample included only civilian households and group quarters populations, information was unavailable on individuals in prison, who may have had higher rates of shoplifting. Third, the assessment of shoplifting was limited to a few questions and did not include information about the frequency or motivation for shoplifting, leaving open the possibility that the behavior occurred only once in the individuals’ lifetime. Even with this broad definition, the results of the study suggest that a lifetime history of shoplifting is strongly associated with high rates of psychopathology and treatment seeking. Future epidemiological studies may benefit from the inclusion of additional questions that may better delineate the epidemiology of shoplifting and examine the similarities and differences of shoplifting and kleptomania in the community. Fourth, this wave of the NESARC did not include assessment of eating disorders or borderline personality disorder, both of which have been associated with a history of shoplifting (32) .
Despite these limitations, the NESARC constitutes the first nationally representative survey to date to include information on shoplifting. Our results suggest that shoplifting is a relatively common behavior and it is associated with substantial rates of psychiatric disorders and psychosocial impairment. High rates of mental health service use were identified in this population. Future research should identify the biological and environmental underpinnings of shoplifting and develop effective screening tools and interventions for individuals with shoplifting problems.
1. National Association of Shoplifting Prevention: www. shopliftingprevention.orgGoogle Scholar
2. Hollinger R, Adams A: 2006 National Retail Survey Final Report. Gainesville, Fla., University of Florida, 2007Google Scholar
3. Merriam-Webster Incorporated: Merriam-Webster Online Dictionary. http://m-w.comGoogle Scholar
4. McElroy SL, Pope HG Jr, Keck PE Jr, Hudson JI, Phillips KA, Strakowski SM: Are impulse-control disorders related to bipolar disorder? Compr Psychiatry 1996; 37:229–240Google Scholar
5. Baylé FJ, Caci H, Millet B, Richa S, Olié JP: Psychopathology and comorbidity of psychiatric disorders in patients with kleptomania. Am J Psychiatry 2003; 160:1509–1513Google Scholar
6. McElroy SL, Pope HG Jr, Hudson JI, Keck PE Jr, White KL: Kleptomania: a report of 20 cases. Am J Psychiatry 1991; 148:652–657Google Scholar
7. Bienvenu OJ, Samuels JF, Riddle MA, Hoehn-Saric R, Liang KY, Cullen BA, Grados MA, Nestadt G: The relationship of obsessive-compulsive disorder to possible spectrum disorders: results from a family study. Biol Psychiatry 2000; 48:287–293Google Scholar
8. Hollander E: Obsessive-Compulsive-Related Disorders. Washington, DC, American Psychiatric Press, 1993Google Scholar
9. Grant J: Kleptomania, in Clinical Manual of Impulse Control Disorders. Edited by Hollander ES. Washington, DC, American Psychiatric Publishing, 2005, pp 175–201Google Scholar
10. Grant JE, Levine L, Kim D, Potenza MN: Impulse control disorders in adult psychiatric inpatients. Am J Psychiatry 2005; 162:2184–2188Google Scholar
11. Grant B, Moore TC, Shepard J, Kaplan K: Source and Accuracy Statement: Wave 1: National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Bethesda, Md, National Institute on Alcohol Abuse and Alcoholism, 2003Google Scholar
12. Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K: Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 2004; 61:807–816Google Scholar
13. Grant BF, Hasin DS, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP: Prevalence, correlates, and disability of personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry 2004; 65:948–958Google Scholar
14. Cottler LB, Grant BF, Blaine J, Mavreas V, Pull C, Hasin D, Compton WM, Rubio-Stipec M, Mager D: Concordance of DSM-IV alcohol and drug use disorder criteria and diagnoses as measured by AUDADIS-ADR, CIDI and SCAN. Drug Alcohol Depend 1997; 47:195–205Google Scholar
15. Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R: The Alcohol Use Disorder and Associated Disabilities Interview Schedule—IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend 2003; 71:7–16Google Scholar
16. Canino G, Bravo M, Ramirez R, Febo VE, Rubio-Stipec M, Fernandez RL, Hasin D: The Spanish Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability and concordance with clinical diagnoses in a Hispanic population. J Stud Alcohol 1999; 60:790–799Google Scholar
17. Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP: The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend 1995; 39:37–44Google Scholar
18. Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R: The Alcohol Use Disorder and Associated Disabilities Interview Schedule—IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend 2003; 71:7–16Google Scholar
19. Ware JE, Kosinski M, Turner-Bowker DM, Gandek B: How to Score Version 2 of the SF-12 Health Survey. Lincoln, RI, Quality Metrics, 2002Google Scholar
20. Research Triangle Institute: Software for Survey Data Analysis (SUDAAN), Version 9.0. Research Triangle Park, NC, Research Triangle Institute, 2004Google Scholar
21. Agresti A: Categorical Data Analysis, 2nd ed. Hoboken, NJ, John Wiley & Sons, 2002Google Scholar
22. Kivivuori J: Delinquent phases: the case of temporally intensified shoplifting behaviour. Br J Criminology 1998; 38:663–680Google Scholar
23. Josephson Institute: The Ethics of American Youth. http://www.josephsoninstitute.org/reportcard/data-tables.htmlGoogle Scholar
24. Hasin DS, Stinson FS, Ogburn E, Grant BF: Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 2007; 64:830–842Google Scholar
25. Compton WM, Thomas YF, Stinson FS, Grant BF: Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 2007; 64:566–576Google Scholar
26. Moreyra P, Ibanez A, Liebowitz MR, Saiz-Ruiz J, Blanco C: Pathological gambling: addiction or obsession? Psychiatr Ann 2002; 32:161–166Google Scholar
27. Petry NM: How treatments for pathological gambling can be informed by treatments for substance use disorders. Exp Clin Psychopharmacol 2002; 10:184–192Google Scholar
28. Slutske WS, Eisen S, True WR, Lyons MJ, Goldberg J, Tsuang M: Common genetic vulnerability for pathological gambling and alcohol dependence in men. Arch Gen Psychiatry 2000; 57:666–673Google Scholar
29. Grant JE, Potenza MN, Hollander E, Cunningham-Williams R, Nurminen T, Smits G, Kallio A: Multicenter investigation of the opioid antagonist nalmefene in the treatment of pathological gambling. Am J Psychiatry 2006; 163:303–312Google Scholar
30. Petry NM, Ammerman Y, Bohl J, Doersch A, Gay H, Kadden R, Molina C, Steinberg K: Cognitive-behavioral therapy for pathological gamblers. J Consult Clin Psychol 2006; 74:555–567Google Scholar
31. Grant JE: Outcome study of kleptomania patients treated with naltrexone: a chart review. Clin Neuropharmacol 2005; 28:11–14Google Scholar
32. Mitchell JE, Fletcher L, Gibeau L, Pyle RL, Eckert E: Shoplifting in bulimia nervosa. Compr Psychiatry 1992; 33:342–345Google Scholar