Brief Interpersonal Psychotherapy for Depressed Mothers Whose Children Are Receiving Psychiatric Treatment
Abstract
Objective: Depressed mothers of children with psychiatric illness struggle with both their own psychiatric disorder and the demands of caring for ill children. When maternal depression remains untreated, mothers suffer, and psychiatric illness in their offspring is less likely to improve. This randomized, controlled trial compared the interpersonal psychotherapy for depressed mothers (IPT-MOMS), a nine-session intervention based on standard interpersonal psychotherapy, to treatment as usual for depressed mothers with psychiatrically ill offspring. Method: Forty-seven mothers meeting DSM-IV criteria for major depression were recruited from a pediatric mental health clinic where their school-age children were receiving psychiatric treatment and randomly assigned to IPT-MOMS (N=26) or treatment as usual (N=21). Mother-child pairs were assessed at three time points: baseline, 3-month follow-up, and 9-month follow-up. Child treatment was not determined by the study. Results: Compared to subjects assigned to treatment as usual, subjects assigned to IPT-MOMS showed significantly lower levels of depression symptoms, as measured by the Hamilton Depression Rating Scale, and higher levels of functioning, as measured by the Global Assessment of Functioning, at 3-month and 9-month follow-ups. Compared to the offspring of mothers receiving treatment as usual, the offspring of mothers assigned to IPT-MOMS showed significantly lower levels of depression as measured by the Children’s Depressive Inventory at the 9-month follow-up. Conclusions: Assignment to IPT-MOMS was associated with reduced levels of maternal symptoms and improved functioning at the 3- and 9-month follow-ups compared to treatment as usual. Maternal improvement preceded improvement in offspring, suggesting that maternal changes may mediate child outcomes.
Major depressive disorder is a common, debilitating illness, affecting one of five women in their lifetime (1) . Many women who suffer from depression are mothers. Because of shared genetic and environmental risk factors, the offspring of depressed mothers have a two- to five-fold increased risk of experiencing a psychiatric illness relative to the offspring of unaffected parents (2 , 3) . In a negatively reinforcing cycle, depressed mothers whose children develop psychiatric illness find it difficult to juggle the mental health treatment needs of multiple affected family members, often putting their own care behind that of their children (4) . Consequently, maternal depression remains untreated (5) , with attendant impairment in a range of functions that have been implicated in both poor maternal and child outcomes, including maternal interpersonal functioning (6 , 7) and parenting skills (8) . Even when children receive psychiatric treatment, the likelihood of favorable responses decreases in the face of persistent maternal depressive symptoms (9) .
Depressed mothers with psychiatrically ill children present both challenges and opportunities. On one hand, if maternal illness is untreated, it is likely to have a negative effect on offspring; on the other hand, when maternal depression is treated, at-risk offspring do better as well (10) . Depression-specific psychotherapies that have demonstrated both efficacy as treatments for syndromal depression (11) , and the capacity to remediate psychosocial impairment (12 – 14) , factors that have been implicated as mediators of child dysfunction (7 , 15) , may represent important treatment options to consider for depressed mothers whose children suffer from psychiatric illness.
Interpersonal psychotherapy for mothers, brief interpersonal psychotherapy for depressed mothers (IPT-MOMS), is a nine-session intervention based on interpersonal psychotherapy for depression (16) with additional modifications designed to help depressed mothers engage in treatment (17) and address relationship difficulties that arise in the context of parenting an ill child (18) . This article describes a randomized, controlled trial of IPT-MOMS as a treatment for major depressive disorder in non-treatment-seeking mothers whose school-age children are receiving psychiatric treatment. The study hypothesized that assignment to IPT-MOMS would be associated with improved outcomes in maternal depressive symptoms and global functioning. A secondary goal was to explore the indirect effects of interpersonal psychotherapy MOMS on offspring with psychiatric illness.
Method
All procedures were approved by the institutional review board of the University of Pittsburgh. After a complete description of the study to the subjects, written informed consent was obtained from 72 potential participants (mothers) during the recruitment period (May 14, 2003, to March 14, 2006). The subjects included mother-child dyads recruited from a general pediatric mental health clinic or from a clinic that specializes in the treatment of suicidal adolescents. A total of 47 subjects (mothers) were deemed eligible for the protocol based on the following criteria: 1) age 18 to 65 years, 2) current diagnosis of major depressive disorder according to DSM-IV criteria, 3) Hamilton Rating Scale for Depression (HAM-D 17-item version) (19) score ≥15, and 4) biological or adoptive mother and custodial parent of a child age 6–18 receiving psychiatric treatment for an internalizing or externalizing disorder. Subjects were excluded from the study if they met any of the following criteria: 1) not currently living with the child, 2) at serious risk for child abuse or neglect, 3) substance abuse within preceding 6 months, 4) actively suicidal, 5) suffering from a psychotic disorder, 6) diagnosis of borderline or antisocial personality disorder, 7) unstable medical condition that could produce symptoms confounding accurate assessment of mood symptoms (e.g., untreated thyroid disease), or 8) currently receiving individual psychotherapy (concurrent treatment with family or group therapy was permitted). Mothers taking antidepressant medications were included if they met entry criteria despite 8 weeks of treatment with stable therapeutic doses of medication. Children gave informed consent or assent after mothers were deemed eligible for inclusion. If multiple children were eligible, the mothers were asked to designate one child participant.
Random Assignment
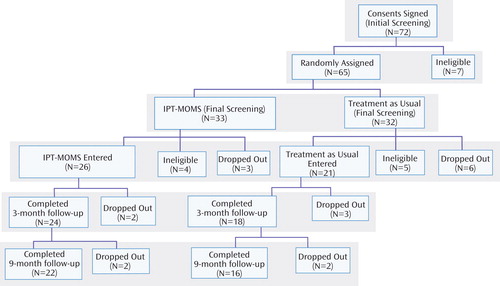
The subjects (N=65) were randomly assigned to either IPT-MOMS or treatment as usual following initial screening procedures that assessed initial severity but did not fully determine eligibility. This permitted investigators to administer the initial engagement session to those assigned to IPT-MOMS at the time of initial contact, a procedure considered essential to the process of working with a difficult-to-engage, non-treatment-seeking population (17) . More thorough screening followed random assignment; therefore, four subjects assigned to IPT-MOMS and five assigned to treatment as usual were ultimately determined to be ineligible for the study. See Figure 1 for a CONSORT subject flow chart. Between random assignment and full determination of eligibility, three subjects assigned to IPT-MOMS and six to treatment as usual dropped out of the study. These differences, although not statistically significant, explain the unequal group sizes of IPT-MOMS and treatment as usual (26 and 21, respectively). Following full determination of eligibility, four subjects assigned to IPT-MOMS and five assigned to treatment as usual did not complete the study (defined as completing the 9-month follow-up assessment).
Assessments
Mothers and children were assessed at baseline and at 3-month and 9-month follow-ups. Maternal lifetime and current psychiatric diagnoses were assigned by using the Structured Clinical Interview for DSM-IV, Clinician Version, for both axis I and II disorders (SCID and SCID II) (20 , 21) . Maternal depressive symptoms were assessed by using the HAM-D 17-item version and the Beck Depression Inventory (BDI) (22) . HAM-D 17-item and BDI total scores range from 0 to 52 and 0 to 63, respectively, with higher scores indicating greater levels of depression severity. Maternal anxiety symptoms were assessed with the Revised Beck Anxiety Inventory (23) , with scores from 10 to 18 indicating symptoms in the mild to moderate range and 19 to 29 indicating in the moderate to severe range. Maternal functioning was assessed using the Global Assessment of Functioning (GAF) (24) and the severity subscale of the Clinical Global Impression Scale (CGI) (25) . GAF range from 0 to 100; scores higher than 90 indicate superior functioning and lower than 70 indicate clinical impairment. The CGI severity subscale consists of a single Likert item ranging from 1 (normal) to 7 (among the most extremely ill patients). SCID I and II were administered by master’s level clinicians in accordance with standards of the Biometrics Division of New York State Psychiatric Institute. Raters were independent from the subjects’ treatment team, and intraclass correlation coefficients were acceptable: 0.80, 0.80, and 0.86 for the HAM-D 17-item version, the GAF, and the CGI, respectively.
Child functioning was assessed with the 13-item child self-report Columbia Impairment Scale (26) , which evaluates four major areas of functioning: interpersonal relations, broad psychopathological domains, functioning in job or schoolwork, and use of leisure time. Items range from 0 (“no problem”) to 4 (“a very big problem”). Scores range from 0 to 52 (lower values indicate lower levels of impairment). Child depressive symptoms were assessed by using the child self-report Children’s Depressive Inventory (27) . These are presented as T scores ranging from 34 (less depressed) to 100 (more depressed), normed separately for ages 7–12 and 13–17. Child psychiatric diagnoses were ascertained by chart review.
IPT-MOMS
ITP-MOMS has been described elsewhere (18) . Briefly, it consists of an initial engagement session based on principles of motivational interviewing and ethnographic interviewing (28) , which is designed to explore and resolve potential barriers to treatment seeking (17 , 29) , followed by eight sessions of brief interpersonal psychotherapy (30) . IPT-MOMS differs from standard interpersonal psychotherapy (16) in that 1) it follows the brief interpersonal psychotherapy model that is both shorter than standard interpersonal psychotherapy and uses some “soft” behavioral strategies to rapidly activate depressed patients (30) , 2) it incorporates a motivational interviewing- and ethnographic interviewing-based engagement session and continues to draw on these engagement strategies as needed during the treatment, and 3) it uses specific strategies to assist mothers in managing problematic interpersonal relationships with their dependent, psychiatrically ill offspring. Sessions were offered to mothers at the same time and in the same location as their child’s mental health visits. Six therapists with master’s or doctoral degrees in social work, nursing, psychology, or medicine (psychiatry) conducted all IPT-MOMS sessions. Sessions were videotaped, and treatment fidelity was assessed by using the Therapy Rating Scale (TRS; 31 , 32) . We rated a subset of tapes (44%) and determined that 98% of those sessions achieved acceptable fidelity in comparison to a designated “gold standard” (≥75% of the mean TRS score of the gold standard therapist). After completing the interpersonal psychotherapy MOMS, the subjects were free to receive additional treatment as needed.
Referral for Treatment as Usual
Subjects assigned to treatment as usual were informed of their diagnoses, given psychoeducational materials, and told to seek treatment. They were given referrals (telephone numbers) to mental health clinics close to their home address and encouraged to avail themselves of services in their communities. Subsequent mental health service use was assessed at the 3-month and 9-month follow-ups by using a structured interview form.
Statistical Analyses
For baseline demographic and clinical characteristics, t tests and chi-square tests were used to compare continuous and categorical variables, respectively. Analyses of covariance, covarying for baseline values, were used to compare groups at follow-up assessments. Tests were considered significant at a=0.05 significance level (two-tailed). Analyses were performed using SAS version 9.1 (33) .
Results
Table 1 shows baseline clinical and demographic features of the group by treatment group. The mean age of the mothers in the total group was 42.7 (SD=8.3), and the mean age of the offspring was 13.8 (SD=3.4, range=6–18). The majority of the group was white (N=37, 79%). The groups did not differ on any demographic variable. All mothers met criteria for major depressive disorder, but over half the subjects also met criteria for additional psychiatric comorbidities. Notably, those assigned to treatment as usual were significantly more likely than those assigned to IPT-MOMS to meet criteria for an additional axis I disorder, most commonly current anxiety disorders (χ 2 =7.4, df=1, p<0.05). There were no other statistically significant differences between groups on baseline clinical variables. Seven mothers assigned to IPT-MOMS and three assigned to treatment as usual were taking antidepressant medications at baseline, but this difference was not statistically significant. Pharmacotherapy remained constant from baseline through the 3-month assessment for those assigned to IPT-MOMS in accordance with the requirements of the protocol. Seventy-six percent (16 of 21) of the treatment as usual subjects reported receiving mental health services from baseline to the 3-month follow-up: nine received both medication and a psychosocial treatment, two received only medication, and five received a psychosocial treatment only. The pharmacotherapy received by the treatment as usual subjects is summarized in Table 2 . Over the 3-month period, the median number of outpatient psychosocial visits attended by the treatment as usual subjects was 4.5, compared to nine IPT-MOMS sessions for those assigned to IPT-MOMS (χ 2 =8.51, df=2, p<0.05).
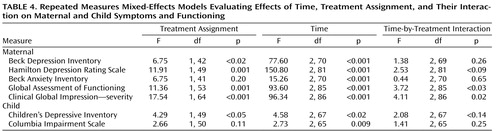
We conducted analyses of covariance to compare mean values of maternal outcome variables at 3- and 9-month follow-ups, controlling for baseline values. As shown in Table 3 , maternal symptom and functioning scores were significantly better in the IPT-MOMS group compared to the treatment as usual group on all measures at each time point with the exception of Beck Anxiety Inventory scores at the 9-month follow-up. Secondary analyses with repeated measures mixed-effects models ( Table 4 ) showed significant time and treatment effects for all measures except the Beck Anxiety Inventory, but significant time-by-treatment interactions for maternal functioning measures only (CGI and GAF scores).
Among offspring of mothers assigned to IPT-MOMS, 52% (N=13) were diagnosed with an internalizing disorder (major depressive disorder, dysthymic disorder, depressive disorder not otherwise specified, social phobia, separation anxiety disorder, or posttraumatic stress disorder), 28% (N=7) with an externalizing disorder (attention deficit hyperactivity disorder, oppositional defiant disorder, or conduct disorder), and 16% (N=4) with both. Among the offspring of treatment as usual mothers, 62% (N=13) were diagnosed with an internalizing disorder, 14% (N=3) with an externalizing disorder, and 19% (N=4) with both. These differences were not statistically significant. There were no significant differences between the groups of offspring on total scores on the Child Behavior Checklist ( Table 3 ).
As shown in Table 3 , at baseline and the 3-month follow-up, there were no differences between groups on measures of child symptoms and functioning. At the 9-month follow-up, however, with the addition of control for baseline values, child self-report depression and functioning (Children’s Depression Inventory and Columbia Impairment Scale) scores were significantly better in the offspring of mothers assigned to IPT-MOMS compared to those assigned to treatment as usual. Using simple linear regressions, we evaluated relationships between percent change in maternal BDI scores from baseline to the 3-month follow-up and child scores at the 9-month follow-up. After adjusting for child scores at the 3-month follow-up, we found significant interactions between percent change in maternal depression scores and treatment assignment for 9-month Children’s Depression Inventory scores (t=2.36, df=19, p=0.03) but not for Columbia Impairment Scale scores, suggesting that acute change in maternal depression may mediate the effect of treatment assignment on child depression over time.
At the 9-month follow-up, 60% (13 of 22) of the subjects completing IPT-MOMS and 100% (16 of 16) of the subjects completing treatment as usual reported receiving mental health treatment between the 3-month and 9-month follow-ups (χ 2 =8.58, df=2, p<0.05). Among IPT-MOMS subjects, seven received both psychotropic medication and psychosocial treatment, three received only medication, and three received psychosocial treatment only. Among treatment as usual subjects, eight received both medication and psychosocial treatment, four only medication, and four only psychosocial treatment. Data supplement tables summarizing pharmacotherapy received by subjects at the 9-month follow-up are available at http://ajp.psychiatryonline.org.
Discussion
This small study had significant limitations, as described below. Nevertheless, data suggest that for depressed mothers whose children are receiving psychiatric treatment, psychotherapy specifically designed to meet their needs results in lower levels of symptoms and higher levels of functioning acutely and at the 9-month follow-up, compared to treatment as usual. In addition, this trial provides preliminary evidence for IPT-MOMS conferring benefit to offspring of depressed mothers, potentially mediated by change in maternal depression.
Recognizing that mothers of ill children rarely attend to their own needs and are, therefore, difficult to engage in treatment (5 , 34 , 35) , IPT-MOMS systematically incorporates strategies to increase the likelihood that subjects will attend sessions: IPT-MOMS therapists systematically explore and address psychological and practical barriers to treatment seeking (17 , 29) , and maternal sessions are coordinated with child sessions. The fact that mothers assigned to IPT-MOMS attended more treatment sessions over a 3-month period compared to mothers assigned to treatment as usual may contribute to the favorable outcomes seen in the IPT-MOMS group and may be an important finding, given the fact that this was predominantly a non-treatment-seeking population.
Although maternal improvement in symptoms and functioning was apparent at the 3-month follow-up, the positive impact of successful maternal treatment on child outcomes was not detectable until the 9-month follow-up. Clinically, we believe that effective IPT-MOMS treatment facilitates improvements in parenting skills, social support use, and management of ongoing interpersonal stressors. That the positive impact of maternal treatment was transmitted to the offspring in a delayed manner would support this hypothesis—i.e., first mothers heal themselves, and then they interact more effectively with their children. Clearly, larger trials will be needed to test this mediational hypothesis.
Our results compare favorably with STAR*D (10) , another study that looked at outcomes in offspring of mothers treated for depression. In both studies, offspring fared better when their mothers’ depression improved. Of interest, in the current trial, 61% (17 of 26) of the mothers initially assigned to IPT-MOMS remitted by the 3-month follow-up (defined as a HAM-D 17-item version score <8), compared with 25% (38 of 151) of the mothers enrolled in STAR*D (and 39% [11 of 21] of the mothers assigned to treatment as usual in the current trial). There are many differences between the two studies, including the fact that the STAR*D participants were treated with medication and not psychotherapy. One possible explanation for the relatively higher remission rates seen with the IPT-MOMS may be that a psychotherapy targeting the specific needs of depressed mothers with ill children may confer advantages beyond pharmacotherapy alone in this population. A properly designed trial would be required to formally test this hypothesis.
There are many limitations to this small study, and it should be replicated to confirm its findings. Most analyses focused on those completing the study, and yet 19% (nine of 47) of the maternal subjects dropped out by the 9-month follow-up, and up to 40% (19 of 47) of child assessments are missing for some measures. Data may not be missing at random. However, there were no differences in the percentages of missing data between the treatment groups at either follow-up assessment, suggesting these effects, even if biased, were similar across groups. In order to address this issue, we conducted secondary analyses of variables using mixed-effects models, techniques that use all available data on all enrolled subjects (36) , and found significant time-by-treatment interactions on measures of maternal functioning. There also appear to be tendencies toward interactions on maternal and child depression scores ( Table 4 ), effects that might have reached statistical significance with larger groups.
The subjects assigned to treatment as usual had more anxiety disorder diagnoses at baseline, a clinical characteristic associated with worse outcomes over time (37) , which may account for observed differences in outcomes between groups. However, there were no differences in baseline levels of anxiety symptoms between groups as measured by the Beck Anxiety Inventory. More subjects assigned to IPT-MOMS were taking antidepressants at study entry than the subjects assigned to treatment as usual, but this number was not statistically significant. Notably, subjects entering the study while taking medication were taking stable doses of antidepressants for at least 8 weeks so that changes in symptoms observed subsequent to entry could be reasonably attributed to the intervention rather than to medications.
Because subjects assigned to IPT-MOMS attended more acute treatment sessions than those assigned to treatment as usual, it is impossible to determine whether favorable outcomes are simply a result of increased session frequency or session content. In addition, subjects in both groups received additional mental health services (both psychotherapy and pharmacotherapy) between 3-month and 9-month assessments, and we did not control for these services in our analyses. Of interest, significantly more treatment as usual than IPT-MOMS completers received treatment in the 3–9 month follow-up interval, and yet those assigned to IPT-MOMS fared better, suggesting enduring effects of acute treatment.
Child outcomes in this trial are considered preliminary because there were few exclusion criteria for children, and, therefore, they carried a wide range of diagnoses, were in different phases of their own treatment, and varied in age. The trial was not adequately powered to disentangle the differential effects of IPT-MOMS across these subgroups of children.
Despite its limitations, this study demonstrates that a high-risk population of non-treatment-seeking depressed mothers with psychiatrically ill offspring who received a brief psychosocial intervention had better outcomes at 3 and 9 months compared to those in treatment as usual. Those assigned to interpersonal psychotherapy MOMS stayed in treatment, achieved substantial clinical gains within a relatively short time, and stayed well over an additional 6 months. Their offspring also seemed to benefit from the mothers’ treatment. Future studies will be needed to replicate these results and to explore factors that mediate effects of maternal treatment outcomes on offspring.

1. Weissman MM, Bland RC, Canino GJ, Faravelli C, Greenwald S, Hwu HG, Joyce PR, Karam EG, Lee CK, Lellouch J, Lépine JP, Newman SC, Rubio-Stipec M, Wells JE, Wickramaratne PJ, Wittchen H, Yeh EK: Cross-national epidemiology of major depression and bipolar disorder. JAMA 1996; 276:293–299Google Scholar
2. Weissman MM, Gammon GD, John K, Merikangas KR, Warner V, Prusoff BA, Sholomskas D: Children of depressed parents: increased psychopathology and early onset of major depression. Arch Gen Psychiatry 1987; 44:847–853Google Scholar
3. Hammen C, Gordon D, Burge D, Adrian C, Jaenicke C, Hiroto D: Maternal affective disorders, illness, and stress: risk for children’s psychopathology. Am J Psychiatry 1987; 144:736–741Google Scholar
4. Nicholson J, Sweeney EM, Geller JL: Mothers with mental illness: I, the competing demands of parenting and living with mental illness. Psychiatr Serv 1998; 49:635–642Google Scholar
5. Swartz HA, Shear MK, Wren FJ, Greeno CG, Sales E, Sullivan BK, Ludewig DP: Depression and anxiety among mothers bringing their children to a pediatric mental health clinic. Psychiatr Serv 2005; 56:1077–1083Google Scholar
6. Zlotnick C, Kohn R, Keitner G, Della Grotta SA: The relationship between quality of interpersonal relationships and major depressive disorder: findings from the National Comorbidity Survey. J Affect Disord 2000; 59:205–215Google Scholar
7. Hammen C, Shih J, Altman T, Brennan PA: Interpersonal impairment and the prediction of depressive symptoms in adolescent children of depressed and nondepressed mothers. J Am Acad Child Adolesc Psychiatry 2003; 42:571–577Google Scholar
8. Susman EJ, Trickett PK, Iannotti RJ, Hollenbeck BE, Zahn-Waxler C: Child-rearing patterns in depressed, abusive, and normal mothers. Am J Orthopsychiatry 1985; 55:237–251Google Scholar
9. Brent DA, Kolko DJ, Birmaher B, Baugher M, Bridge J, Roth C, Holder D: Predictors of treatment efficacy in a clinical trial of three psychosocial treatments for adolescent depression. J Am Acad Child Adolesc Psychiatry 1998; 37:906–914Google Scholar
10. Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, Hughes CW, Garber J, Malloy E, King CA, Cerda G, Sood AB, Alpert JE, Trivedi MH, Rush AJ, STAR*D-Child Team: Remissions in maternal depression and child psychopathology: a STAR*D child report. JAMA 2006; 295:1389–1398Google Scholar
11. Elkin I, Shea T, Watkins JT, Imber ST, Sotsky SM, Collins JF, Glass DR, Pilkonis PA, Leber WR, Docherty JP, Fiester SJ, Parloff MB: National Institute of Mental Health Treatment of Depression Collaborative Research Program: general effectiveness of treatments. Arch Gen Psychiatry 1989; 46:971–982Google Scholar
12. Jarrett RB, Rush AJ: Short-term psychotherapy of depressive disorders: current status and future directions. Psychiatry 1994; 57:115–132Google Scholar
13. Klerman GL, Dimascio A, Weissman M, Prusoff B, Paykel ES: Treatment of depression by drugs and psychotherapy. Am J Psychiatry 1974; 131:186–191Google Scholar
14. Weissman MM, Klerman GL, Paykel ES, Prusoff BA, Hanson B: Treatment effects on the social adjustment of depressed patients. Arch Gen Psychiatry 1974; 30:771–778Google Scholar
15. Hammen C, Shih JH, Brennan PA: Intergenerational transmission of depression: test of an interpersonal stress model in a community sample. J Consult Clin Psychol 2004; 72:511–522Google Scholar
16. Weissman MM, Markowitz JC, Klerman GL: Comprehensive Guide to Interpersonal Psychotherapy. New York, Basic Books, 2000Google Scholar
17. Swartz HA, Zuckoff A, Grote NK, Spielvogle HN, Bledsoe SE, Shear MK, Frank E: Engaging depressed patients in psychotherapy: integrating techniques from motivational interviewing and ethnographic interviewing to improve treatment participation. Prof Psychol Res Pr 2007; 38:430–439Google Scholar
18. Swartz HA, Zuckoff A, Frank E, Spielvogle HN, Shear MK, Fleming MA, Scott J: An open-label trial of enhanced brief interpersonal psychotherapy in depressed mothers whose children are receiving psychiatric treatment. Depress Anxiety 2006; 23:398–404Google Scholar
19. Hamilton M: A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 25:56–62Google Scholar
20. First M, Spitzer R, Gibbon M, Williams J: Structured Clinical Interview for DSM-IV Axis I Disorders (SCID). New York, New York State Psychiatric Institute, Biometrics Research, 1995Google Scholar
21. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Personality Disorders (SCID-II). Washington, DC, American Psychiatric Press, 1997Google Scholar
22. Beck AT, Steer RA: Manual for the Beck Depression Inventory. San Antonio, Tex, Psychological Corporation, 1993Google Scholar
23. Beck AT, Steer RA: Manual for the Revised Beck Anxiety Inventory. San Antonio, Tex, Psychological Corporation, 1990Google Scholar
24. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders (4th ed). Washington, DC, American Psychiatric Association, 1994Google Scholar
25. Guy W: ECDEU Assessment Manual for Psychopharmacology. Rockville, Md, National Institute for Mental Health, US Department of Health, Education, and Welfare, 1976, pp 218–222Google Scholar
26. Bird HR, Shaffer D, Fisher P, Gould M, Staghezza B, Chen J, Hoven C: The Columbia Impairment Scale (CIS): pilot findings on a measure of global impairment for children and adolescents. Int J Methods Psychiatr Res 1993; 3:167–176Google Scholar
27. Kovacs M: Children’s Depression Inventory Manual. North Towanda, NY, Multi-Health Systems, 1992Google Scholar
28. Schensul SL, Schensul JJ, LeCompte MD: Essential Ethnographic Methods: Observations, Interviews, and Questionnaires: Ethnographer’s Toolkit 2. Walnut Creek, Calif, Alta Mira Press, 1999Google Scholar
29. Zuckoff A, Swartz HA, Grote NK: Motivational interviewing as a prelude to psychotherapy of depression, in Motivational Interviewing in the Treatment of Psychological Problems. Edited by Arkowitz H, Westra HA, Miller WR, Rollnick S. New York, Guilford, 2007, pp 109–144Google Scholar
30. Swartz HA, Frank E, Shear MK, Thase ME, Fleming MAD, Scott J: A pilot study of brief interpersonal psychotherapy for depression in women. Psychiatr Serv 2004; 55:448–450Google Scholar
31. Wagner EF, Frank E, Steiner S: Discriminating maintenance treatments for recurrent depression: development and implementation of a rating scale. J Psychother Pract Res 1992; 1:280–290Google Scholar
32. Frank E, Kupfer DJ, Wagner EF, McEachran AB, Cornes C: Efficacy of interpersonal psychotherapy as a maintenance treatment of recurrent depression: contributing factors. Arch Gen Psychiatry 1991; 48:1053–1059Google Scholar
33. SAS Institute Inc: SAS OnlineDoc, version 9. Cary, NC, SAS Institute Inc, 2000Google Scholar
34. Verdeli H, Ferro T, Wickramaratne P, Greenwald S, Blanco C, Weissman MM: Treatment of depressed mothers of depressed children: pilot study of feasibility. Depress Anxiety 2004; 19:51–58Google Scholar
35. Ferro T, Verdeli H, Pierre F, Weissman MM: Screening for depression in mothers bringing their offspring for evaluation or treatment of depression. Am J Psychiatry 2000; 157:375–379Google Scholar
36. Littell RC, Milliken GA, Stroup WW, Wolfinger RD, Schabenberger O: SAS for Mixed Models, 2nd ed. Cary, NC, SAS Institute Inc, 2006Google Scholar
37. Feske U, Frank E, Kupfer DJ, Shear MK, Weaver E: Anxiety as a predictor of response to interpersonal psychotherapy for recurrent major depression: an exploratory investigation. Depress Anxiety 1998; 8:135–141Google Scholar