A Randomized, Controlled Proof-of-Concept Trial of an Internet-Based, Therapist-Assisted Self-Management Treatment for Posttraumatic Stress Disorder
Abstract
Objective: The authors report an 8-week randomized, controlled proof-of-concept trial of a new therapist-assisted, Internet-based, self-management cognitive behavior therapy versus Internet-based supportive counseling for posttraumatic stress disorder (PTSD). Method: Service members with PTSD from the attack on the Pentagon on September 11th or the Iraq War were randomly assigned to self-management cognitive behavior therapy (N=24) or supportive counseling (N=21). Results: The dropout rate was similar to regular cognitive behavior therapy (30%) and unrelated to treatment arm. In the intent-to-treat group, self-management cognitive behavior therapy led to sharper declines in daily log-on ratings of PTSD symptoms and global depression. In the completer group, self-management cognitive behavior therapy led to greater reductions in PTSD, depression, and anxiety scores at 6 months. One-third of those who completed self-management cognitive behavior therapy achieved high-end state functioning at 6 months. Conclusions: Self-management cognitive behavior therapy may be a way of delivering effective treatment to large numbers with unmet needs and barriers to care.
Cognitive behavior therapy for posttraumatic stress disorder (PTSD) entails a set of strategies designed to help trauma survivors understand and manage symptoms, correct maladaptive cognitions, and process trauma memories therapeutically (1) . Although it has been shown to be efficacious (2 , 3) , cognitive behavior therapy is not widely available nor routinely employed (4) . In addition, cognitive behavior therapy requires significant professional training and expertise to administer, as well as patient time and resources. Consequently, there is ample justification for considering self-management and telehealth-based treatments to enhance treatment fidelity, effectiveness, and accessibility (5) . We conducted a randomized, controlled proof-of-concept trial of a therapist-assisted, Internet-delivered self-management cognitive behavior therapy (6) and a comparison condition comprising Internet-based supportive counseling. If cognitive behavior therapy can be efficiently deployed and conveniently delivered, it can be more accessible and widely disseminated, especially to individuals who experience various barriers to care.
Method
Participants
The patients were Department of Defense service members in the Washington, D.C., area who had PTSD as a result of the Pentagon attack on September 11th or combat in Iraq/Afghanistan. Exclusion criteria were 1) active substance dependence, 2) current suicidal ideation, 3) history of psychotic disorder, 4) <21 or >65 years of age, 5) PTSD or depression immediately before the trauma, 6) current psychiatric treatment, 7) marked ongoing stressors, and 8) inadequate social supports. Medications varied but were stable and maintained.
The participants were recruited through advertisements and presentations at Department of Defense sites. One hundred forty-one participants were screened; 41 were ineligible, 31 did not consent, and 26 could not be contacted for assessment. Forty-five participants were randomly assigned, and 33 completed treatment. Five patients dropped out after random assignment but before treatment; seven dropped out during treatment; 24 patients completed the 3-month follow-up, and 18 completed the 6-month follow-up (some service members were hard to locate). There were no differences in dropouts between the two study arms overall (likelihood ratio=1.19, df=1, N=45, p>0.05; at posttreatment: likelihood ratio=0.40, df=1, N=45, p>0.05) or at the 3-month (likelihood ratio=1.75, df=1, N=45, p>0.05) and 6-month follow-ups (likelihood ratio=0.43, df=1, N=45, p>0.05). Treatment arms did not differ in trauma type (likelihood ratio=1.99, df=1, N=45, p>0.05) (56% September 11th; 44% combat).
Completers were not different from noncompleters on gender (likelihood ratio=4.31, df=1, N=45), minority status (likelihood ratio=0.04, df=1, N=45), or baseline anxiety (t=1.01, df=45). Noncompleters were significantly older (t=2.18, df=43, p<0.05; 40.82 years old, versus 34.75 for completers) and more likely enlisted (likelihood ratio=4.59, df=1, N=43, p<0.05).
There were no differences in any variable between those who completed the posttreatment or 3-month follow-up assessments. In the self-management cognitive behavior therapy arm, those with 6-month follow-up data had higher socioeconomic status (t=2.09, df=22, p<0.05), lower baseline anxiety (t=3.23, df=21, p<0.01), and lower baseline PTSD scores (t=2.60, df=22, p<0.05), similar to other published studies (7) . There were no differences between completers and noncompleters within the supportive counseling arm at both follow-up intervals.
Measures
Online ratings
At each log on, service members were required to make ratings of their PTSD symptoms with a modified PTSD checklist (8 , 9) and a global rating of their level of depression on a scale of 1–10 before they were allowed to proceed with that particular log on’s activities. The PSTD Checklist evaluated the severity of PTSD symptoms in the last 24 hours with Likert-type scaling from 1=not at all to 5=extremely. The PTSD Checklist items employed were the following:
Repeated disturbing memories, thoughts, or images of events surrounding your traumatic experience
Repeated disturbing dreams of upsetting events surrounding your traumatic experience
Feeling very upset and stressed (e.g., heart pounding, trouble breathing, sweating) when something reminded you of your stressful experience or events surrounding the traumatic experience
Avoiding thinking about or talking about your traumatic experience or avoiding having feelings related to these events
Avoiding activities or situations because they reminded you of your stressful experience or events surrounding the traumatic experience
Trouble falling asleep or staying asleep since your traumatic experience
Feeling irritable or having angry outbursts since your traumatic experience
The global depression item was worded in the following manner: “On a scale of 1–10, please rate how depressed, down, or lethargic you have felt in general over the last 24 hours (1=not at all depressed, 10=severe incapacitating depression).” The repeated log-on assessments of PTSD symptoms and global depression were used to track outcome and to monitor clinical status. Study therapists were automatically notified if the patients endorsed depression item 7 or above. In addition, the therapists monitored the patients’ daily symptom reports by logging on to a special back end to the website (the back end also allowed therapists to review homework submissions and to determine time since last log on).
Baseline and follow-up assessment measures
The study therapists conducted the baseline assessments in order to initially establish rapport. Clinicians blind to study arm conducted the follow-up evaluations. The primary outcome measure was the PTSD Symptom Scale—Interview Version (10) , which is a structured interview that asks participants to rate how much they were bothered by each of the PTSD symptoms specified in DSM-IV, ranging from 0 (never) to 3 (five times per week or more), yielding a sum score measuring overall PTSD symptom severity. Internal consistencies ranged from a=0.76 to 0.92, and the scale has been found to have excellent diagnostic utility.
Depression symptoms were assessed with the 21-item Beck Depression Inventory—II (11) . The participants rated the severity of each symptom (e.g., sadness, worthlessness) on a 4-point scale ranging from 0 (not at all) to 3 (severely), and scores were summed to form an overall composite score. The Beck Depression Inventory—II is used widely to assess symptoms of depression among clinical and normal populations and has shown to be a reliable and valid measure in several investigations of treatment outcome studies of combat-related PTSD (12 , 13) . Anxiety symptoms were measured with the Beck Anxiety Inventory (14) . The Beck Anxiety Inventory is a 21-item self-report measure. Like the Beck Depression Inventory, symptom ratings range from 0 to 3, which are summed for a total anxiety score. The Beck Anxiety Inventory has been used in many PTSD outcome studies with combat-related PTSD (15) . Cronbach’s alpha for the Beck Depression Inventory—II and the Beck Anxiety Inventory range from 0.90 to 0.94.
Procedure
The participants provided written informed consent. They were evaluated at baseline, after treatment, and at 3 and 6 months after baseline. Each intervention arm was therapist-assisted and Internet-delivered and lasted 8 weeks, with 56 total possible log ons (daily). At each log on, the participants made online symptom ratings, reported homework compliance and homework content, acquired new content (or content was restated), and received a new homework assignment.
At baseline, each patient had an approximately 2- hour face-to-face meeting with the study therapist who, in addition to conducting the initial evaluation, introduced the study and intervention procedures; provided psychoeducation about PTSD and the benefits of stress management, a unique log-on ID, and password; and demonstrated the respective Internet sites. The patients in both arms also had periodic and ad lib study therapist contact via e-mail and telephone (they could also request a call back or an e-mail message from their therapist).
Study Interventions
Two highly specialized web applications were developed to automatize the delivery of the two interventions, collect outcome and process data (e.g., compliance), and assist study therapists and their supervisors to monitor patient participation (e.g., homework compliance). On each web site, patients had ad lib access to educational information about PTSD, stress, and trauma, as well as common comorbid problems and symptoms they might experience (e.g., depression, survivor guilt). The participants were also provided unrestricted access to information on strategies to manage their anger and sleep hygiene.
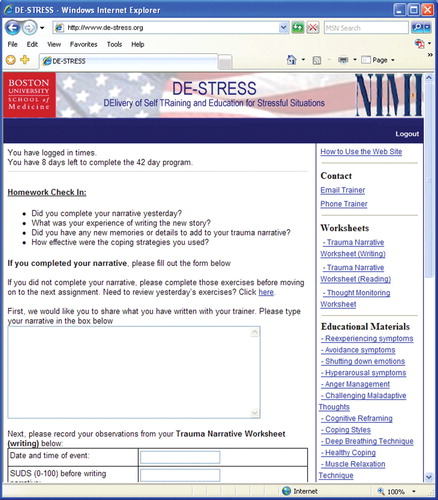
In order to reduce stigma and to emphasize the self-care aspects of the self-management cognitive behavior therapy, we employed the following title: DElivery of Self-TRraining and Education for Stressful Situations or DE-STRESS. The DE-STRESS acronym was particularly well received in the military context and by patients.
Internet-delivered self-management cognitive behavior therapy
The self-management cognitive behavior therapy was designed to teach patients strategies to help them cope and manage their reactions to situations that triggered recall of traumatic experiences (and negative affect and arousal). The intervention taught, promoted, and prompted stress and negative affect management strategies applied to a personalized hierarchy of trauma triggers (stressful contexts) through a series of homework assignments. The goal was to reduce PTSD symptom burden and to promote greater self-efficacy and confidence in coping capacities. The specific components of the self-management cognitive-behavior therapy were the following:
Self-monitoring of situations that triggered trauma-related distress (first 2 weeks)
The generation of a serial ordering (hierarchy) of these trigger contexts in terms of their degree of threat or avoidance (starting week three)
Didactics on stress management strategies that, once practiced (starting day 1), were used for
Graduated, self-guided, in vivo exposure to items from the personalized hierarchy (starting with the least threatening or least avoided item in week 3
Seven online trauma writing sessions (week 7, see below)
A review of progress (charts of daily symptom reports were presented), a series of didactics on relapse prevention, and the generation of a personalized plan for future challenges (week 8)
In the initial meeting with the study therapist, an initial hierarchy of stressful situations was generated collaboratively. It was assumed that most patients with PTSD are not sufficiently aware of what triggers the recall of trauma memories. As a result, in the first 2 weeks, the patients were asked to monitor their reactions to various stressful and demanding situations. After this period, the therapists assisted the patients in generating a final personalized stress hierarchy (with e-mail).
In the face-to-face session, the study therapists also provided initial training in two stress-management strategies (deep, slow diaphragmatic breathing and simple, progressive muscle relaxation) and initial training in simple cognitive reframing techniques (how to challenge unhelpful thought patterns and alter self-talk to effectively manage demanding situations). Subsequently, homework assignments were given online to further acquire these skill sets (e.g., see Figure 1 ).

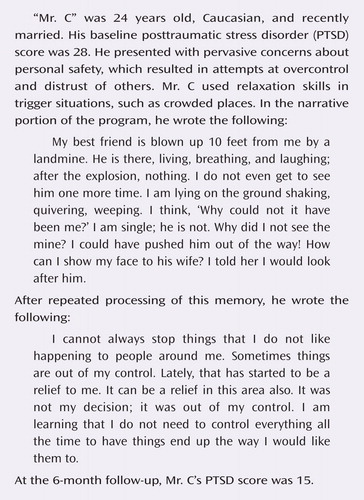
At the end of week 6, the study therapists had a planned phone conversation with the patients to determine if they were ready to do the trauma narrative portion of the self-management cognitive behavior therapy (no patients were deemed incapable or ineligible). In week 7, the participants were asked to write (type) a detailed first-person, present-tense account of a particularly salient and troubling traumatic experience. They were then asked to read their trauma narrative and encouraged to experience any emotions or memories that they may have been avoiding, while using coping skills acquired in the program. In the subsequent six log ons, the patients were asked to rewrite and process their traumatic memory, including any other memories that might not have occurred to them initially. The writing task is a variant of techniques employed in cognitive behavior therapy and cognitive processing therapy to target PTSD (13 , 16) . The goal was to promote mastery and to reduce avoidance, as opposed to maximizing emotional processing to promote extinction, as is the case in exposure therapy (2) .
Internet-delivered supportive counseling
The majority of the supportive counseling intervention entailed participants being asked to self-monitor daily nontrauma -related concerns and hassles and online writing about these experiences. Psychoeducation materials were available about the psychological, emotional, and cognitive effects of trauma, but there was no skills training or prescriptions for proactive action. The supportive counseling group was asked to visit the web site daily to report their symptoms, read about stress and stress management, and write about current concerns. The web site allowed the participants to ask for an immediate telephone call from their therapists, and they were called periodically by their study therapist to check in on how they were doing and to answer any questions they might have about the self-help program. Through e-mail and the telephone, supportive counseling therapists were instructed to be empathic and validating, nondirective and supportive, and to focus on non-trauma-related present-day concerns. In week 8, patients in the supportive counseling arm were asked to plan ways of using what they learned in the course of the therapy from that point forward and to plan for future stressors; they also were shown graphs of the course of their progress (symptom reporting).
Analysis Plan
Online ratings
We used hierarchical linear modeling (17) to analyze models of individual change or growth in the online PTSD and depression symptom ratings over the 56 (possible) repeated ratings by intervention group. The advantage of using hierarchical linear modeling is the ability to account for all of the 56 possible repeated measures and the ability to use an expectation-maximization algorithm for full maximum likelihood estimation of missing data during model fit (18) .
We used a two-level hierarchical linear model to analyze online symptom ratings across the repeated online assessments (level 1) and to determine if the slope was related to the intervention arm (level 2) in the intent-to-treat group. In these analyses, the level 1 model specifying change or growth rate in symptoms (Y) for person i at time t was: Y ti =b 0i +b 1i (Time)+e ti . In this equation, b 0i represents the average level of adjustment at a specific time and b 1i represents the expected change in a fixed period of time. In these analyses, the unit of time was one day. To examine the effect of intervention arm on symptom ratings over time on level 2, we used the model-building approach, with the augmented models as follows: b 0i =g 00 +g 01 (intervention arm)+m 0i ; b 1i =g 10 +g 11 (intervention arm)+m 1i .
Assessment measures
We used repeated-measures analysis of covariance (ANCOVA), with baseline outcome scores as the covariate, to compare improvement over time in each arm. We also conducted planned comparisons examining a priori hypotheses that the active intervention (self-management cognitive behavior therapy) would lead to greater change in symptoms and clinical outcomes. All analyses were conducted on the intent-to-treat and completer groups.
Results
Participant Characteristics
There were no pretreatment differences between the two arms demographically or in baseline levels of depression, anxiety, or PTSD symptoms (see Table 1 ). Supportive counseling participants (mean=41.05, SD=20.10) logged on more often than self-management cognitive behavior therapy participants (mean=23.63, SD=17.52) (t=3.11, df=43, p<0.01). The two arms did not differ on time spent in treatment (t=1.35, df=39, p>0.10) (supportive counseling: mean=46.76 days, SD=24.03; self-management cognitive behavior therapy: mean=36.92 days, SD=22.84) or in average days between sessions (t=–1.43, df=39, p>0.10) (supportive counseling: mean=1.23 days, SD=0.66; self-management cognitive behavior therapy: mean=1.60 days, SD=0.98).
Online Symptom Reports
For both arms, mean total PTSD symptoms, criterion C avoidance, and criterion D hyperarousal symptom ratings declined over the course of treatment (γ 10 =–0.02, p<0.001, γ 10 =–0.003, p<0.001, and γ 10 =–0.004, p<0.001, respectively). However, patients in the self-management cognitive behavior therapy arm had a sharper decline in mean total PTSD symptom severity, γ 11 =–0.02, p<0.001; avoidance, γ 11 =–0.003, p<0.05; and hyperarousal symptoms, γ 11 =–0.007, p<0.001. PTSD criterion B reexperiencing symptom ratings did not decrease significantly across treatment (γ 10 =–0.0004, p>0.10), nor were there differential treatment effects (γ 11 =0.004, p>0.10). Global depression ratings decreased significantly over treatment (γ 10 =–0.01, p>0.10). In addition, the self-management cognitive behavior therapy group had marginally significant higher depression scores (γ 01 =1.00, p=0.08) but a significantly sharper decline in depression symptoms relative to the supportive counseling arm (γ 11 =–0.007, p<0.01). Analysis of the online symptom ratings for the completer group produced similar results although no differences in depression ratings.
Assessment Data
The patients in each arm improved over time for the intent-to-treat and completer groups (see Table 1 ). Repeated-measures ANCOVAs, with baseline scores as the covariate, revealed a significant main effect of time for total PTSD interview scores (F=25.26, df=1, 43, p<0.001), depression (F=7.13, df=1, 40, p<0.001), and anxiety (F=14.58, df=1, 38, p<0.001).
For the intent-to-treat and completer groups, at the 3-month follow-up, there were no significant differences in the two arms on any outcome. However, for the completers, at the 6-month follow-up, the self-management cognitive behavior therapy arm had significantly lower depression (t=2.15, df=16, p<0.05), anxiety (t=2.06, df=16, p=0.06), and total PTSD symptoms (t=2.02, df=16, p=0.06) ( Figure 2 ).The controlled effect sizes (self-management cognitive behavior therapy relative to supportive counseling) for these changes were d=1.03, d=1.01, and d=0.95, respectively. Also, in the completer group, a greater percentage of cases in the self-management cognitive behavior therapy arm no longer met criteria for PTSD (operationalized as a PTSD Symptom Scale—Interview Version score below 6) compared to the supportive counseling arm at posttreatment and the 6-month follow-up ( Table 1 ). A significantly greater percentage of self-management cognitive behavior therapy cases in the intent-to-treat group no longer met criteria for PTSD compared to the supportive counseling arm at posttreatment (likelihood ratio=3.89, df=1, N=45, p<0.05) (25% versus 5%) and at the 6-month follow-up (likelihood ratio=8.35, df=1, N=45, p<0.01) (25% versus 3%). With respect to high end-state functioning(19) (Beck Depression Inventory—II and Beck Anxiety Inventory scores <12 and PTSD Symptom Scale—Interview Version scores <6) in the completer group, the two arms differed at posttreatment (self-management cognitive behavior therapy=29% versus supportive counseling=0%) (likelihood ratio=6.81, df=1, N=30, p<0.01) and at the 6-month follow-up interval (self-management cognitive behavior therapy=33% versus supportive counseling=0%) (likelihood ratio=4.76, df=1, N=18, p<0.05). Finally, also with respect to high end-state functioning in the intent-to-treat group, the two arms differed at the 3-month follow-up (self-management cognitive behavior therapy=25% versus supportive counseling=0%) (likelihood ratio=8.35, df=1, N=45, p<0.01) and at the 6-month follow-up interval (self-management cognitive behavior therapy=25% versus supportive counseling=0%) (likelihood ratio=8.35, df=1, N=45, p<0.01).
Discussion
Intent-to-treat analyses of online symptom reporting and indicators of end-stage functioning, as well as completer analyses of other outcome data, indicated that participants who received self-management cognitive behavior therapy reported greater gains than those who received supportive counseling. One-third of those who completed self-management cognitive behavior therapy achieved high end-state functioning 6 months after treatment (one-quarter of the intent-to-treat group). The intervention was tolerated well, and the dropout rate was similar to that of face-to-face trials. Because many military and emergency service personnel with PTSD often do not receive evidence-based treatment (20) , these initial results point to a potentially viable means to deliver rapid and effective PTSD treatment to a large population with otherwise unmet needs for PTSD care.
These results are somewhat tempered by the fact that younger and more symptomatic service members were less likely to be located at 6 months (they were arguably more likely to be redeployed). Also, there was a tendency for fewer people to complete self-management cognitive behavior therapy than supportive counseling, and future research should study factors that enhance web usage for cognitive behavior therapy.
We recognize that our pilot study had a small group size, which limits the generalizability of the findings and reduces power to detect moderators of treatment outcome. Nevertheless, these promising results suggest the need for future research into Internet-based therapies to assist patients with PTSD. Self-management cognitive behavior therapy is a potential solution to the demand for efficient, low-cost, and stigma-reducing interventions for traumatic stress, especially in the military, in disaster contexts, and in the emergency services. This approach should be considered (and evaluated) within a tiered system of self-management approaches, ranging from an Internet-based companion to face-to-face treatment to guide and systematize cognitive behavior therapy components to free up therapists’ time and resources to a completely self-help approach by means of the Internet, DVDs, or booklets.
1. Keane TA, Barlow DH: Posttraumatic stress disorder, in Anxiety and Its Disorders: The Nature and Treatment of Anxiety and Panic, 2nd Ed. Edited by Barlow DH. New York, Guilford, 2002, pp 418–453Google Scholar
2. Rothbaum BO, Meadows EA, Resick P, Foy DW: Cognitive-behavioral therapy, in Effective Treatments for PTSD: Practice Guidelines from the International Society for Traumatic Stress Studies. Edited by Foa EB, Keane TM, Friedman MJ. New York, Guilford, 2000, pp 60–83Google Scholar
3. Litz BT, Bryant R: Early intervention for trauma in adults: cognitive-behavioral therapy, in Effective Treatments for PTSD: Practice Guidelines from the International Society for Traumatic Stress Studies (2nd ed). Edited by Foa E, Friedman M, Keane T, Cohen J. New York, Guilford (in press)Google Scholar
4. Zayfert C, Deviva JC, Becker CB, Pike JL, Gillock KL, Hayes SA: Exposure utilization and completion of cognitive behavioral therapy for PTSD in a “real world” clinical practice. J Trauma Stress 2005; 18:637–645Google Scholar
5. Taylor CB, Luce KH: Computer- and Internet-based psychotherapy interventions. Curr Dir Psych Science 2003; 12:18–22Google Scholar
6. Litz BT, Williams L, Wang J: A therapist-assisted Internet self-help program for traumatic stress. Prof Psych Res Prac 2004; 35:628–634Google Scholar
7. Bryant RA, Moulds ML, Nixon RD: Cognitive behaviour therapy of acute stress disorder: a four-year follow-up. Behav Res Ther 2003; 41:489–494Google Scholar
8. Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM: The PTSD Checklist (PCL). Boston, National Center for PTSD, 1993Google Scholar
9. Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA: The psychometric properties of the PTSD checklist (PCL). Behav Res Ther 1996; 34:669–673Google Scholar
10. Foa EB, Tolin DF: Comparison of the PTSD Symptom Scale—Interview Version and the Clinician-Administered PTSD Scale. J Trauma Stress 2000; 13:181–191Google Scholar
11. Beck AT, Steer RA, Brown GK: Beck Depression Inventory Manual, 2nd Ed. San Antonio, Tex, Psychological Corporation, 1996Google Scholar
12. Bolton EE, Lambert JF, Wolf EJ, Raja S, Varra AA, Fisher LM: Evaluating a cognitive-behavioral group treatment program for veterans with posttraumatic stress disorder. Psychiatr Serv 2004; 1:140–146Google Scholar
13. Monson CM, Schnurr PP, Resick P, Friedman MJ, Young-Xu Y, Stevens SP: Cognitive processing therapy for veterans with military-related posttraumatic stress disorder . J Consult Clin Psychol 2006; 74:898–907Google Scholar
14. Beck AT, Epstein N, Brown G, Steer RA: An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1998; 56:893–897Google Scholar
15. Rothbaum BO, Ruef AM, Litz BT, Han H, Hodges L: Virtual reality exposure therapy of combat-related PTSD: a case study using psychophysiological indicators of outcome . J Cogn Psychotherapy 2003; 17:163–177Google Scholar
16. Taylor S: Clinicians’ Guide to PTSD: A Cognitive Behavioral Approach. New York, Guilford, 2006Google Scholar
17. Bryk AS, Raudenbush SW: Hierarchical Linear Models: Applications and Data Analysis Methods. Newbury Park, Calif, Sage Publications, 1992Google Scholar
18. Schafer JL, Graham JW: Missing data: our view of the state of the art. Psychol Methods 2002; 7:147–177Google Scholar
19. Ehlers A, Clark DM, Hackmann A: A randomized controlled trial of cognitive therapy, a self-help booklet, and repeated assessments as early interventions for posttraumatic stress disorder. Arch Gen Psychiatry 2003; 60:1024–1032Google Scholar
20. Hoge CW, Auchterlonie JL, Milliken CS: Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA 2006; 296:1023–1032Google Scholar




