Epidemiology and Course of Anorexia Nervosa in the Community
Abstract
Objective: Most previous studies of the prevalence, incidence, and outcome of anorexia nervosa have been limited to cases detected through the health care system, which may bias our understanding of the disorder’s incidence and natural course. The authors sought to describe the onset and outcomes of anorexia nervosa in the general population. Method: Lifetime prevalences, incidence rates, and 5-year recovery rates of anorexia nervosa were calculated on the basis of data from 2,881 women from the 1975–1979 birth cohorts of Finnish twins. Women who screened positive for eating disorder symptoms (N=292), their screen-negative female co-twins (N=134), and 210 randomly selected screen-negative women were assessed for lifetime eating disorders by telephone by experienced clinicians. To assess outcomes after clinical recovery and to detect residua of illness, women who had recovered were compared with their unaffected co-twins and healthy unrelated women on multiple outcome measures. Results: The lifetime prevalence of DSM-IV anorexia nervosa was 2.2%, and half of the cases had not been detected in the health care system. The incidence of anorexia nervosa in women between 15 and 19 years of age was 270 per 100,000 person-years. The 5-year clinical recovery rate was 66.8%. Outcomes did not differ between detected and undetected cases. After clinical recovery, the residua of illness steadily receded. By 5 years after clinical recovery, most probands had reached complete or nearly complete psychological recovery and closely resembled their unaffected co-twins and healthy women in weight and most psychological and social measures. Conclusions: The authors found a substantially higher lifetime prevalence and incidence of anorexia nervosa than reported in previous studies, most of which were based on treated cases. Most women recovered clinically within 5 years, and thereafter usually progressed toward full recovery.
Anorexia nervosa is a severe psychiatric disorder that mainly affects adolescent girls and young women (1 – 3) . Although the disorder was first described centuries ago, its risk factors, etiology, and course remain poorly understood (1 – 3) .
Numerous studies have assessed the prevalence of anorexia nervosa (4 , 5) . Estimates of prevalence are influenced by the number of new-onset cases, but also by duration of illness, methods of case detection, and the age of study participants (6) . Counting new-onset cases only, that is, calculating the incidence, is a more accurate approach to comparing rates of illness across communities and time periods and is essential for rigorous investigations of the etiology and course of illness (6) . Despite this, few studies have examined the incidence of anorexia nervosa. Those that have been reported (7 – 9) reflect the difficulty of addressing relatively rare disorders: either they are limited to cases detected in health care settings or they lack statistical power because of small sample sizes. Nevertheless, they document a steady increase in the incidence of anorexia nervosa among 15- to 19-year-old women since the 1930s (9 – 11) .
Long-term follow-up studies of anorexia nervosa are few and primarily reflect clinical case series or studies based on clinical catchment areas (12 – 14) . They suggest that anorexia nervosa tends to have a chronic course and carries a high risk of mortality (about 5.6% per decade) (15 – 17) . However, as it has been estimated that only half of cases of anorexia nervosa are detected in primary care settings (18) and only one-third of the community cases are treated in mental health care settings (5) , the natural course of the illness remains poorly understood.
Our aim was to describe the onset and outcomes of anorexia nervosa in the general population. Using the nationwide population-based 1975–1979 birth cohorts of Finland, we examined the incidence and lifetime prevalence of anorexia nervosa among twins. To better understand the impact of anorexia on young women’s lives, we also compared the behavioral, psychological, and social outcomes of women with anorexia nervosa with those of their unaffected co-twins and unrelated healthy women.
Method
The “FinnTwin 16” Birth Cohorts
Study subjects were Finnish twins participating in “FinnTwin 16,” a nationwide longitudinal cohort study of health behaviors in twins and their families (19) that identified virtually all live twin births from 1975 through 1979 from the central population registry of Finland. The twins and their parents were sent baseline self-report questionnaires when the twins were 16 years old (wave 1), and follow-up questionnaires were mailed to the twins at age 17, age 18, and between ages 22 and 28 (waves 2, 3, and 4, respectively). Data collection and analysis were approved by the ethics committee of the Department of Public Health of the University of Helsinki.
Questionnaire Screening for Eating Disorders
The wave 4 questionnaire included a self-report screen for eating disorder symptoms that assessed current height and weight, ideal weight, minimum and maximum weight at current height, purging, and weight loss behaviors. Body image was assessed by use of three subscales of the Eating Disorder Inventory (20) —body dissatisfaction, drive for thinness, and bulimia. All screen-positive women (N=292), their screen-negative female co-twins (N=134), and 210 randomly selected screen-negative women were invited to participate in diagnostic telephone interviews. A total of 2,881 participants responded to the wave 4 questionnaire (response rate, 90.4%), and the mean age of respondents was 24.4 years (SD=0.9). Details of the screening process are provided elsewhere (21) .
Diagnostic Interviews
Five experienced clinicians (four M.D.’s and one R.N. at the Eating Disorder Unit of Helsinki University Central Hospital) received detailed training in administering the short version of the Structured Clinical Interview for DSM-IV (SCID) (22) . The interviews were conducted by telephone to obtain current and lifetime diagnoses of anorexia nervosa, bulimia nervosa, and binge eating disorder, to define the age of participants at the first and last manifestations of these illnesses, and to establish the temporal sequence of these diagnoses and their respective time courses. Interrater agreement for diagnosis was good (mean kappa=0.87, range=0.64–1.00) (21) . Drs. Keski-Rahkonen and Sihvola supervised interviewers throughout the study and helped solve diagnostic problems, such as concerns about diagnostic threshold and differential diagnosis.
The interview participation rate was 85.2% overall (90.1% for screen-positive women, 76.2% for screen-negative female co-twins, and 84.8% for the random sample of screen-negative women). Only 12 individuals (1.9%) declined to be interviewed; the others who did not participate could not be reached because their current telephone numbers could not be obtained.
Definition of Disorder
Because the diagnostic criteria and the boundaries of anorexia nervosa have changed over time and remain contentious, we used two definitions of the disorder: DSM-IV anorexia nervosa and broad anorexia nervosa. Broad anorexia nervosa includes DSM-IV anorexia nervosa and ICD-10 atypical anorexia, here defined as anorexia nervosa without amenorrhea or weight loss of at least 15% that led to a body mass index (BMI) ≤19, coupled with undue influence of body weight on self-evaluation or intense fear of weight gain.
Many of the cases identified in this study were in subjects who reported that they had never received an eating disorder diagnosis from a health professional. We refer to these cases as undetected by the health care system, and we refer to all other cases as detected by the health care system, whether or not the individuals received treatment for their disorder.
Prevalent and Incident Cases
We defined lifetime prevalent cases of DSM-IV or broad anorexia nervosa to include all cases identified in this study, regardless of age at onset, age at interview, or recovery status. Lifetime prevalent cases of DSM-IV anorexia nervosa comprised 55 probands in 53 twin pairs (51 discordant and two concordant pairs; both concordant pairs were monozygotic); broad anorexia nervosa comprised 107 probands in 100 twin pairs (93 discordant and seven concordant pairs, of which six were monozygotic and one dizygotic).
We defined incident cases for the age interval from 15 to 19 years as those in which the first manifestation of anorexia nervosa occurred during that age interval as reported in the diagnostic interview. For 10 individuals who could not clearly recall their age at illness onset, age at minimum BMI was substituted.
Five-Year Clinical Recovery Rates
For each case of DSM-IV or broad anorexia nervosa, the interviewers determined the last age at which any eating disorder symptoms occurred. We defined clinical recovery as restoration of weight and menstruation and the absence of bingeing and purging for at least 1 year prior to assessment. The 5-year clinical recovery rate was defined as the proportion of women with anorexia nervosa who reached clinical recovery within 5 years after onset.
Outcomes After Clinical Recovery
The possible residua of illness after clinical recovery were measured in three domains. First, physical characteristics were measured by BMI. We calculated current BMI from self-reported weight and height; agreement between self-reported and measured BMI in the women from this birth cohort was 0.92 (23) . Second, social characteristics were measured by occupation, education, parity, and marriage or cohabitation. Third, psychological characteristics were measured by eight scales with well-established psychometric properties: four scales of the Eating Disorder Inventory (drive for thinness, bulimia, body dissatisfaction, and perfectionism) (20) ; the state anxiety and trait anxiety subscales from the Spielberger State-Trait Anxiety Inventory (24) ; the Rosenberg Self-Esteem Scale (25) ; and the Psychosomatic Symptom Scale (26) .
In the evaluation of outcomes after clinical recovery, we compared probands with DSM-IV and broad anorexia nervosa with their unaffected female co-twins. “Unaffected” was defined as screening negative for eating disorder symptoms in the wave 4 questionnaire (21) and not having a lifetime diagnosis of DSM-IV anorexia nervosa, bulimia nervosa, binge eating disorder, or eating disorder not otherwise specified in the SCID interview. Of the 93 co-twins in pairs discordant for broad anorexia nervosa, seven women had lifetime eating disorders, 13 were female co-twins who did not participate in the interview, and 26 were male co-twins from opposite-sex dizygotic twin pairs. After these individuals were excluded, 47 unaffected female co-twins remained.
Although unaffected co-twins are in many respects an ideal comparison group, they may differ from women in the general population. In order to detect any such differences that might be relevant to our conclusions, we drew a random sample of 105 female-female twin pairs (210 women) from the screen-negative women in these birth cohorts. Those who were also negative for all eating disorders in the SCID interview were termed “healthy women” (N=134).
Statistical Analysis
Lifetime prevalences of DSM-IV and of broad anorexia nervosa were calculated by dividing the number of lifetime prevalent cases by the total number of women who responded to the eating disorder screen material in the wave 4 questionnaire (N=2,545).
We computed the incidence rates of DSM-IV and of broad anorexia nervosa for the peak 5-year interval of risk (ages 15–19 years), as has been done in previous studies (5) . For later age groups, the data would be less reliable because of the small number of cases and varying ages at assessment. The numerator was the number of incident cases detected in the given age interval, and the denominator was the number of person-years at risk.
We used the Kaplan-Meier survival method to compute 5-year clinical recovery rates for DSM-IV and broad anorexia nervosa, and we used the log-rank test to compare survival curves across groups.
Psychological outcomes after clinical recovery were analyzed in two ways. To examine trends toward full recovery, we calculated mean psychological outcome scores for women with DSM-IV anorexia nervosa who were currently ill, those who had been in clinical recovery for >5 years, and the two comparison groups (unaffected co-twins and healthy women). These results do not account for age at illness onset and illness duration. Next, to examine the trends toward full recovery after clinical recovery and to assess their statistical significance while also accounting for age at illness onset and illness duration, we designed a model that compared the probands and their unaffected co-twins as a function of time on the eight psychological outcome scales. We predicted each outcome variable using a random intercept linear regression model and the following predictors: disorder status (we used only broad anorexia nervosa because of power constraints), age at illness onset, illness duration, time from recovery to interview for the proband (with linear and quadratic terms), and the same time variables for the co-twin. The random intercepts were included to account for dependence between twins. Age at onset, illness duration, and the time-dependent predictors for the unaffected co-twins were found not to be significant and were dropped from the final model.
For comparisons of physical and social characteristics between cases and comparison groups, we used analysis of variance for continuous outcome measures and logistic regression for categorical outcome measures. To account for clustered sampling within the twin pair, p values and confidence intervals in all analyses were adjusted using standard procedures for survey data (27) . We used the statistical software Stata 9.2 (Stata Corp, College Station, Tex.) for all analyses.
Results
Prevalence and Incidence
The lifetime prevalence was 2.2% (95% confidence interval [CI]=1.6–2.7) for DSM-IV anorexia nervosa (55 cases out of 2,545 women) and 4.2% (95% CI=3.4–5.0) for broad anorexia nervosa (107 cases out of 2,545 women). The incidence of DSM-IV anorexia nervosa for ages 15–19 years was 270 per 100,000 person-years (95% CI=180–360), and the incidence of broad anorexia nervosa was 490 per 100,000 person-years (95% CI=370–610).
Five-Year Clinical Recovery Rate
The 5-year clinical recovery rates were 66.8% and 69.1% for DSM-IV and broad anorexia nervosa, respectively ( Figure 1 ). Overall, 70.9% women with DSM-IV anorexia nervosa and 76.6% with broad anorexia nervosa had reached clinical recovery by the time of the interview.

a Results of Kaplan-Meier survival analysis. The 5-year clinical recovery rate was defined as the proportion who reached clinical recovery within 5 years after onset of illness. Clinical recovery was defined as restoration of weight and menstruation and the absence of bingeing and purging for at least 1 year prior to assessment.
Outcomes After Clinical Recovery
The mean current BMI of DSM-IV anorexia probands in clinical recovery (mean BMI=21.7, SD=3.0, 95% CI=21.0–22.4) did not significantly differ from that of their unaffected co-twins (mean BMI=21.8, SD=2.7, 95% CI=21.0–22.6).
Over time in clinical recovery, the mean psychological outcome scores of DSM-IV anorexia nervosa probands generally improved ( Table 1 ). Using the broad definition of anorexia nervosa to maximize statistical power, we formally tested these observed trends. The null hypothesis was that outcomes of probands and co-twins do not converge, that is, that probands remain more symptomatic than their co-twins. We could reject the null hypothesis for six of the eight outcome measures: drive for thinness (z=–2.30, p=0.021), bulimia (z=–3.23, p<0.001), perfectionism (z=–3.01, p=0.003), state anxiety (z=–2.49, p=0.013), trait anxiety (z=–2.53, p=0.011), and self-esteem (z=4.02, p<0.0001). For the other two measures, there was no detectable convergence of proband and co-twin outcomes (body dissatisfaction, z=–1.35, p=0.18; psychosomatic symptoms, z=–1.42, p=0.16). In other words, we found that the residua of illness receded steadily and statistically significantly over time for six of the eight psychological outcome measures, converging over time with their healthy co-twins’ outcomes ( Figure 2 ).
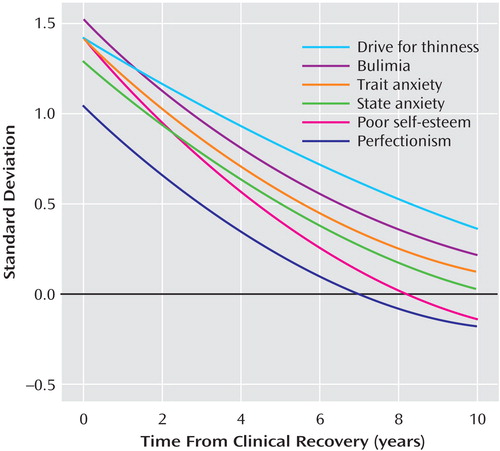
a State and trait anxiety are from the State-Trait Anxiety Inventory, poor self-esteem is from the Rosenberg Self-Esteem Scale, and the other three measures are subscales of the Eating Disorder Inventory. These outcome measures were standardized: for each one, the curved lines represent broad anorexia nervosa probands, and the line at SD=0 represents the level of unaffected co-twins. Age at illness onset and illness duration were not statistically significantly associated with psychological outcomes after clinical recovery.
Neither the women who were currently ill with broad anorexia nervosa nor the probands who were in clinical recovery differed from their unaffected co-twins on education, occupation, or parity. The currently ill probands did differ from their unaffected co-twins in the proportion married or cohabiting with a partner (26.9% versus 53.1%, p=0.04); the probands in clinical recovery showed a smaller and statistically nonsignificant difference from their unaffected co-twins on this measure (43.9% versus 52.1%).
Detected Versus Undetected Cases
Approximately half of the cases ascertained in this study had been detected in the health care system. Detected cases constituted 53% (29 of 55) of all DSM-IV anorexia nervosa cases and 41% (44 of 107) of all broad anorexia nervosa cases. The 5-year clinical recovery rates were similar for the detected and undetected cases: 61.8% versus 68.4%, respectively, for DSM-IV anorexia nervosa, and 60.1% versus 69.5%, for broad anorexia nervosa.
For broad anorexia nervosa, we had a sufficient number of cases to compare the detected and undetected cases on numerous measures, including age at onset, minimum BMI, and psychological symptoms ( Table 2 ). There were few differences between the detected and undetected cases, none statistically significant.
Unaffected Co-Twins Versus Healthy Women
The unaffected co-twins of broad anorexia nervosa probands were also compared with the healthy women from the same birth cohorts ( Table 2 ), and the differences were neither statistically nor clinically significant. The frequency of marriage or cohabitation was similar in unaffected co-twins (52.1%) and healthy women (50.0%).
Discussion
In this population cohort of young women, there were three main findings. First, the incidence rate of anorexia nervosa was about twice as high as rates reported in prior studies. Second, the great majority of women who developed anorexia nervosa achieved clinical recovery within 5 years. Third, 5 years after clinical recovery, most women reached complete or nearly complete psychological recovery, closely resembling their unaffected co-twins and healthy women in weight and psychosocial measures.
Incidence Rates
The incidence rate of DSM-IV anorexia nervosa at ages 15–19 years was 270 per 100,000 person-years in this study, compared with previous reports of 136 per 100,000 person-years in the United States (4) and 109 per 100,000 person-years in the Netherlands (11) . We propose five competing explanations for the high incidence rate: first, that anorexia nervosa was underascertained in prior studies, most of which were restricted to cases detected in the health care system; second, that anorexia nervosa was overascertained in this study; third, that anorexia nervosa is more common among twin than nontwin individuals because of unknown twin-specific exposures not shared by the general population; fourth, that the incidence rate of anorexia nervosa in Finland may be higher than in other countries; and fifth, that high incidence rates of anorexia nervosa were observed because of a cohort effect.
The first explanation predicts that our results should be similar to those of prior studies when we compute our incidence rates only on the basis of cases detected in the health care system. This prediction was borne out: the incidence of DSM-IV anorexia nervosa, based only on the detected cases, was 140 per 100,000 person-years at ages 15–19 years, which is similar to the figures cited above from the United States and the Netherlands. Also, our lifetime prevalences are well in line with earlier community-based observations from the United States (28) and Australia (29) .
The second explanation predicts that noncases misclassified as cases of anorexia nervosa (undetected cases) should have a less severe and clear-cut illness than true (detected) cases. This prediction was not borne out: the undetected and the detected cases exhibited similar psychopathology and recovery rates.
The third explanation predicts that anorexia is more common among twin than nontwin individuals. However, previous research has found that rates of psychiatric disorders in twin and nontwin populations are comparable (30) . In this study, we found no differences in the diagnostic distribution and outcomes of broad anorexia nervosa by zygosity, and most cases were from discordant twin pairs. We also observed no appreciable differences in marriage and cohabitation frequency, body dissatisfaction, or psychosomatic symptoms between monozygotic and dizygotic healthy women (data available from first author).
Our data thus suggest that the incidence of anorexia nervosa has been substantially underestimated in previous studies, because a large proportion of true cases of anorexia nervosa remain undetected (5 , 18) , even in countries with highly developed and universal health care systems, such as Finland. More research on the patterns of help-seeking behavior in women with anorexia nervosa is warranted.
The other two possible explanations cannot be directly tested by our study. The first is that the incidence rate of anorexia nervosa in Finland may be higher than in other countries. However, several recent studies have found lifetime prevalences of anorexia nervosa comparable to ours, although they did not assess incidences of anorexia nervosa (4 , 28 , 29) . The second is that the high incidences of anorexia nervosa we detected may in part reflect a secular trend that is specific to recent birth cohorts. Bulik et al. (4) recently demonstrated that the prevalence of anorexia nervosa is greater among Swedes born after 1945 than among those born earlier. The incidence of anorexia nervosa also has risen linearly in the United States and in the Netherlands in recent past decades (9 – 11) .
Clinical Recovery Rates
The 5-year clinical recovery rate of anorexia nervosa in our study was higher than rates reported by most, though not all, previous studies. A recent review of 119 clinical outcome studies found that 47% of participants with anorexia nervosa reached clinical recovery (14) . Recovery rates increased significantly with follow-up time. In studies that recorded 5- or 6-year recovery rates from anorexia nervosa, the proportion achieving clinical recovery ranged from 35% to 80% of participants; the use of different definitions of clinical recovery probably contributed to the variability of the recovery rates (31 – 36) . In this study, more than two-thirds of the women with DSM-IV anorexia nervosa achieved clinical recovery within 5 years. Despite this, the burden of illness was considerable: in almost two-thirds of the cases, the illness duration was ≥2 years, and in half, it was ≥3 years.
Outcomes After Recovery
Rather than simply relying on our evaluation of clinical recovery, we were able to compare broad anorexia probands with their unaffected co-twins and healthy women on multiple measures. Probands with broad anorexia nervosa in clinical recovery could not be distinguished from their unaffected co-twins and healthy women in self-reported BMI, nor on measures of social function. They still differed from their unaffected co-twins on eight measures designed to capture psychological characteristics. Over time, however, these residua of illness receded. On six of the eight measures, the probands progressed to full recovery. The pattern was less clear for the other two measures of psychological characteristics: body dissatisfaction and psychosomatic symptoms appeared to be more persistent in the probands. Future follow-up waves will establish whether these differences diminish over time.
Limitations
Selection bias due to differential participation of cases and noncases of anorexia nervosa in the telephone interviews is possible but likely minimal. Telephone numbers were obtained by letters sent to addresses updated from the Finnish population registry (response rate, 90.4%). The telephone interview participation rate of women with self-reported eating disorders was 90.1%, while that of healthy women was 84.8%.
The impact of treatment on outcome could not be directly assessed in this study. We found that the detection of broad anorexia nervosa by the health care system had no association with prognosis in this study. This result does not, however, demonstrate that treatment had no effect, because case detection does not necessarily imply treatment (or proper treatment).
We did not assess mortality, because the number of cases was small and the follow-up did not extend beyond ages 22–28 years. Previous studies have shown that the risk of mortality increases as a function of illness duration (16) . Only a third of women with broad anorexia nervosa (N=38) in our study had eating disorder symptoms for more than 5 years, and only 8.4% (N=19) had them for more than 10 years. Thus, estimates of anorexia nervosa-related mortality in this birth cohort will be more meaningful when linkage with mortality and cause-of-death registries is conducted. It is worth noting, nonetheless, that the overall mortality in this cohort was very low; only eight deaths were recorded in the population registry between the first assessment wave at age 16 and the fourth wave at ages 22–28. In the worst-case scenario, if all the deaths in the cohort were due to anorexia nervosa, the crude mortality rate of 0.3% per decade would be markedly lower than those recorded in follow-up studies of anorexia nervosa in clinical settings (37 , 15 – 17) , although they would be in line with community-based and national registry-based observations (38 – 40) .
Conclusion
In this population study, the incidences of DSM-IV and broad anorexia nervosa were much higher than rates reported previously. The 5-year clinical recovery rates were higher than those reported in most previous studies. Nonetheless, the burden of illness was remarkable. After clinical recovery, the residua of illness steadily receded: women closely resembled their unaffected co-twins on most measures after 5 years in clinical recovery, which demonstrates that full psychological recovery is both possible and likely.
1. Becker AE, Grinspoon SK, Klibanski A, Herzog DB: Eating disorders. N Engl J Med 1999; 340:1092–1098Google Scholar
2. Fairburn CG, Harrison PJ: Eating disorders. Lancet 2003; 361:407–416Google Scholar
3. Walsh BT, Devlin MJ: Eating disorders: progress and problems. Science 1998; 280:1387–1390Google Scholar
4. Bulik CM, Sullivan PF, Tozzi F, Furberg H, Lichtenstein P, Pedersen NL: Prevalence, heritability, and prospective risk factors for anorexia nervosa. Arch Gen Psychiatry 2006; 63:305–312Google Scholar
5. Hoek HW, van Hoeken D: Review of the prevalence and incidence of eating disorders. Int J Eat Disord 2003; 34:383–396Google Scholar
6. Susser E, Schwartz S, Morabia A, Bromet E: Psychiatric Epidemiology. New York, Oxford University Press, 2006Google Scholar
7. Currin L, Schmidt U, Treasure J, Jick H: Time trends in eating disorder incidence. Br J Psychiatry 2005; 186:132–135Google Scholar
8. Hoek HW, Bartelds AIM, Bosveld JJF, van der Graaf Y, Limpens VEL, Maiwald M, Spaaij CJK: Impact of urbanization on detection rates of eating disorders. Am J Psychiatry 1995; 152:1272–1278Google Scholar
9. Lucas AR, Beard CM, O’Fallon WM, Kurland LT: 50-year trends in the incidence of anorexia nervosa in Rochester, Minn: a population-based study. Am J Psychiatry 1991; 148:917–922Google Scholar
10. Lucas AR, Crowson CS, O’Fallon WM, Melton LJ III: The ups and downs of anorexia nervosa. Int J Eat Disord 1999; 26:397–405Google Scholar
11. Van Son GE, van Hoeken D, Bartelds AI, Van Furth EF, Hoek HW: Time trends in the incidence of eating disorders: a primary care study in the Netherlands. Int J Eat Disord 2006; 39:565–569Google Scholar
12. Lewinsohn PM, Striegel-Moore RH, Seeley JR: Epidemiology and natural course of eating disorders in young women from adolescence to young adulthood. J Am Acad Child Adolesc Psychiatry 2000; 39:1284–1292Google Scholar
13. Rastam M, Gillberg C, Wentz E: Outcome of teenage-onset anorexia nervosa in a Swedish community-based sample. Eur Child Adolesc Psychiatry 2003; 12(suppl 1):I78–I90Google Scholar
14. Steinhausen H-C: The outcome of anorexia nervosa in the 20th century. Am J Psychiatry 2002; 159:1284–1293Google Scholar
15. Harris EC, Barraclough B: Excess mortality of mental disorder. Br J Psychiatry 1998; 173:11–53Google Scholar
16. Sullivan PF: Mortality in anorexia nervosa. Am J Psychiatry 1995; 152:1073–1074Google Scholar
17. Theander S: Outcome and prognosis in anorexia nervosa and bulimia: some results of previous investigations, compared with those of a Swedish long-term study. J Psychiatr Res 1985; 19:493–508Google Scholar
18. Hudson JI, Hiripi E, Pope HG Jr, Kessler RC: The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry 2007; 61:348–358Google Scholar
19. Kaprio J, Pulkkinen L, Rose RJ: Genetic and environmental factors in health-related behaviors: studies on Finnish twins and twin families. Twin Res 2002; 5:366–371Google Scholar
20. Garner DM: Eating Disorder Inventory 2, Professional Manual. Odessa, Fla, Psychological Assessment Resources, 1991Google Scholar
21. Keski-Rahkonen A, Sihvola E, Raevuori AH, Kaukoranta J, Bulik CM, Hoek HW, Rissanen A, Kaprio J: Reliability of self-reported eating disorders: optimizing population screening. Int J Eat Disord 2005; 39:754–762Google Scholar
22. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-Patient Edition (SCID-I/NP). New York, Biometrics Research, New York State Psychiatric Institute, November 2002Google Scholar
23. Schousboe K, Willemsen G, Kyvik KO, Mortensen J, Boomsma DI, Cornes BK, Davis CJ, Fagnani C, Hjelmborg J, Kaprio J, De Lange M, Luciano M, Martin NG, Pedersen N, Pietilainen KH, Rissanen A, Saarni S, Sorensen TI, Van Baal GC, Harris JR: Sex differences in heritability of BMI: a comparative study of results from twin studies in eight countries. Twin Res 2003; 6:409–421Google Scholar
24. Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA: Manual for the State-Trait Anxiety Inventory. Palo Alto, Calif, Consulting Psychologists Press, 1983Google Scholar
25. Rosenberg M: Society and the Adolescent Self-Image, rev ed. Middletown, Conn, Wesleyan University Press, 1989Google Scholar
26. Aro H: Life stress and psychosomatic symptoms among 14 to 16-year old Finnish adolescents. Psychol Med 1987; 17:191–201Google Scholar
27. Williams RL: A note on robust variance estimation for cluster-correlated data. Biometrics 2000; 56:645–646Google Scholar
28. Klump KL, Miller KB, Keel PK, McGue M, Iacono WG: Genetic and environmental influences on anorexia nervosa syndromes in a population-based twin sample. Psychol Med 2001; 31:737–740Google Scholar
29. Wade TD, Bergin JL, Tiggemann M, Bulik CM, Fairburn CG: Prevalence and long-term course of lifetime eating disorders in an adult Australian twin cohort. Aust NZ J Psychiatry 2006; 40:121–128Google Scholar
30. Ben Tovim DI, Walker K, Gilchrist P, Freeman R, Kalucy R, Esterman A: Outcome in patients with eating disorders: a 5-year study. Lancet 2001; 357:1254–1257Google Scholar
31. Kendler KS: Twin studies of psychiatric illness: an update. Arch Gen Psychiatry 2001; 58:1005–1014Google Scholar
32. Fichter MM, Quadflieg N: Six-year course and outcome of anorexia nervosa. Int J Eat Disord 1999; 26:359–385Google Scholar
33. Gillberg IC, Rastam M, Gillberg C: Anorexia nervosa outcome: six-year controlled longitudinal study of 51 cases including a population cohort. J Am Acad Child Adolesc Psychiatry 1994; 33:729–739Google Scholar
34. Martin FE: The treatment and outcome of anorexia nervosa in adolescents: a prospective study and five year follow-up. J Psychiatr Res 1985; 19:509–514Google Scholar
35. Norring CE, Sohlberg SS: Outcome, recovery, relapse, and mortality across six years in patients with clinical eating disorders. Acta Psychiatr Scand 1993; 87:437–444Google Scholar
36. Steinhausen HC, Seidel R, Winkler MC: Evaluation of treatment and intermediate and long-term outcome of adolescent eating disorders. Psychol Med 2000; 30:1089–1098Google Scholar
37. Birmingham CL, Su J, Hlynsky JA, Goldner EM, Gao M: The mortality rate from anorexia nervosa. Int J Eat Disord 2005; 38:143–146Google Scholar
38. Korndörfer SR, Lucas AR, Suman VJ, Crowson CS, Krahn LE, Melton LJ III: Long-term survival of patients with anorexia nervosa: a population-based study in Rochester, Minn. Mayo Clin Proc 2003; 78:278–284Google Scholar
39. Lindblad F, Lindberg L, Hjern A: Improved survival in adolescent patients with anorexia nervosa: a comparison of two Swedish national cohorts of female inpatients. Am J Psychiatry 2006; 163:1433–1435Google Scholar
40. Reas DL, Kjelsas E, Heggestad T, Eriksen L, Nielsen S, Gjertsen F, Gotestam KG: Characteristics of anorexia nervosa-related deaths in Norway (1992–2000): data from the National Patient Register and the Causes of Death Register. Int J Eat Disord 2005; 37:181–187Google Scholar





