Risk Factors for Suicide Completion in Major Depression: A Case-Control Study of Impulsive and Aggressive Behaviors in Men
Abstract
OBJECTIVE: Major depression is a major risk factor for suicide. However, not all individuals with major depression commit suicide. Impulsive and aggressive behaviors have been proposed as risk factors for suicide, but it remains unclear whether their effect on the risk of suicide is at least partly explained by axis I disorders commonly associated with suicide, such as major depression. With a case-control design, a comparison of the level of impulsive and aggressive behaviors and the prevalence of associated psychopathology was carried out with control for the presence of primary psychopathology. METHOD: One hundred and four male suicide completers who died during an episode of major depression and 74 living depressed male comparison subjects were investigated with proxy-based interviews by using structured diagnostic instruments and personality trait assessments. RESULTS: The authors found that current (6-month prevalence) alcohol abuse/dependence, current drug abuse/dependence, and cluster B personality disorders increased the risk of suicide in individuals with major depression. Also, higher levels of impulsivity and aggression were associated with suicide. An analysis by age showed that these risk factors were more specific to younger suicide victims (ages 18–40). A multivariate analysis indicated that current alcohol abuse/dependence and cluster B personality disorder were two independent predictors of suicide. CONCLUSIONS: Impulsive-aggressive personality disorders and alcohol abuse/dependence were two independent predictors of suicide in major depression, and impulsive and aggressive behaviors seem to underlie these risk factors. A developmental hypothesis of suicidal behavior, with impulsive and aggressive behaviors as the starting point, is discussed.
Several lines of evidence confirm the strong association between major depressive disorder and completed suicide (1–4). More specifically, estimates indicate that approximately 60% of suicide victims suffered from major depressive disorder and other mood disorders (3, 5–7). On the other hand, most subjects affected with major depressive disorder do not die by suicide. The lifetime mortality risk by suicide of subjects with major depressive disorder who have been inpatients has usually been reported at around 15% (8). This was revised to 3.4%, with a higher risk in men (7%) than in women (1%) (9). Regardless of the exact suicide mortality risk faced by subjects affected with major depressive disorder, it is clear that this figure is substantial. Why some patients with major depressive disorder die by suicide while others with seemingly the same disorder do not, is a question of enormous clinical relevance.
Among sociodemographic risk factors, gender, marital status, and migration are those more strongly associated with suicide in patients with major depressive disorder (10, 11). Issues related to social and/or medical support, such as discharge from psychiatric care (12) and certain clinical symptoms, have also been identified as predictors of suicide. In addition, a positive history of suicide attempts seems to be a powerful predictor identified by some studies (13–15). Furthermore, investigators have reported that various clinical symptoms of depression, such as insomnia, memory problems, self-neglect, anhedonia, hopelessness, and comorbidity with alcohol dependence/abuse, increase the risk of suicide (11, 16–19).
There has been growing evidence to support the role of impulsive and aggressive behaviors in the risk of suicide. Studies assessing living patients with major depressive disorder have indicated that suicide attempters have higher levels of impulsive and aggressive behaviors (20–24). Similarly, studies looking at the prevalence of these traits in other diagnostic categories have also suggested that attempters are more likely to be impulsive and aggressive (25–29). However, data on impulsive and aggressive behaviors in suicide completers are limited and based primarily on indirect evidence, such as the prevalence of diagnostic categories associated with aggressive and impulsive traits. These studies showed that substance use disorders (1) and borderline personality disorders (30) are associated with an increased risk of suicide when they are comorbid with major depressive disorder. The few studies that carried out direct personality trait assessments remain controversial. Two studies found an association between aggression and suicide (31, 32), but one recent study in adults ages 50 and over showed that the association between aggression and suicide was no longer significant when the authors controlled for psychopathology (33). Therefore, it remains unclear whether the association between impulsive and aggressive behaviors and the risk of suicide is at least partly explained by axis I disorders that are commonly associated with suicide, such as major depressive disorder. This issue has not been properly addressed because almost all previous studies of suicide have exclusively investigated unselected suicide victims in relation to normal comparison subjects and lacked a psychiatric comparison group. Thus, the purpose of our study was to investigate impulsive and aggressive behaviors and associated psychopathology while we directly controlled for major depressive disorder. More specifically, we investigated subjects who committed suicide in the context of a major depressive episode and compared them to a group of age- and gender-matched living subjects with a current major depressive episode of sufficient severity to warrant treatment in a specialized psychiatric outpatient clinic but without a history of medically serious suicide attempts. A key methodological innovation in this study was the use of a proxy informant for both the suicide group, when it was necessary, and also for the living depressed comparison subjects to prevent a reporting artifact because of the method of data collection.
Method
Subjects
Patients used for this study were 104 men ages 18 years and over who committed suicide, as determined by the Quebec Coroner’s Office, and who met DSM-IV diagnostic criteria for major depressive disorder or depression not otherwise specified in the 6 months before their death. Individuals with depression not otherwise specified (operationally defined as depressed mood or lack of interest most of the time for at least 2 weeks and four symptoms of depression) were selected for this study because these patients most likely had major depressive disorder. They were not recognized as having such because of the reduced sensitivity of the psychological autopsy procedure, particularly for conditions present immediately before death (34). The subjects who met criteria for bipolar or any psychotic disorder were excluded to increase comparability between groups. Our subjects were consecutive male suicide victims (representative of male suicide cases in the general population) who were recruited primarily from 2000 to 2004. The acceptance rate of participation by the families of the suicide victims was 75%. Suicide cases from families who did not agree to participate were not different from those included in the study with regard to age, race, or method of suicide.
The comparison subjects were 74 living men, age-matched (within 2 years) to the cases, who met criteria for major depressive disorder with a condition severe enough to require follow-up in a specialized psychiatric outpatient clinic. The acceptance rate of participation was 90%, and those who did not agree to participate had similar demographic characteristics to those who accepted. To ensure comparability of the two groups, all comparison subjects were diagnosed by proxy-based interviews carried out on average 5 months after recruitment. This project was approved by our local institutional review board and the families of the suicide victims; comparison subjects and informants signed written informed consents.
Diagnoses
Psychiatric diagnoses in suicide victims were made by means of the psychological autopsy method. This technique, which has been validated for axis I and II diagnoses (32, 35, 36), consists in part of selecting a family member who was best acquainted with the deceased to serve as an informant for the interview process. In our study, the informants included a mother, father, sibling, significant other, friend, or other relative. We have previously shown that the type of informant makes no significant difference in the rate of specific disorders identified (3). The families were recruited at the Montreal Morgue and were interviewed, on average, 4 months after the suicide.
Psychiatric diagnoses were obtained by using the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) (37), in addition to the Structured Clinical Interview for DSM-IV Personality Disorders (SCID-II) (38). The SCID was used to investigate 71 suicide victims and all comparison subjects. Before the SCID, we used the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS) (39), an interview modified to include questions adapted from the Interview Schedule for Children (40), to assess personality disorders. As reported elsewhere (7), the diagnoses obtained using these two different methods had excellent concordance rates. Information collected through the SCID or the K-SADS interviews and from the coroner’s notes and medical records was used by the interviewers to write a case history for each subject. These case histories were reviewed by a clinical panel to reach a consensus regarding DSM-IV diagnoses for each subject.
Interrater Reliability
Two or more interviewers were asked to separately rate the same subject, and kappa coefficients for key diagnoses were excellent: major depression, 0.96; alcohol abuse/dependence, 0.98; drug abuse/dependence, 1.00; bipolar disorder, 1.00; schizophrenia, 1.00, and cluster B personality disorders, 1.00. These excellent concordance rates are consistent with previous analyses by our group (3) and are probably a consequence of substantial clinical training of the interviewers, who were all clinical psychologists, and of regular training sessions carried out by our clinical coordinator to avoid drifting.
Personality Trait Assessments
The Brown-Goodwin History of Aggression (41) is an 11-item interview that assesses lifetime aggressive behaviors across three separate stages of life (childhood, adolescence, and adulthood). The Barratt Impulsiveness Scale (42) has been commonly used in the investigation of impulsive behaviors and consists of 30 items. Finally, the Temperament and Character Inventory (43) was used to collect data by assessing four basic temperament and three character dimensions. The estimate for internal consistency was excellent overall with the informant version of the Brown-Goodwin History of Aggression (alpha=0.88), the Barratt Impulsiveness Scale (alpha=0.89), and the Temperament and Character Inventory (alphas between 0.73 and 0.88 for the four temperament and three character scales).
Validity of Proxy-Based Personality Assessments
We compared personality trait assessments by means of the instruments listed and scored them using two different informants for each subject. No significant differences were found for any of the comparisons (p values between 0.25 and 0.94), which had good measures of symmetry (gamma values between 0.40 and 0.68). Furthermore, with living subjects, we compared information obtained with the same instruments with an informant and the subject and found no significant differences (p values between 0.67 and 0.98 for all comparisons) and also good measures of symmetry (gamma values between 0.46 and 0.75). These findings are consistent with the literature on the validity of behavioral assessments with informants (32, 35, 36).
In addition, the validity of impulsive and aggressive measures was supported by the finding of a positive correlation between disorders that are characterized by high levels of these behaviors. A positive correlation was found between levels of impulsivity (Barratt Impulsiveness Scale) and aggression (Brown-Goodwin History of Aggression) (r=0.36, p<0.001). Moreover, high levels of impulsivity and high levels of lifetime aggression were correlated with severity of alcohol and drug abuse/dependence, as well as with cluster B personality disorders (r values between 0.17 and 0.58 for all tested correlations). These findings are consistent with previous reports (31, 44).
Classification of Suicide
Suicide cases were classified as violent and nonviolent, according to the classification system used in other studies (45–47). Poisoning, gas, and drowning were classified as nonviolent, whereas all other suicide methods were classified as violent.
Statistical Analysis
Statistical analyses were performed with SPSS version 11.5 (SPSS, Chicago) and Epi-Info version 6 (Centers for Disease Control, Atlanta). Chi-square analyses, Fisher’s exact test (two-tailed), and odds ratios (with the exact limit test to evaluate the 95% confidence interval [CI]) were used to compare categorical variables, and Student’s t test was used to analyze continuous variables. The joint effect of the independent variables, including age and the interactions of age and independent variables, were then analyzed with stepwise logistic regression.
Results
Study Group Characteristics
One hundred four depressed male suicide completers and 74 living depressed men were included in this study. Their ages (suicide victims: mean=40.6, SD=14.4; comparison subjects: mean=43.0, SD=10.8), working status (employed—suicide victims: N=52, 60%; comparison subjects: N=26, 61%), and education levels (completed college—suicide victims: N=17, 20%; comparison subjects: N=15, 24%) were similar between the groups. In addition, a similar proportion of suicide victims and comparison subjects had at least one or more children (suicide victims: N=53, 59%; comparison subjects: N=36, 62%). Almost all suicide cases and comparison subjects were from the same ethnic and cultural/religious backgrounds (N=57 and 66, 98%, in both groups were French Canadian, and N=55 and 63, 95%, in both groups were Catholic). There were no significant differences between groups in family history of suicide or in history of physical and/or sexual abuse.
Axis I Disorders
The prevalence rates of alcohol abuse/dependence and drug abuse/dependence in the last 6 months were significantly higher in depressed suicide completers than in depressed comparison subjects. No significant differences were found in the prevalence rates of other major axis I diagnoses in the last 6 months (Table 1). In addition, although a higher proportion of depressed suicide completers had a positive lifetime history of substance-related disorders, no significant differences were found for any lifetime axis I diagnosis (Table 1). Finally, two or more comorbid axis I disorders were more prevalent in depressed suicide completers (N=38, 37%) than in depressed comparison subjects (N=8, 11%) (odds ratio=4.75, 95% CI=1.97–12.60).
Axis II Disorders
The prevalence rates of cluster B personality disorders were significantly higher in depressed suicide victims than in depressed comparison subjects (Table 1). On the other hand, the prevalence rates of cluster A and cluster C personality disorders were comparable between suicide victims and comparison subjects. Finally, two or more comorbid axis I and axis II disorders were more prevalent in depressed suicide completers (N=54, 50%) than in depressed comparison subjects (N=14, 21%) (odds ratio=3.87, 95% CI=1.85–8.29).
Behavioral Measures
Mean scores on measures of impulsive behaviors obtained by using the total score on the Barratt Impulsiveness Scale were comparable between groups. Nevertheless, the prevalence rates of highly impulsive individuals (those scoring 75 and higher, as suggested by Barratt [48]) were significantly higher in depressed suicide completers than in depressed comparison subjects (p=0.001) (Table 2). In addition, mean scores on lifetime aggressive behavior measures obtained by using the total score on the Brown-Goodwin History of Aggression were significantly higher (p<0.02) in depressed suicide completers than in depressed comparison subjects. However, measures on the Temperament and Character Inventory were not statistically different between groups (Table 2).
Analysis by Age
To explore the possible effect of age, we decided to separate the groups by using 40 years as the cutoff point (18–40 years and ≥41). This point was chosen primarily because it was the mean and median age of our study group and because this is the age up to which suicide is the leading cause of death for men in Canada (49).
The prevalence rates of alcohol abuse/dependence in the last 6 months were significantly higher in younger depressed suicide completers than in younger depressed comparison subjects, and a nonsignificant higher proportion of younger depressed suicide completers had a positive history of drug abuse/dependence during the 6 months before their deaths. No other significant differences were found on current axis I diagnoses between younger and older depressed suicide completers (Table 3).
Lifetime prevalence rates of drug abuse/dependence were significantly higher in younger depressed suicide completers than in younger depressed comparison subjects but not in older depressed suicide completers compared to older depressed comparison subjects. There was a nearly significant difference between alcohol abuse/dependence among depressed suicide completers older than 40 compared to older depressed comparison subjects. No other significant differences were found on lifetime axis I diagnoses in younger or older depressed suicide completers (Table 3).
The prevalence rates of cluster B personality disorders were significantly higher in younger depressed suicide victims than in younger depressed comparison subjects but not in older cases, whereas no significant differences were found between younger and older depressed suicide victims compared to depressed comparison subjects for cluster A and cluster C personality disorders (Table 3). Nevertheless, interesting nearly significant differences were observed, particularly with regard to the effect of cluster C diagnoses in younger depressed suicide victims.
There was a marked effect of age on direct measures of impulsive and aggressive behaviors. In particular, the proportion of highly impulsive individuals, as well as mean scores of lifetime aggressive behaviors, were significantly higher in depressed suicide victims than in depressed comparison subjects only in the younger age group (Table 2).
Finally, we found that suicide completers 40 years and younger were using marginally more violent suicide methods (N=41, 85%) than suicide cases older than 40 (N=27, 66%) (odds ratio=3.04, 95% CI=0.98–10.00).
Predictors of Suicide
A stepwise logistic regression that included all significant variables and their interaction with age showed that cluster B personality disorders and alcohol abuse/dependence in the last 6 months were two independent predictors of suicide in major depressive disorder. The adjusted odds ratio for cluster B personality disorders was 16.59 (95% CI=2.02–136.24), and the adjusted odds ratio for alcohol abuse/dependence for the last 6 months was 4.08 (95% CI=1.38–12.06). No interaction term was a significant predictor of suicide outcome. Figure 1 illustrates the major predictors of suicide and other variables that significantly correlated with these predictors.
Discussion
One hundred four men who committed suicide during an episode of major depressive disorder were compared to a group of 74 living men with major depressive disorder. Both groups were similar in terms of age, marital and parental status, education level, race, and religion. To our knowledge, this is the first study that has used a design that allowed direct control for the effect of major depressive disorder during an investigation of risk factors for suicide. In addition, there are only a few studies of suicide completers (31–33) that investigated impulsive and aggressive behaviors using a case-control design and standardized interviews to retrieve information on personality disorders and personality traits of the deceased.
Axis I Disorders
Alcohol abuse/dependence during the 6 months preceding death increased the likelihood of dying by suicide in patients with major depressive disorder. A logistic regression analysis with control for the effects of age showed that the presence of alcohol abuse/dependence in the last 6 months was a good predictor of suicide, with an adjusted risk of 4.08. On the other hand, the prevalence rates of alcohol abuse/dependence in the last 6 months did not remain significant when we controlled for other significant factors. This finding is probably attributable to the fact that among those with drug abuse/dependence in the month preceding death, many (N=11, 52%) had also concomitant alcohol abuse/dependence. These findings confirm previous studies that showed the importance of substance abuse/dependence as a risk factor for suicide in adolescents and suicide attempters when it was comorbid with major depression (50–57).
Comorbidity with anxiety disorder does not appear to be a major risk factor for suicide in major depressive disorder in men. More specifically, panic disorder, when comorbid with major depressive disorder, has been reported to increase the risk of suicidal behavior (58, 59). However, in our study, depressed suicide completers had rates of panic disorder (N=2, 1.9%) that were comparable to those of depressed comparison subjects (N=2, 2.7%). This is consistent with previous studies of patients with major depression that reported no relationship between comorbidity with panic disorder and increased risk for lifetime suicide attempts (60). Nevertheless, it is possible that we failed to see an effect of anxiety disorders on suicide risk because we focused on male major depressive disorder in this study, and comorbidity with panic disorder has been reported to be more common in female suicide victims than in male suicide victims (61).
Axis II Disorders
Our analysis showed that cluster B personality disorders were major independent predictors of male suicide in major depressive disorder. Primarily, personality disorders characterized by the presence of impulsive/aggressive personality traits (borderline and antisocial) were observed as cluster B personality disorders in our study group, with 43% of them (N=13) having both diagnoses. This finding is consistent with previous studies (3, 30, 31, 62, 63) about antisocial and borderline personality disorders as risk factors for suicidal behavior. In addition, at the time of death, 71% (N=21) of those affected by a cluster B personality disorder had alcohol and/or drug abuse/dependence. This observation supports the vision that higher levels of impulsive and aggressive behaviors combined with behavioral disinhibition facilitated by substance use may mediate suicide in major depressive disorder and is consistent with previous research on suicide completers (64). However, our analysis showed that this seems to be particularly the case for younger suicide completers.
On the other hand, we found that cluster C personality disorders were not associated with an increased risk of suicide when we directly controlled for major depressive disorder. This result contrasts with findings from Foster et al. (65) and Cheng et al. (30) and suggests that cluster C personality disorders may be more directly related to the risk of major depressive disorder than to the risk of suicidal behavior.
Impulsive and Aggressive Behaviors
We found that impulsive and aggressive behaviors were associated with the risk of suicide in depression and that this effect was more important among younger cases (18 to 40 years). On the other hand, impulsive and aggressive behaviors were not direct predictors of suicide. It seems that these personality traits probably underlie the main predictors. This vision is supported by the positive correlation found between impulsive and aggressive behaviors and cluster B personality disorder and alcohol and drug abuse/dependence. It is possible to speculate that a developmental cascade may start with a biological predisposition to higher levels of impulsive and aggressive behaviors. Having a higher level of impulsive and aggressive behavior may, in turn, increase the risk of developing a cluster B personality disorder that, per se, could lead to an increased risk of substance abuse/dependence (66–68). This developmental hypothesis of suicidal behavior is also supported by at least one other study showing that borderline personality disorder alone was not a risk factor for suicide (30), but when it was comorbid with severe depression, the risk of dying by suicide was increased close to 450 times.
Age Effects
The effect of age on the mediating role of impulsive and aggressive behaviors and substance abuse/dependence on the risk of suicide was suggested by the stratified analyses. We have further explored this effect by investigating how these risk factors interacted with age in the regression model; however, the interactions were not retained in the final model. This is explained by the fact that although impulsive and aggressive behaviors and substance abuse/dependence are not significant risk factors in subjects older than 40, their effect is in a similar direction. In other words, these variables do not have opposite effects according to age.
Limitations
The limitations associated with the methods employed in this study are inherent to postmortem studies involving proxy-based interviews. However, the validity of such procedures, particularly with regard to the use of observable behaviors, has been well demonstrated (32), and our comparisons of data obtained using two different informants on the same subject, as well as comparisons between the comparison subject and his or her informant, further support its use on behavioral measures. On the other hand, the major problem of proxy-based interviews seems to be at the level of sensitivity (34). Nevertheless, using proxy-based techniques in both groups, we controlled for this possible bias.
Another important limitation of this study is that we focused on male subjects. How generalizable are the risk factors identified in this study to female depressed patients is an issue that deserves investigation. Of particular interest will be to investigate whether or not impulsive and aggressive behaviors play a similar role in mediating suicide in depressed women as they seem to play in depressed men.
Conclusions
This study was the first to our knowledge to investigate suicide completers in a specific diagnostic category by using a case-control design. Thus, 104 male depressed suicide completers and 74 living depressed male comparison subjects were investigated by means of the psychological autopsy method to better define the risk factors for suicide in major depressive disorder. We found that current alcohol abuse/dependence and the presence of a cluster B personality disorder were two independent risk factors for suicide among depressed individuals. In addition, we found that impulsive and aggressive behaviors were associated with suicide, but this association was not independent of cluster B and alcohol abuse in relation to suicide. These risk factors seem to play a larger role in younger suicide victims (ages 18–40). Further studies should be carried out to investigate the external validity of these findings, particularly among women and in other diagnostic categories associated with suicide, such as schizophrenia.
 |
 |
 |
Received June 4, 2004; revision received Aug. 31, 2004; accepted Dec. 2, 2004. From the McGill Group for Suicide Studies, Douglas Hospital Research Centre, and the Department of Psychiatry, McGill University; the Centre de Recherche Fernand-Seguin, Hôpital L-H. Lafontaine, Université de Montréal, Montreal; and the New York State Psychiatric Institute, Departments of Psychiatry and Neuroscience, Columbia University, New York. Address correspondence and reprint requests to Dr. Turecki, McGill Group for Suicide Studies, Douglas Hospital, McGill University, 6875 LaSalle Blvd., Montreal, Que. H4H 1R3, Canada; [email protected] (e-mail). Supported by the Canadian Institute of Health Research (grant MOP-38078). Dr. Turecki is a Canadian Institute of Health Research scholar.
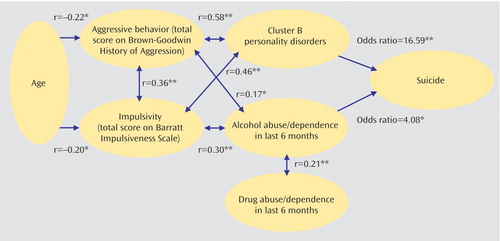
Figure 1. Relationship Between Cluster B Personality Disorders, Alcohol and/or Drug Abuse/Dependence in the Last 6 Months, Age, Impulsivity, and Aggressive Behaviors in Predicting Suicide in Subjects With Major Depression
*p<0.01. **p<0.001.
1. Brent DA: Depression and suicide in children and adolescents. Pediatr Rev 1993; 14:380–388Crossref, Medline, Google Scholar
2. Conwell Y, Duberstein PR, Cox C, Herrmann JH, Forbes NT, Caine ED: Relationships of age and axis I diagnoses in victims of completed suicide: a psychological autopsy study. Am J Psychiatry 1996; 153:1001–1008Link, Google Scholar
3. Lesage AD, Boyer R, Grunberg F, Vanier C, Morissette R, Menard-Buteau C, Loyer M: Suicide and mental disorders: a case-control study of young men. Am J Psychiatry 1994; 151:1063–1068Link, Google Scholar
4. Angst J, Gamma A, Gastpar M, Lepine JP, Mendlewicz J, Tylee A: Gender differences in depression: epidemiological findings from the European DEPRES I and II studies. Eur Arch Psychiatry Clin Neurosci 2002; 252:201–209Crossref, Medline, Google Scholar
5. Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM: Psychological autopsy studies of suicide: a systematic review. Psychol Med 2003; 33:395–405Crossref, Medline, Google Scholar
6. Henriksson MM, Aro HM, Marttunen MJ, Heikkinen ME, Isometsa ET, Kuoppasalmi KI, Lonnqvist JK: Mental disorders and comorbidity in suicide. Am J Psychiatry 1993; 150:935–940Link, Google Scholar
7. Kim C, Lesage A, Seguin M, Lipp O, Vanier C, Turecki G: Patterns of comorbidity in male suicide completers. Psychol Med 2003; 33:1299–1309Crossref, Medline, Google Scholar
8. Guze SB, Robins E: Suicide and primary affective disorders. Br J Psychiatry 1970; 117:437–438Crossref, Medline, Google Scholar
9. Blair-West GW, Cantor CH, Mellsop GW, Eyeson-Annan ML: Lifetime suicide risk in major depression: sex and age determinants. J Affect Disord 1999; 55:171–178Crossref, Medline, Google Scholar
10. Roy A: Family history of suicide. Arch Gen Psychiatry 1983; 40:971–974Crossref, Medline, Google Scholar
11. Barraclough BM, Pallis DJ: Depression followed by suicide: a comparison of depressed suicides with living depressives. Psychol Med 1975; 5:55–61Crossref, Medline, Google Scholar
12. Goldacre M, Seagroatt V, Hawton K: Suicide after discharge from psychiatric inpatient care. Lancet 1993; 342:283–286Crossref, Medline, Google Scholar
13. Brent DA, Perper JA, Moritz G, Baugher M, Schweers J, Roth C: Suicide in affectively ill adolescents: a case-control study. J Affect Disord 1994; 31:193–202Crossref, Medline, Google Scholar
14. Renaud J, Brent DA, Birmaher B, Chiappetta L, Bridge J: Suicide in adolescents with disruptive disorders. J Am Acad Child Adolesc Psychiatry 1999; 38:846–851Crossref, Medline, Google Scholar
15. Suominen K, Isometsä E, Suokas J, Haukka J, Achte K, Lönnqvist J: Completed suicide after a suicide attempt: a 37-year follow-up study. Am J Psychiatry 2004; 161:562–563Link, Google Scholar
16. Fawcett J, Scheftner WA, Fogg L, Clark DC, Young MA, Hedeker D, Gibbons R: Time-related predictors of suicide in major affective disorder. Am J Psychiatry 1990; 147:1189–1194Link, Google Scholar
17. Beck AT, Brown G, Berchick RJ, Stewart BL, Steer RA: Relationship between hopelessness and ultimate suicide: a replication with psychiatric outpatients. Am J Psychiatry 1990; 147:190–195Link, Google Scholar
18. Beck AT, Brown G, Steer RA: Prediction of eventual suicide in psychiatric inpatients by clinical ratings of hopelessness. J Consult Clin Psychol 1989; 57:309–310Crossref, Medline, Google Scholar
19. Beck AT, Steer RA, Kovacs M, Garrison B: Hopelessness and eventual suicide: a 10-year prospective study of patients hospitalized with suicidal ideation. Am J Psychiatry 1985; 142:559–563Link, Google Scholar
20. Malone KM, Szanto K, Corbitt EM, Mann JJ: Clinical assessment versus research methods in the assessment of suicidal behavior. Am J Psychiatry 1995; 152:1601–1607Link, Google Scholar
21. Pendse B, Westrin A, Engstrom G: Temperament traits in seasonal affective disorder, suicide attempters with non-seasonal major depression and healthy controls. J Affect Disord 1999; 54:55–65Crossref, Medline, Google Scholar
22. Weissman M, Fox K, Klerman GL: Hostility and depression associated with suicide attempts. Am J Psychiatry 1973; 130:450–455Abstract, Google Scholar
23. Stein D, Apter A, Ratzoni G, Har-Even D, Avidan G: Association between multiple suicide attempts and negative affects in adolescents. J Am Acad Child Adolesc Psychiatry 1998; 37:488–494Crossref, Medline, Google Scholar
24. Corruble E, Damy C, Guelfi JD: Impulsivity: a relevant dimension in depression regarding suicide attempts? J Affect Disord 1999; 53:211–215Crossref, Medline, Google Scholar
25. Soloff PH, Lis JA, Kelly T, Cornelius J, Ulrich R: Risk factors for suicidal behavior in borderline personality disorder. Am J Psychiatry 1994; 151:1316–1323Link, Google Scholar
26. Maiuro RD, O’Sullivan MJ, Michael MC, Vitaliano PP: Anger, hostility, and depression in assaultive vs suicide-attempting males. J Clin Psychol 1989; 45:531–541Crossref, Medline, Google Scholar
27. Windle M: Characteristics of alcoholics who attempted suicide: co-occurring disorders and personality differences with a sample of male Vietnam era veterans. J Stud Alcohol 1994; 55:571–577Crossref, Medline, Google Scholar
28. Burch EA Jr: Suicide attempt histories in alcohol-dependent men: differences in psychological profiles. Int J Addict 1994; 29:1477–1486Crossref, Medline, Google Scholar
29. Grosz DE, Lipschitz DS, Eldar S, Finkelstein G, Blackwood N, Gerbino-Rosen G, Faedda GL, Plutchik R: Correlates of violence risk in hospitalized adolescents. Compr Psychiatry 1994; 35:296–300Crossref, Medline, Google Scholar
30. Cheng AT, Mann AH, Chan KA: Personality disorder and suicide: a case-control study. Br J Psychiatry 1997; 170:441–446Crossref, Medline, Google Scholar
31. Brent DA, Johnson BA, Perper J, Connolly J, Bridge J, Bartle S, Rather C: Personality disorder, personality traits, impulsive violence, and completed suicide in adolescents. J Am Acad Child Adolesc Psychiatry 1994; 33:1080–1086Crossref, Medline, Google Scholar
32. Conner KR, Conwell Y, Duberstein PR: The validity of proxy-based data in suicide research: a study of patients 50 years of age and older who attempted suicide, II: life events, social support and suicidal behavior. Acta Psychiatr Scand 2001; 104:452–457Crossref, Medline, Google Scholar
33. Conner KR, Conwell Y, Duberstein PR, Eberly S: Aggression in suicide among adults age 50 and over. Am J Geriatr Psychiatry 2004; 12:37–42Crossref, Medline, Google Scholar
34. Ernst C, Lalovic A, Lesage A, Seguin M, Tousignant M, Turecki G: Suicide and no axis I psychopathology. BMC Psychiatry 2004; 4:7Crossref, Medline, Google Scholar
35. Kelly TM, Mann JJ: Validity of DSM-III-R diagnosis by psychological autopsy: a comparison with clinician ante-mortem diagnosis. Acta Psychiatr Scand 1996; 94:337–343Crossref, Medline, Google Scholar
36. Zhang J, Conwell Y, Wieczorek WF, Jiang C, Jia S, Zhou L: Studying Chinese suicide with proxy-based data: reliability and validity of the methodology and instruments in China. J Nerv Ment Dis 2003; 191:450–457Crossref, Medline, Google Scholar
37. Spitzer RL, Williams JBW, Gibbon M, First MB: The Structured Clinical Interview for DSM-III-R (SCID), I: history, rationale, and description. Arch Gen Psychiatry 1992; 49:624–629Crossref, Medline, Google Scholar
38. First MB, Spitzer RL, Gibbon M, Williams JBW: The Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II), part I: description. J Personal Disord 1995; 9:2Google Scholar
39. Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Ambrosini PJ, Tabrazi MA, Davies M: The assessment of affective disorders in children and adolescents by semistructured interview: test-retest reliability of the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present Episode Version. Arch Gen Psychiatry 1985; 42:696–702Crossref, Medline, Google Scholar
40. Kovacs M: The Children’s Depression Inventory (CDI). Psychopharmacol Bull 1985; 21:995–998Medline, Google Scholar
41. Brown GL, Goodwin FK: Cerebrospinal fluid correlates of suicide attempts and aggression. Ann NY Acad Sci 1986; 487:175–188Crossref, Medline, Google Scholar
42. Barratt ES: Barratt Impulsiveness Scale. Princeton, NJ, ETS Test Collection, Educational Testing Service, 1959Google Scholar
43. Cloninger CR, Przybeck TR, Svrakic DM, Wetzel RD: The Temperament and Character Inventory (TCI): A Guide to Its Development and Use. St Louis, Washington University, Center for Psychobiology of Personality, 1994Google Scholar
44. Plutchik R: Outward and inward directed aggressiveness: the interaction between violence and suicidality. Pharmacopsychiatry Suppl 1995; 2:47–57Crossref, Google Scholar
45. Lester D: Factors affecting choice of method of suicide. J Clin Psychol 1970; 26:437Crossref, Medline, Google Scholar
46. Heilä H, Isometsä ET, Henriksson MM, Heikkinen ME, Marttunen MJ, Lönnqvist JK: Suicide and schizophrenia: a nationwide psychological autopsy study on age- and sex-specific clinical characteristics of 92 suicide victims with schizophrenia. Am J Psychiatry 1997; 154:1235–1242Link, Google Scholar
47. Denning DG, Conwell Y, King D, Cox C: Method choice, intent, and gender in completed suicide. Suicide Life Threat Behav 2000; 31:367–385Google Scholar
48. Barratt E: Anxiety and impulsiveness related to psychomotor efficiency. Percept Mot Skills 1959; 9:191–198Crossref, Google Scholar
49. Principales causes de décès, Canada, 1997. Ottawa, Ont, Agence de santé publique du Canada, 1997. http://www.phac-aspc. gc.ca/publicat/lcd-pcd97/mrt_mf_f.htmlGoogle Scholar
50. Levy JC, Deykin EY: Suicidality, depression, and substance abuse in adolescence. Am J Psychiatry 1989; 146:1462–1467Link, Google Scholar
51. Bukstein OG, Brent DA, Perper JA, Moritz G, Baugher M, Schweers J, Roth C, Balach L: Risk factors for completed suicide among adolescents with a lifetime history of substance abuse: a case-control study. Acta Psychiatr Scand 1993; 88:403–408Crossref, Medline, Google Scholar
52. Brent DA, Johnson B, Bartle S, Bridge J, Rather C, Matta J, Connolly J, Constantine D: Personality disorder, tendency to impulsive violence, and suicidal behavior in adolescents. J Am Acad Child Adolesc Psychiatry 1993; 32:69–75Crossref, Medline, Google Scholar
53. Chignon JM, Cortes MJ, Martin P, Chabannes JP: Attempted suicide and alcohol dependence: results of an epidemiologic survey. Encephale 1998; 24:347–354Medline, Google Scholar
54. Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L: Age- and sex-related risk factors for adolescent suicide. J Am Acad Child Adolesc Psychiatry 1999; 38:1497–1505Crossref, Medline, Google Scholar
55. Pezawas L, Stamenkovic M, Jagsch R, Ackerl S, Putz C, Stelzer B, Moffat RR, Schindler S, Aschauer H, Kasper S: A longitudinal view of triggers and thresholds of suicidal behavior in depression. J Clin Psychiatry 2002; 63:866–873Crossref, Medline, Google Scholar
56. Malone KM, Haas GL, Sweeney JA, Mann JJ: Major depression and the risk of attempted suicide. J Affect Disord 1995; 34:173–185Crossref, Medline, Google Scholar
57. Mann JJ, Waternaux C, Haas GL, Malone KM: Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry 1999; 156:181–189Abstract, Google Scholar
58. Warshaw MG, Massion AO, Peterson LG, Pratt LA, Keller MB: Suicidal behavior in patients with panic disorder: retrospective and prospective data. J Affect Disord 1995; 34:235–247Crossref, Medline, Google Scholar
59. Friedman S, Smith L, Fogel A: Suicidality in panic disorder: a comparison with schizophrenic, depressed, and other anxiety disorder outpatients. J Anxiety Disord 1999; 13:447–461Crossref, Medline, Google Scholar
60. Placidi GPA, Oquendo MA, Malone KM, Brodsky B, Ellis SP, Mann JJ: Anxiety in major depression: relationship to suicide attempts. Am J Psychiatry 2000; 157:1614–1618Link, Google Scholar
61. Henriksson MM, Isometsa ET, Kuoppasalmi KI, Heikkinen ME, Marttunen MJ, Lonnqvist JK: Panic disorder in completed suicide. J Clin Psychiatry 1996; 57:275–281Medline, Google Scholar
62. Corbitt EM, Malone KM, Haas GL, Mann JJ: Suicidal behavior in patients with major depression and comorbid personality disorders. J Affect Disord 1996; 39:61–72Crossref, Medline, Google Scholar
63. Brodsky BS, Malone KM, Ellis SP, Dulit RA, Mann JJ: Characteristics of borderline personality disorder associated with suicidal behavior. Am J Psychiatry 1997; 154:1715–1719Link, Google Scholar
64. Isometsa ET, Henriksson MM, Heikkinen ME, Aro HM, Marttunen MJ, Kuoppasalmi KI, Lonnqvist JK: Suicide among subjects with personality disorders. Am J Psychiatry 1996; 153:667–673Link, Google Scholar
65. Foster T, Gillespie K, McClelland R, Patterson C: Risk factors for suicide independent of DSM-III-R axis I disorder: case-control psychological autopsy study in Northern Ireland. Br J Psychiatry 1999; 175:175–179Crossref, Medline, Google Scholar
66. Nace EP, Saxon JJ Jr, Shore N: A comparison of borderline and nonborderline alcoholic patients. Arch Gen Psychiatry 1983; 40:54–56Crossref, Medline, Google Scholar
67. Johnson JG, Cohen P, Skodol AE, Oldham JM, Kasen S, Brook JS: Personality disorders in adolescence and risk of major mental disorders and suicidality during adulthood. Arch Gen Psychiatry 1999; 56:805–811Crossref, Medline, Google Scholar
68. Joyce PR, Mulder RT, Luty SE, McKenzie JM, Sullivan PF, Cloninger RC: Borderline personality disorder in major depression: symptomatology, temperament, character, differential drug response, and 6-month outcome. Compr Psychiatry 2003; 44:35–43Crossref, Medline, Google Scholar



