Toward a Neuropsychological Theory of Antidepressant Drug Action: Increase in Positive Emotional Bias After Potentiation of Norepinephrine Activity
Abstract
OBJECTIVE: Antidepressants that increase serotonin or norepinephrine in the brain are effective in treating depression, but there is no neuropsychological account of how these changes relieve depressive states. Cognitive theories suggest that biases in information processing lead depressed patients to make unrealistically negative judgments about themselves and the world. METHOD: A single dose of the noradrenergic antidepressant reboxetine or placebo was administered to 24 healthy volunteers. Effects on emotional processing were assessed through facial expression recognition, emotional categorization, and emotional memory. RESULTS: On the three measures, reboxetine biased perception toward positive, rather than negative, information in the absence of changes in nonemotional performance or mood. CONCLUSIONS: These results suggest that a single dose of an antidepressant can increase the processing of positively valenced material in nondepressed volunteers. Antidepressants may therefore work in a manner similar to that of psychological treatments that aim to redress negative biases in information processing.
Although many studies have confirmed the efficacy of noradrenergic drugs in the treatment of depression (1), the mechanism by which increasing levels of this neurotransmitter improve the psychological symptoms of low mood, feelings of worthlessness, and poor social function remains to be elucidated. Patients suffering from depression show negative biases in perception and memory, and such biases are believed to play a fundamental role in the maintenance of mood disorders (2).
Both antidepressants and cognitive therapies relieve depressive symptoms, with full recovery taking a number of weeks. Cognitive behavior therapy explicitly seeks to change conscious biases in the processing of emotional cognitions (2). However, the effects of antidepressant drug administration on negative biases in depression are usually thought to reflect nonspecific, and secondary, consequences of mood improvement (3). In this study, we assessed the effect of a single dose of the antidepressant reboxetine, a selective norepinephrine reuptake inhibitor, on three measures of emotional processing in healthy volunteers. Healthy volunteers were chosen to control for the effects of depression and mood improvement following antidepressant administration.
Method
The study subjects were 24 volunteers (12 male) between the ages of 20 and 47 years. Volunteers were screened to exclude current or previous history of psychiatric disorder, substance abuse, and serious physical and neurological problems. They were free of medication apart from contraceptive pills.
This study was approved by the local ethics committee. After complete description of the study to the subjects, written informed consent was obtained.
The volunteers fasted from 8:00 a.m., and the testing session started at 12:00 noon. After a 30-minute baseline period, the volunteers received either 4 mg of reboxetine or placebo in a double-blind, randomized, between-groups design. These two groups were matched on age (mean=31.7 years, SD=2.8, and mean=30.3 years, SD=2.3), gender, and IQ (National Adult Reading Test score: mean=119, SD=2, and mean=117, SD=3).
Psychological testing began 2 hours after administration of reboxetine (in line with the pharmacokinetics of reboxetine, for which peak drug levels are attained within 2 hours).
Recognition of facial expression was assessed as previously described (4). Facial expressions associated with five emotions (anger, disgust, fear, happiness, sadness) were presented. These had been averaged by using computer graphic techniques between 100% emotion and neutral in 10% steps (40 examples of each emotion were therefore presented). Each of the 10 actors was also presented while showing a neutral facial expression. Each stimulus remained on the screen for 500 msec, after which the volunteers responded by pressing labeled keys.
To assess emotional categorization, 60 personality characteristics selected to be extremely unlikable or likable (5) were presented on the computer screen for 500 msec (matched on word length, frequency, and meaningfulness). The volunteers were asked to categorize these personality traits as likable or unlikable as quickly and as accurately as possible.
Emotional memory was examined by a surprise test of recall of the personality traits used in the emotional categorization task, immediately after task completion. The number of items recalled for each valence (minus false positives) was calculated.
Memory was measured with the Rey Auditory Verbal Learning Test (6). Recall over five repetitions of a 15-item word list was assessed first and was then followed by delayed recall and recognition of the same items.
The subjects also performed the Rapid Visual Information Processing Task (from CANTAB, CeNeS Pharmaceuticals, Cambridge, U.K.). Digits between 1 and 9 were presented in the center of the screen at a rate of 200 per minute for 7 minutes. The subjects were asked to detect any one of three specified digit sequences (3-5-7, 2-4-6, or 4-6-8). The speed and number of correct detections and responses made in the absence of appropriate stimuli (false alarms) were recorded.
Mood and subjective state were monitored at baseline, 2 hours, and 4 hours by using visual analogue scales for happy, sad, frightened, angry, disgusted, alert, and anxious.
Results
The facial expression task revealed greater recognition of happy facial expressions after reboxetine than after placebo in the absence of differences in the recognition of other basic emotions (Figure 1, left side). There was a significant interaction of group and happiness intensity (F=8.1, df=4, 88, p<0.001). As shown in Figure 1 (right side), there was a difference in the accurate identification of low levels of happiness. This was not a difference in response bias (indiscriminate labeling of faces as “happy”) as the effect remained in a signal detection analysis (t=3.0, df=22, p=0.007).
In the emotional categorization task, the volunteers receiving reboxetine had a greater difference between the times for their responses to positive descriptors (mean=421 msec, SD=56) and negative descriptors (mean=552, SD=80) than did those receiving placebo (positive: mean=499 msec, SD=51; negative: 514 msec, SD=44), and the interaction of valence and group was significant (F=5.3, df=1, 22, p=0.03). In the surprise recall test, the placebo group remembered fewer positive descriptors (mean=3.5, SD=0.6) than negative descriptors (mean=5.1, SD=0.8), whereas this “negative” bias was not present in the volunteers receiving reboxetine (positive: mean=5.6, SD=0.8; negative: mean=5.4, SD=0.7) (F=4.8, df=1, 22, p=0.04).
In contrast to the processing of emotional information, the processing of nonemotional information was not affected by reboxetine (p>0.4), suggesting that the better performance found in the emotional tasks does not represent more global actions on speed, memory, or attention. There was also no effect of reboxetine on ratings of subjective state (p>0.4), and inclusion of these mood ratings as covariates did not abolish the effects on happiness recognition (F=5.6, df=1, 15, p=0.03), emotional categorization (F=5.3, df=1, 15, p=0.04), or emotional memory (F=5.3, df=1, 15, p=0.04).
Discussion
Administration of a single clinical dose of the antidepressant reboxetine was found to facilitate the processing of positively valenced emotional information in healthy volunteers in the absence of improved cognitive performance. This shift in information processing represents an early effect of antidepressant medication that could act to reverse the negative biases in perception seen in depressed patients (2).
The therapeutic effects of antidepressant drugs are usually described as needing 2 or more weeks of treatment, and the apparent delay in action has led to speculation that slowly evolving molecular adaptive processes are required before effects on mood and anxiety are expressed (7). Our findings suggest that changes in emotional processing may be found after a single administration of an antidepressant. This raises the interesting hypothesis that differences in the processing of external cues (e.g., positive social stimuli) and internal cues (e.g., positive memories) may occur early in the course of antidepressant treatment, but that interaction with the environment is required before these processing biases lead to clinically improved mood.
This effect of reboxetine suggests that psychological and neuropharmacological theories of depression may be convergent. Psychological theories emphasize the importance of reducing negative cognitions and information processing biases in the treatment of mood disorder (2). The current results suggest that antidepressant administration may have similar effects on information processing through a pharmacological mechanism. We have recently obtained data suggesting a similar effect on the recognition of happy facial expressions for another class of antidepressants, the selective serotonin reuptake inhibitors (4), which have comparable clinical efficacy in mood disorders (8) and which have been reported to increase affiliative behaviors in healthy volunteers (9). Increasing knowledge of the neurobiological mechanisms involved in emotional processing could lead to novel antidepressant treatments as well as innovative strategies that combine the key therapeutic elements of pharmacological and psychological approaches.
Received July 31, 2002; revision received Nov. 1, 2002; accepted Nov. 25, 2002. From the University of Oxford, Department of Psychiatry, Warneford Hospital. Address reprint requests to Dr. Harmer, University Department of Psychiatry, Warneford Hospital, Oxford OX3 7JX, United Kingdom; [email protected] (e-mail). Supported by a Medical Research Council U.K. training fellowship (Dr. Harmer).
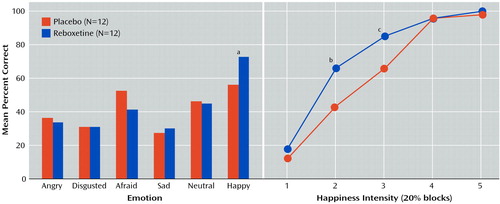
Figure 1. Accuracy of Recognition of Six Facial Expressions and Recognition of Happy Expressions in Relation to Happiness Intensity for 24 Healthy Volunteers Given a Single Dose of Reboxetine or Placebo
aSignificant difference between groups (t=3.3, df=22, p=0.003).
bSignificant difference between groups (t=3.7, df=22, p=0.001).
cSignificant difference between groups (t=4.0, df=22, p=0.001).
1. Schatzberg AF: Clinical efficacy of reboxetine in major depression. J Clin Psychiatry 2000; 61(suppl 10):31-38Medline, Google Scholar
2. Beck AT, Rush AJ, Shaw BF, Emery G: Cognitive Therapy of Depression. New York, Guilford, 1979Google Scholar
3. Peselow ED, Robins C, Block P, Barouche F, Fieve RR: Dysfunctional attitudes in depressed patients before and after clinical treatment and in normal control subjects. Am J Psychiatry 1990; 147:439-444Link, Google Scholar
4. Harmer CJ, Bhagwagar Z, Perrett DI, Vollm BA, Cowen PJ, Goodwin GM: Acute SSRI administration affects the processing of social cues in healthy volunteers. Neuropsychopharmacology 2003; 28:148-152Crossref, Medline, Google Scholar
5. Anderson NH: Likableness ratings of 555 personality-trait words. J Pers Soc Psychol 1968; 9:272-279Crossref, Medline, Google Scholar
6. Rey A: L’examen de clinique en psychologie. Paris, Presses Universitaires de France, 1964Google Scholar
7. Reid IC, Stewart CA: How antidepressants work: new perspectives on the pathophysiology of depressive disorder. Br J Psychiatry 2001; 178:299-303Crossref, Medline, Google Scholar
8. Kent JM, Coplan JD, Gorman JM: Clinical utility of the selective serotonin reuptake inhibitors in the spectrum of anxiety. Biol Psychiatry 1998; 44:812-824Crossref, Medline, Google Scholar
9. Knutson B, Wolkowitz OM, Cole SW, Chan T, Moore EA, Johnson RC, Terpstra J, Turner RA, Reus VI: Selective alteration of personality and social behavior by serotonergic intervention. Am J Psychiatry 1998; 155:373-379Link, Google Scholar



