Geriatric Psychiatry Versus General Psychiatry Inpatient Treatment of the Elderly
Abstract
OBJECTIVE: The authors compared the clinical treatment given older psychiatric inpatients on a geriatric psychiatry unit and a general psychiatry unit. METHOD: The charts of 50 randomly selected general psychiatry inpatients over the age of 65 years and 50 inpatients from the geriatric psychiatry unit who were matched for age, gender, and primary diagnosis were reviewed. RESULTS: Significantly greater percentages of older inpatients treated on the geriatric psychiatry unit received complete organic medical workups, structured cognitive assessment, aging-sensitive aftercare referral, and monitoring of psychopharmacological side effects and blood levels than comparable patients on a general psychiatry unit. CONCLUSIONS: Geriatric psychiatry subspecialty inpatient care appears to be associated with distinct clinically relevant assessment and treatment advantages. Continuing geropsychiatric education of general psychiatrists is indicated.
Over the last two decades, geriatric psychiatry has emerged as an organized subdiscipline within psychiatry. Accreditation of geriatric psychiatry R-5 residency (fellowship) programs by the Accreditation Council for Graduate Medical Education as well as certification for added qualifications in geriatric psychiatry by the American Board of Psychiatry and Neurology have helped to more formally legitimize the subspecialty. General psychiatry residency training requires a geriatric psychiatry experience. In addition, an impressive body of evidence-based clinical knowledge specific to the behavioral health care of the elderly is now increasingly available.
However, to our knowledge, studies demonstrating potential clinical advantages of subspecialty geropsychiatry services over general psychiatric care of elderly patients are limited. In contrast, comparisons of specialized geriatric medicine with general medicine practice settings are more developed. For example, subspecialty geriatric medicine programming has been associated with clinical benefits compared with general medical environments in both acute inpatient and outpatient settings (1–4). In long-term-care settings, some, albeit not all, studies examining outcomes associated with “special care units” for dementia have reported clinical advantages of the specialized environment (5–7).
In view of these findings, we compared several measures of treatment of elderly psychiatric inpatients hospitalized on a specialized geriatric psychiatry unit compared with elderly psychiatric inpatients on a general psychiatry unit in the same hospital.
Method
A retrospective inpatient chart review was conducted of psychiatrically hospitalized patients 65 years of age or older at Hillside Hospital (now The Zucker Hillside Hospital), the psychiatric division of Long Island Jewish Medical Center in Glen Oaks, N.Y. Zucker Hillside Hospital is a 208-bed psychiatric hospital, which at the time of the study (1997–1998) included a dedicated 20-bed geriatric psychiatry unit and eight additional cluster beds for geropsychiatric patients on a contiguous unit. These 28 beds were medically staffed by Geriatric Psychiatry Division attending geropsychiatrists. In “overflow” circumstances, when the dedicated geriatric psychiatry beds were full (including the admission of patients over census to absolute capacity), elderly patients in need of psychiatric hospitalization were routinely admitted to regular general psychiatry units. General psychiatry beds are staffed by attending general psychiatrists who are not part of the Geriatric Psychiatry Division.
A computer printout of all patients 65 years or older who were hospitalized between January 1996 and June 1997 was requested from the statistical computing section of Hillside Hospital. Date of birth, assigned unit, gender, and diagnosis were included. Fifty randomly selected patient identification numbers were then taken from the general psychiatry unit and matched for age, sex, and primary diagnosis to 50 identification numbers from the dedicated geriatric psychiatry unit.
The medical records of these 100 patients were systematically reviewed by a geriatric psychiatry fellow (I.C.Y.) for the following information: 1) completeness of organic workup (chemistry screen, CBC, RPR, thyroid function tests, B12/folic acid levels, brain imaging), 2) cognitive screening (brief standardized testing, full neuropsychological battery), 3) documentation of psychotropic blood level monitoring for relevant psychotropics (e.g., lithium, mood stabilizers, tricyclic antidepressants), 4) documentation of psychotropic drug side effect monitoring, including orthostatic hypotension, neuroleptic-related extrapyramidal symptoms, tricyclic antidepressant-related anticholinergic side effects, tricyclic antidepressant-related ECG changes, and side effects of selective serotonin reuptake inhibitors, other antidepressants, mood stabilizers, and benzodiazepines, 5) number of ECT treatments/episode, 6) discharge follow-up arrangement (to specialized geriatric versus general psychiatric services), and 7) length of stay.
Two-tailed chi-square and t tests were used to compare these clinical measures between elderly patients who were admitted to the geriatric psychiatry unit and those admitted to the general psychiatry unit.
Results
The mean age of patients in both treatment settings was 76.0 years (SD=6). There were 29 women and 21 men in each group. Primary diagnoses of patients in each setting were major depressive disorder (N=28 [56%]), bipolar disorder (N=7 [14%]), psychotic disorder (N=8 [16%]), and dementia with behavioral disturbance (N=7 [14%]). In general, diagnostic workup procedures and psychotropic monitoring measures were significantly more comprehensive and regularly documented in the records of patients in the geropsychiatry subspecialty inpatient setting than the general psychiatry setting.
Comparisons of diagnostic and treatment variables between the geriatric psychiatry and general psychiatry inpatient units are illustrated in Figure 1. A complete organic workup was documented for 18 (36%) patients in the geriatric psychiatry unit and seven (14%) in the general psychiatry unit. Brief standardized testing was documented for 35 (70%) of the patients in the geriatric unit and five (10%) of the patients in the general unit. Full neuropsychological battery testing was documented for 15 (30%) of the patients in the geriatric unit and two (4%) in the general unit. Psychotropic blood level monitoring was documented for all 19 of the patients in the geriatric unit and 15 (80%) of the 19 patients in the general unit who were taking blood-level-relevant psychotropics. Discharge to geropsychiatric specialty services was documented for 34 (79%) of the 43 patients discharged from the geriatric unit and 18 (44%) of the 41 patients discharged from the general unit. Monitoring of the side effect of orthostatic hypotension was documented for 44 (88%) of the patients on the geriatric unit and 22 (44%) of those on the general unit. Monitoring of this side effect was also documented for 26 (93%) of the 28 patients on the geriatric unit and 12 (46%) of the 26 patients in the geriatric psychiatry unit who were taking neuroleptics and for both of the patients on the geriatric unit and three of the 10 patients on the general unit who were taking tricyclic antidepressants. Monitoring of neuroleptic-related extrapyramidal symptoms was documented for 22 (79%) of the 28 patients on the geriatric unit and five (19%) of the 26 patients on the general unit who were taking neuroleptics. Monitoring of tricyclic-related anticholinergic side effects was not documented in either of the patients on the geriatric unit and in one of the 10 patients on the general unit who were taking tricyclic antidepressants. Monitoring of tricyclic-related ECG effects was documented in one of the two patients on the geriatric unit and none of the 10 patients on the general unit taking tricyclics. Monitoring of the side effects of SSRIs was documented in seven (50%) of the 14 patients on the geriatric unit and one (8%) of the 12 on the general unit who were taking SSRIs. Monitoring of the side effects of other antidepressants was documented in nine (43%) of the 21 patients on the geriatric unit and one (4%) of the 23 on the general unit who were taking other antidepressants. Monitoring of the side effects of mood stabilizers was documented in six (38%) of the 16 patients on the geriatric unit and one (8%) of the 13 on the general unit who were taking mood stabilizers. Monitoring of the side effects of benzodiazepines was documented in one (8%) of the 13 patients on the geriatric unit and one (4%) of the 23 on the general unit who were taking benzodiazepines.
The mean number of ECTs per episode given to the nine patients on the geriatric psychiatry unit who received ECT was 7.3 (range=3–12), compared with 4.6 per episode (range=1–8) for the 11 patients on the general psychiatry unit given ECT. The mean length of stay for the 50 patients on the geriatric unit was 29.9 days (mean or range=8–104), compared with 25.8 days (mean or range=4–78) for the 50 patients on the general unit. These between-unit differences were not significant.
Discussion
Findings from this retrospective pilot study suggest that clinical advantages are likely associated with geriatric psychiatry subspecialty care in the areas of completeness of diagnostic assessment, psychotropic practices (side effect monitoring, blood level monitoring), routinization of cognitive assessments, appropriateness of number of ECT treatments per episode, and age-specific aftercare referral. However, because outcome measures related to clinical benefit were not considered, conclusions cannot be drawn about the actual clinical significance of more detailed assessments, monitoring, and geriatric-sensitive treatment decision making. In addition, other than a nonsignificantly longer length of stay in the geriatric psychiatry unit, measures of costs per setting were not taken into account. Therefore, cost effectiveness of highlighted geropsychiatric subspecialty practices cannot be analyzed. Future prospective studies addressing possible benefits of subspecialty geriatric psychiatry care should incorporate short-term and long-term outcome indicators and cost estimates into their study design.
Although the subspecialty geriatric psychiatry setting demonstrated significantly more attentive clinical practices in regard to the care of elderly psychiatric patients, lapses in either consistently vigilant side effect monitoring or its documentation were not uncommon. Thus, geropsychiatric care in both geriatric psychiatry subspecialty and general psychiatry inpatient settings would likely benefit from standardized treatment algorithms requiring that key information (such as orthostatic blood pressure or cognitive examination) be recorded on formatted progress notes.
Since the need for trained geriatric psychiatrists exceeds the supply (8), general psychiatrists will continue to play a critical role in geriatric mental health service delivery. Current findings suggest that geriatric psychopharmacology, use of ECT in the elderly, comprehensive geropsychiatric and organic/dementia assessment, and community resources for the aged should be foci of continuing education efforts for general psychiatrists.
The results presented here must be considered preliminary. Data were gleaned from a single geriatric psychiatry inpatient setting and from only one institution by a single medical chart reviewer who was not blind to the treatment unit. Although patients were matched for diagnosis, frequencies of diagnoses in the two settings may have differed (e.g., more dementia patients on the geriatric psychiatry unit; more bipolar and psychotic disorder patients on the general units). Because the geriatric psychiatry and general psychiatry units at Hillside Hospital often function as tertiary care referral centers, more difficult, refractory cases are often admitted; these patients may not represent geropsychiatry inpatients typically encountered in community hospital settings. Results are also based on what information was documented in the medical record. It is conceivable that some of the treatment variables considered were evaluated but not documented. Additional nonretrospective survey methods that incorporate M.D. and R.N. interviewing may help address this issue in future studies.
Optimal treatment of older people is dependent on awareness of aging-related biological changes and psychosocial vulnerabilities and strengths. General adult health care environments often lack appreciation of the unique needs of the elderly. For example, a review of emergency psychiatric services for the elderly (9) concluded that several barriers to comprehensive assessment and treatment of geropsychiatric emergencies exist in typical general hospital emergency settings. Current data validate the importance of geriatric psychiatry as an inpatient subspecialty with clinical applications that translate into more attentive patient care practices for older people. Further studies comparing practice behaviors of geropsychiatrists and general psychiatrists in other settings that treat older patients are indicated.
Received Dec. 10, 2002; revision received Aug. 11, 2003; accepted Aug. 14, 2003. From the Division of Geriatric Psychiatry, Department of Psychiatry, Zucker Hillside Hospital, Long Island Jewish Medical Center, North Shore-Long Island Jewish Health System, Glen Oaks, N.Y. Address reprint requests to Dr. Greenwald, Zucker Hillside Hospital, 75-59 263rd St., Glen Oaks, NY 11004; [email protected] (e-mail).
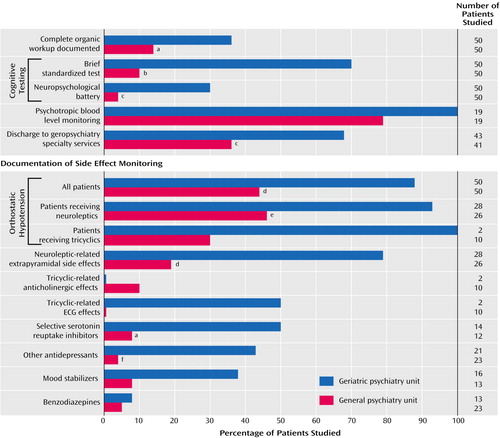
Figure 1. Comparison of Clinical Assessment/Treatment Variables Documented in the Charts of Elderly Inpatients on a Geriatric Psychiatry Unit and a General Psychiatry Unit
ap≤0.05, chi-square test.
bp≤0.001, chi-square test.
cp≤0.002, chi-square test.
dp≤0.0001, chi-square test.
ep≤0.0005, chi-square test.
fp≤0.01, chi-square test.
1. Cohen HJ, Feussner JR, Weinberger M, Carnes M, Handy RC, Hsieh F, Phibbs C, Courtney D, Lyles KW, May C, McMurtry C, Pennypacker L, Smith DM, Ainslie N, Hornick T, Brodkin K, Lavori P: A controlled trial of inpatient and outpatient geriatric evaluation and management. N Engl J Med 2002; 346:905–912Crossref, Medline, Google Scholar
2. Silverman M, Musa D, Martin DC, Lave JR, Adams J, Ricci EM: Evaluation of outpatient geriatric assessment: a randomized multi-site trial. J Am Geriatr Soc 1995; 43:733–740Crossref, Medline, Google Scholar
3. Rubenstein LZ, Stuck AE, Siu AL, Wieland D: Impacts of geriatric evaluation and management programs on defined outcomes: overview of the evidence. J Am Geriatr Soc 1991; 39(9, part 2):8S-16SGoogle Scholar
4. Rubenstein LZ, Josephson KR, Wieland GD, English PA, Sayre JA, Kane RL: Effectiveness of a geriatric evaluation unit: a randomized clinical trial. N Engl J Med 1984; 311:1664–1670Crossref, Medline, Google Scholar
5. Sloane PD, Mathew LJ, Scarborough M, Desai JR, Koch GG, Tangen C: Physical and pharmacological restraint of nursing home patients with dementia. JAMA 1991; 265:1278–1282Crossref, Medline, Google Scholar
6. Benson DM, Cameron D, Humbach E, Servino L, Gambert SR: Establishment and impact of a dementia unit within a nursing home. J Am Geriatr Soc 1987; 35:319–323Crossref, Medline, Google Scholar
7. Sloane PD, Lindeman DA, Phillips C, Moritz DJ, Koch G: Evaluating Alzheimer’s special care units: reviewing the evidence and identifying potential sources of study bias. Gerontologist 1995; 35:103–111Crossref, Medline, Google Scholar
8. Jeste DV, Alexopoulos GS, Bartels SJ, Cummings JL, Gallo JJ, Gottlieb GL, Halpain MC, Palmer BW, Patterson TL, Reynolds CF III, Lebowitz BD: Consensus statement on the upcoming crisis in geriatric mental health: research agenda for the next 2 decades. Arch Gen Psychiatry 1999; 56:848–853Crossref, Medline, Google Scholar
9. Colenda CC, Greenwald BS, Crossett JH, Husain MM, Kennedy GJ: Barriers to effective psychiatric emergency services for elderly persons. Psychiatr Serv 1997; 48:321–325Link, Google Scholar



