Treating Acute Stress Disorder Following Mild Traumatic Brain Injury
Abstract
OBJECTIVE: Acute stress disorder permits early identification of trauma survivors who are at risk of developing chronic posttraumatic stress disorder (PTSD). This study aimed to prevent PTSD in people who developed acute stress disorder after a mild brain injury by early provision of cognitive behavior therapy. METHOD: Twenty-four civilian trauma survivors with acute stress disorder were given five individually administered sessions of either cognitive behavior therapy or supportive counseling within 2 weeks of their trauma. RESULTS: Fewer patients receiving cognitive behavior therapy than supportive counseling met criteria for PTSD at a posttreatment evaluation (8% versus 58%, respectively). There were also fewer cases of PTSD at a 6-month follow-up evaluation among those receiving cognitive behavior therapy (17%) than among those receiving supportive counseling (58%). Patients in the cognitive behavior therapy condition displayed less reexperiencing and avoidance symptoms at the follow-up evaluation than patients receiving supportive counseling. CONCLUSIONS: These findings suggest that PTSD following mild brain injury can be effectively prevented with early provision of cognitive behavior therapy.
Acute stress disorder describes posttraumatic stress reactions that occur within 1 month of a trauma (1). Approximately 80% of people with acute stress disorder develop posttraumatic stress disorder (PTSD) (2). Two previous treatment studies have demonstrated that only 20% of patients with acute stress disorder who received brief cognitive behavior therapy have PTSD 6 months later (3, 4). Among patients whose acute stress disorder occurs following a mild traumatic brain injury, approximately 80% develop chronic PTSD (5, 6). Mild brain injury includes loss of consciousness at the time of trauma and potentially some degree of cognitive impairment (7). Considering that cognitive behavior therapy involves exposure to trauma memories and cognitive restructuring, the effects of mild brain injury may impede the efficacy of cognitive behavior therapy in these patients. To our knowledge, there have been no controlled treatment studies of acute stress disorder or PTSD following mild brain injury. The current study tested the efficacy of cognitive behavior therapy in preventing PTSD in patients who develop acute stress disorder following mild brain injury by providing these patients with either cognitive behavior therapy or supportive counseling.
Method
Patients were survivors of either motor vehicle accidents or nonsexual assaults who were referred from hospital staff and mental health centers to the PTSD Unit at Westmead Hospital. Inclusion criteria were 1) trauma occurrence within the preceding 2 weeks, 2) acute stress disorder criteria met, 3) English proficiency, 4) age between 18 and 60 years, and 5) trauma involved mild brain injury, which was defined as posttraumatic amnesia of less than 24 hours and Glasgow Coma Scale score of 13–15, which reflects minimal disruption to consciousness (7). Posttraumatic amnesia was defined as the period of anterograde amnesia before events that occur after the trauma are recalled in a continuous manner.
Twenty-four patients entered the study, and all were retained for the 6-month follow-up evaluation. The cognitive behavior therapy group comprised four men and eight women (mean age=29.42 years, SD=13.93), and the supportive counseling group comprised four men and eight women (mean age=33.00 years, SD=14.37). Prior psychiatric diagnoses were noted in two cognitive behavior therapy patients (major depression, bulimia nervosa) and two supportive counseling patients (major depression, attention deficit disorder).
Acute stress disorder was assessed by using the Acute Stress Disorder Interview (8). Patients were administered the Impact of Event Scale (9), the Beck Depression Inventory (10), and the Beck Anxiety Inventory (11). PTSD was assessed by using the Clinician Administered PTSD Scale, Form 2 (12). Before treatment, patients rated their confidence in treatment (1=“not at all confident,” 10=“extremely confident”).
Written informed consent, as approved by the University of New South Wales Human Research Ethics Committee, was obtained prior to study entry. Patients were assessed at pretreatment, posttreatment (within 1 week of treatment completion), and at a 6-month follow-up evaluation by a clinical psychologist who was blind to treatment condition. All measures were administered at each assessment except that the Acute Stress Disorder Interview was administered at pretreatment and the Clinician Administered PTSD Scale, Form 2, was administered at posttreatment and the follow-up evaluation. Patients were randomly assigned, through a process of minimization stratified on gender and severity of acute stress disorder, to receive cognitive behavior therapy or supportive counseling. Each group received five 1½-hour individually administered weekly sessions conducted by clinical psychologists, who followed therapist manuals (available from the first author).
The cognitive behavior therapy program comprised 1) education about trauma reactions, 2) progressive muscle relaxation training, 3) imaginal exposure to traumatic memories, 4) cognitive restructuring, and 5) graded in vivo exposure to avoided situations. Fifty minutes of imaginal exposure to trauma memories was performed during each session and also as daily homework. The supportive counseling program comprised education about trauma and general problem-solving skills.
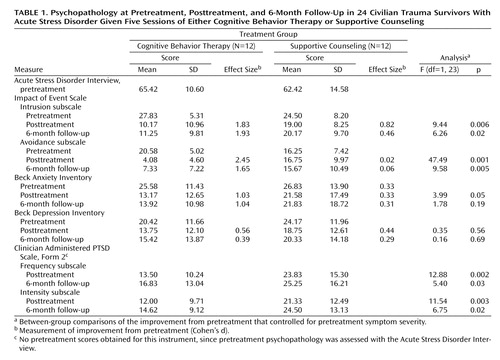
Analyses of covariance (ANCOVA) that controlled for pretreatment symptom severity were conducted for posttreatment and 6-month follow-up scores on the Clinician Administered PTSD Scale (intensity and frequency subscales), Impact of Event Scale (intrusions and avoidance subscales), and the Beck Depression Inventory and Beck Anxiety Inventory. We derived Cohen’s d effect size by calculating the mean difference between assessments of each treatment condition and dividing this by the pooled standard deviation (13) and then used Hedges G effect sizes to correct for variations due to small patient group sizes (14).
Results
All sessions were audiotaped, and 16 therapy sessions (13% of the 120 sessions) were rated by two independent raters for 33 treatment components that were rated as present or absent. Sessions were also scored for proficiency (0=“unacceptable,” 6=“superior”). No supportive counseling session included exposure, cognitive restructuring, or anxiety management. The mean rating for exposure, cognitive restructuring, and anxiety management in the cognitive behavior therapy conditions was 5.1 (SD=1.3).
Planned comparisons indicated that before treatment, groups did not differ in terms of age, trauma assessment interval, pretreatment severity of acute stress disorder, treatment confidence ratings, or scores on the Impact of Event Scale, Beck Depression Inventory, or Beck Anxiety Inventory.
Chi-square tests indicated that at posttreatment, fewer patients met criteria for PTSD in the cognitive behavior therapy group (8%, N=1) than in the supportive counseling group (58%, N=7) (χ2=6.75, df=1, p<0.05, with Yates’s correction [15]). At the 6-month follow-up evaluation, fewer patients met criteria for PTSD in the cognitive behavior therapy group (17%, N=2) than in the supportive counseling group (58%, N=7) (χ2=4.44, df=1, p<0.05). The effect sizes of the different proportion of patients reporting PTSD was considerable at posttreatment (1.16) and follow-up (0.87).
Table 1 presents the psychopathology scores over the course of the study and the effect sizes of the improvement from pretreatment to posttreatment and from pretreatment to the 6-month follow-up evaluation. At posttreatment, ANCOVAs indicated significant effects for scores on the intrusions and avoidance subscales of the Impact of Event Scale, the Beck Anxiety Inventory, and the frequency and intensity subscales of the Clinician Administered PTSD Scale. There was no effect for Beck Depression Inventory scores. At the 6-month follow-up evaluation, ANCOVAs indicated main effects for scores on the intrusions and avoidance subscales of the Impact of Event Scale and the frequency and intensity subscales of the Clinician Administered PTSD Scale. There were no effects for Beck Depression Inventory or Beck Anxiety Inventory scores.
Discussion
This study demonstrates that brief cognitive behavior therapy is an effective intervention for patients who sustain a mild brain injury. The presence of partial amnesia of the trauma as a result of impaired loss of consciousness did not reduce the efficacy of strategies involving prolonged exposure to trauma memories, cognitive restructuring, and anxiety management. In contrast to previous results (4), depression was not markedly improved with cognitive behavior therapy. Depression is common after brain injury (8), and the presence of cognitive deficits, postconcussive syndrome, or other sequelae of brain injury may have led to persistent depression in our patients.
We emphasize that these conclusions are limited by the small study group size. Further, we did not index cognitive impairment, and this may influence treatment response following brain injury. The higher rate of PTSD in the cognitive behavior therapy group at the 6-month follow-up evaluation (17%) than at posttreatment (8%) suggests subsequent follow-up evaluations are needed to index longer-term effects of cognitive behavior therapy. These limitations notwithstanding, these results indicate that early intervention for patients who develop acute stress disorder after mild brain injury can lead to significant reductions in PTSD. Considering the prevalence of mild brain injury sustained in traumatic contexts, early application of cognitive behavior therapy for those who are at risk of PTSD may have significant public health benefits.
 |
Received Nov. 27, 2001; revision received Aug. 29, 2002; accepted Sept. 19, 2002. From the School of Psychology, University of New South Wales. Address reprint requests to Dr. Bryant, School of Psychology, University of New South Wales, Sydney NSW 2052, Australia; [email protected] (e-mail). Supported by a grant from the Motor Accident Authority of New South Wales.
1.. Bryant RA, Harvey AG: Acute stress disorder: a critical review of diagnostic issues. Clin Psychol Rev 1997; 17:757-773Crossref, Medline, Google Scholar
2.. Harvey AG, Bryant RA: The relationship between acute stress disorder and posttraumatic stress disorder following motor vehicle accidents. J Consult Clin Psychol 1998; 66:507-512Crossref, Medline, Google Scholar
3.. Bryant RA, Harvey AG, Sackville T, Dang ST, Basten C: Treatment of acute stress disorder: a comparison of cognitive-behavioral therapy and supportive counseling. J Consult Clin Psychol 1998; 66:862-866Crossref, Medline, Google Scholar
4.. Bryant RA, Sackville T, Dang ST, Moulds M, Guthrie R: Treating acute stress disorder: an evaluation of cognitive behavior therapy and supportive counseling techniques. Am J Psychiatry 1999; 156:1780-1786Abstract, Google Scholar
5.. Bryant RA, Harvey AG: Relationship between acute stress disorder and posttraumatic stress disorder following mild traumatic brain injury. Am J Psychiatry 1998; 155:625-629Link, Google Scholar
6.. Bryant RA: Posttraumatic stress disorder and traumatic brain injury: can they co-exist? Clin Psychol Rev 2001; 21:931-948Crossref, Medline, Google Scholar
7.. American Congress of Rehabilitation Medicine: Definition of mild traumatic brain injury. J Head Trauma Rehab 1993; 8:86-87Crossref, Google Scholar
8.. Bryant RA, Harvey AG, Dang ST, Sackville T: Assessing acute stress disorder: psychometric properties of a structured clinical interview. Psychol Assess 1998; 10:215-220Crossref, Google Scholar
9.. Horowitz MJ, Wilner N, Alvarez W: Impact of Event Scale: a measure of subjective stress. Psychosom Med 1979; 41:209-218Crossref, Medline, Google Scholar
10.. Beck AT, Steer RA, Brown GK: Beck Depression Inventory, 2nd ed, Manual. San Antonio, Tex, Psychological Corp, 1996Google Scholar
11.. Beck AT, Steer RA: Beck Anxiety Inventory. San Antonio, Tex, Psychological Corp, 1993Google Scholar
12.. Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM: The development of a Clinician-Administered PTSD Scale. J Trauma Stress 1995; 8:75-90Crossref, Medline, Google Scholar
13.. Cohen J: Statistical Power Analysis for the Behavioral Sciences. New York, Academic Press, 1988Google Scholar
14.. Hedges LV: Estimation of effect size from a series of independent experiments. Psychol Bull 1982; 97:490-499Crossref, Google Scholar
15.. Fleiss JL: Statistical Methods for Rates and Proportions, 2nd ed. New York, John Wiley & Sons, 1981Google Scholar



