Depression and Self-Reported Functional Status in Older Primary Care Patients
Abstract
OBJECTIVE: The authors’ goal was to examine whether depression is associated with overreporting of functional disability. METHOD: The subjects were 304 patients 60 years old or older who were recruited from primary care settings. Measures included examiner ratings of depression diagnosis and medical burden and self-reported and examiner-rated functional assessments. Multiple regression techniques were used to determine the independent association of depression with self-reported function after examiner-rated function was added to the analysis as a covariate. RESULTS: Depression diagnosis was associated with poorer self-reported role functioning, whether the patient attributed the disability to physical or emotional causes. Depression was not independently associated with poorer self-reported physical functioning. CONCLUSIONS: Clinicians and researchers should recognize that depression can confound the self-reporting and attribution of functional disability.
A number of studies have shown that depression is a leading correlate of functional disability in younger and mixed-age adult populations (1–3). Although the greater prevalence of physical disorders in the elderly than in younger adults may lessen the relative contribution of depression to disability (4), several studies have shown that depression is associated with functional disability in older adults (5–7). However, some of these investigations used subject self-report to measure functional status. Interpretation of such results must be tempered by recognition of the potential confound between depression and self-reported disability, since depression may color self-perceptions and lead to overreporting of functional disability (8–10).
To understand this potential confound better, we explored whether depression is independently associated with self-reported functional status after examiner-rated function is added to the analysis as a covariate. We recruited patients from primary care practices because the majority of older patients suffering clinically significant depression do not see mental health professionals but do see their primary care physicians (11, 12). Accordingly, there have been calls to understand later-life depression and its associated morbidity better in primary care settings (13–15).
Method
The subjects in this study were part of a group described previously (16) who were recruited from private internal medicine offices or a family medicine clinic. All patients 60 years old or older who came for treatment at these practices and gave formal verbal informed consent (procedure approved by the University of Rochester Research Subjects Review Board) were eligible to participate. Patients were screened with the Center for Epidemiologic Studies Depression Scale (CES-D Scale) (17). Stratified sampling was used to oversample patients scoring higher than 21 on the CES-D Scale, but the final study group included patients scoring both above and below this cutoff. Subject assessments were based on the Structured Clinical Interview for DSM-III-R (SCID) (18) administered by trained raters. Depression diagnoses based on the SCID were assigned by a consensus conference of investigators and raters.
Study diagnostic groups were defined as follows: no depression, current major depression, and current minor depression. The diagnosis of minor depression was based on the SCID and the criteria in the appendix to DSM-IV; this definition required no previous history of major depression.
Medical illness burden was rated by using the Cumulative Illness Rating Scale (19). Examiner-rated overall functional status was measured with the Instrumental Activities of Daily Living scale and the Physical Self-Maintenance scale (20); the assessment was based on interview with the subject as well as physician-investigator (J.M.L.) review of the primary care chart. The Global Assessment of Functioning from DSM-III-R and the Karnofsky Performance Status Scale (21) were used to provide examiner ratings of disability judged caused by psychiatric and physical illness factors, respectively.
Self-reported functional status was assessed by using subscales of the Medical Outcomes Study 36-item Short-Form Health Survey (22). The 10 items asking patients to rate limitations in their physical activities due to their overall health were summed as one variable, physical functioning. The 36-item Short-Form Health Survey includes role functioning items that ask the subject to make attributions of the origin of disability, e.g., “Have you had any of the following problems…as a result of your physical health” for one set of responses and “…as a result of any emotional problems (such as feeling depressed or anxious)” for a similar but separate item set.
The questions asking respondents to attribute any curtailment in role activities to their physical health (four items) or emotional health (three items) were summed as the variables physical role and emotional role, respectively. All three 36-item Short-Form Health Survey subscales were converted to scaled scores between 0 and 100 as described in the 36-item Short-Form Health Survey manual (23).
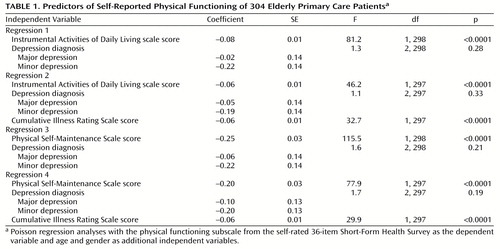
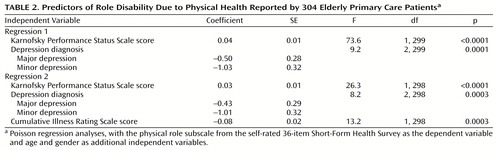
Multiple regression techniques were used to determine whether depression was associated with self-reported functional status (physical functioning) independent of examiner-rated functional level (Instrumental Activities of Daily Living scale or Physical Self-Maintenance scale); age and gender were controlled for. To determine whether any such association was due to medical illness burden comorbid with depression, these regressions were run again with the addition of Cumulative Illness Rating Scale scores as a covariate. Similarly, to explore the relationships between subjective and examiner-rated attributions of role disability, multiple regressions were used to determine the independent associations of depression with physical role and emotional role while Karnofsky Performance Status Scale and Global Assessment of Functioning scores, respectively, were added as covariates (again, with age and gender controlled for) and run again with the addition of Cumulative Illness Rating Scale as a covariate.
Poisson (log linear) regression analysis was used, with an adjustment for extra-Poisson variation, because the dependent variables were discrete with skewed distributions. We used two-tailed p values and defined statistical significance as p<0.01. Parameter estimates (coefficients and standard error) are reported for the independent variables of interest; for the group of patients with a depression diagnosis, the reference group (i.e., coefficient=0) was the nondepressed group.
Results
There were 304 subjects who completed all study measures; 183 (60%) of these subjects were women. Their mean age was 71.3 years (SD=7.6, range=60–94). Their scores on the measures were as follows: Instrumental Activities of Daily Living scale mean=2.3 (SD=4.5, range=0–20), Physical Self-Maintenance scale mean=1.0 (SD=1.8, range=0–15), Global Assessment of Functioning mean=71.1 (SD=15.2, range=15–90), Karnofsky Performance Status Scale mean=79.9 (SD=13.2, range=35–100), Cumulative Illness Rating Scale mean=6.2 (SD=3.0, range=0–16), physical functioning mean=56.8 (SD=29.7, range=0–100), physical role mean=49.4 (SD=41.1, range=0–100), and emotional role mean=69.0 (SD=38.7, range=0–100). Multicollinearity was not a problem in these analyses; all correlations among the predictor variables were less than 0.5.
Table 1 shows the regression analyses examining associations with physical functioning. Depression diagnosis was not significantly associated with physical functioning after we added the Instrumental Activities of Daily Living scale or Physical Self-Maintenance scale scores as covariates, whether or not we also controlled for medical burden as measured by the Cumulative Illness Rating Scale.
Table 2 shows the results examining associations with physical role. Depression diagnosis independently predicted poorer physical role function when covaried for examiner-rated physical disability (Karnofsky Performance Status Scale score), whether or not we controlled for Cumulative Illness Rating Scale scores. Although not shown in Table 2, depression diagnosis was independently associated with poorer emotional role function when covaried for examiner-rated psychiatric disability (measured by the Global Assessment of Functioning), again without and with controlling for Cumulative Illness Rating Scale ratings (p<0.0001 in each of these regressions).
Discussion
These results support the notion that depression may confound the reporting of important aspects of disability. Depression diagnosis was independently associated with poorer self-reported role functioning, whether the subjects attributed this disability to physical or emotional health. However, depression diagnosis was not independently associated with self-reported physical functioning.
We note that our methodology determined the association between depression and self-reported function while examiner-rated function was included in the statistical analysis as a covariate. An alternative approach would be to use precisely the same items to compare self-reported and examiner-rated function directly. Performance-based functional assessments also would add a complementary dimension, although their use raises additional interesting questions regarding the impact of depression on motivational factors that can greatly affect performance measures (24). In addition, longitudinal investigations should determine how fluctuations in depressive states over time affect the interface between depression and self-rated versus examiner-rated function. Such studies ultimately may help clarify depression’s mediating or moderating role in the relationships between medical illnesses and disability. At this time, it is clear that researchers should be mindful of the potential confounding effects of depression on self-reported functional status. Clinicians should use all available informants to aid interpretation of the reports or attributions of disability by depressed elderly patients.
 |
 |
Received Aug. 18, 1999; revisions received Feb. 8, March 31, and Sept. 19, 2000; accepted Oct. 4, 2000. From the Laboratory of Depression and Medical Comorbidity, Program in Geriatrics and Neuropsychiatry, Department of Psychiatry, and the Department of Biostatistics, University of Rochester School of Medicine and Dentistry. Address reprint requests to Dr. Lyness, Department of Psychiatry, University of Rochester Medical Center, 300 Crittenden Blvd., Rochester, NY 14642; [email protected] (e-mail). Supported in part by NIMH grants MH-01113 (Dr. Lyness) and MH-18911 (Dr. Caine). The authors thank T.K. Noel, C. Doane, A. Wisner, A. Gleason, G. Kiernan, H. Stiner, and Z. Yoediono; the patients and staff of the offices of Drs. J. Allen, M. Bergin, M. Berliant, C. Conners, R. Greene, M. Labanowski, R. Maggio, B. Peyser, and R. Pincus; and the Family Medicine Center at Highland Hospital, Rochester, N.Y.
1. Stewart-Brown S, Layte R: Emotional health problems are the most important cause of disability in adults of working age: a study in the four counties of the old Oxford region. J Epidemiol Community Health 1997; 51:672–675Crossref, Medline, Google Scholar
2. Andrews G, Sanderson K, Beard J: Burden of disease: methods of calculating disability from mental disorder. Br J Psychiatry 1998; 173:123–131Crossref, Medline, Google Scholar
3. Wells KB, Stewart A, Hays RD, Burnam MA, Rogers W, Daniels M, Berry S, Greenfield S, Ware J: The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA 1989; 262:914–919Crossref, Medline, Google Scholar
4. Olivares TE, Lyness JM, King DA, Cox C, Doane C, Caine ED: Depressive symptoms, medical illness, and functional status in older primary care patients, in 1998 Annual Meeting New Research Program and Abstracts. Washington, DC, American Psychiatric Association, 1998, pp 218–219Google Scholar
5. Bruce ML, Seeman TE, Merrill SS, Blazer DG: The impact of depressive symptomatology on physical disability: MacArthur Studies of Successful Aging. Am J Public Health 1994; 84:1796–1799Google Scholar
6. Koenig HG, George LK: Depression and physical disability outcomes in depressed medically ill hospitalized older adults. Am J Geriatr Psychiatry 1998; 6:230–247Crossref, Medline, Google Scholar
7. Penninx BW, Guralnik JM, Ferrucci L, Simonsick EM, Deeg DJH, Wallace RB: Depressive symptoms and physical decline in community-dwelling older persons. JAMA 1998; 279:1720–1726Google Scholar
8. Lyness JM, Cox C, Curry J, Conwell Y, King DA, Caine ED: Older age and the underreporting of depressive symptoms. J Am Geriatr Soc 1995; 43:216–221Crossref, Medline, Google Scholar
9. Caine ED: Standing at the mental health/physical health interface: is current caregiver research valid? in Stress Effects on Family Caregivers of Alzheimer’s Patients: Research and Interventions. Edited by Light E, Niederehe G, Lebowitz BD. New York, Springer, 1994, pp 25–37Google Scholar
10. Morgado A, Smith M, Lecrubier Y, Widlocher D: Depressed subjects unwittingly overreport poor social adjustment which they reappraise when recovered. J Nerv Ment Dis 1991; 179:614–619Crossref, Medline, Google Scholar
11. Regier DA, Farmer ME, Rae DS, Myers JK, Kramer M, Robins LN, George LK, Karno M, Locke BZ: One-month prevalence of mental disorders in the United States and sociodemographic characteristics: the Epidemiologic Catchment Area study. Acta Psychiatr Scand 1993; 88:35–47Crossref, Medline, Google Scholar
12. Shepherd M, Wilkinson G: Primary care as the middle ground for psychiatric epidemiology. Psychol Med 1988; 18:263–267Crossref, Medline, Google Scholar
13. Alexopoulos GS: Geriatric depression in primary care. Int J Geriatr Psychiatry 1996; 11:397–400Crossref, Google Scholar
14. Gallo JJ, Rabins PV, Iliffe S: The “research magnificent” in late life: psychiatric epidemiology and the primary health care of older adults. Int J Psychiatry Med 1997; 27:185–204Crossref, Medline, Google Scholar
15. Oxman TE: New paradigms for understanding the identification and treatment of depression in primary care. Gen Hosp Psychiatry 1997; 19:79–81Crossref, Medline, Google Scholar
16. Lyness JM, Caine ED, King DA, Cox C, Yoediono Z: Psychiatric disorders in older primary care patients. J Gen Intern Med 1999; 14:249–254Crossref, Medline, Google Scholar
17. Radloff LS: The CES-D Scale: a self-report depression scale for research in the general population. J Applied Psychol Measurement 1977; 1:385–401Crossref, Google Scholar
18. Spitzer RL, Williams JBW, Gibbon M: Structured Clinical Interview for DSM-III-R (SCID). New York, New York State Psychiatric Institute, Biometrics Research, 1986Google Scholar
19. Linn BS, Linn MW, Gurel L: Cumulative Illness Rating Scale. J Am Geriatr Soc 1968; 16:622–626Crossref, Medline, Google Scholar
20. Lawton MP, Brody EM: Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969; 9:179–186Crossref, Medline, Google Scholar
21. Karnofsky DA, Burchenal JH: The clinical evaluation of chemotherapeutic agents in cancer, in Evaluation of Chemotherapeutic Agents. Edited by MacLeod CM. New York, Columbia, 1949, pp 191–205Google Scholar
22. Ware JE Jr, Sherbourne CD: The MOS 36-Item Short-Form Health Survey (SF-36), I: conceptual framework and item selection. Med Care 1992; 30:473–483Crossref, Medline, Google Scholar
23. Ware JE Jr, Snow KK, Kosinski M, Gandek B: SF-36 Health Survey Manual and Interpretation Guide. Boston, the Health Institute, 1992Google Scholar
24. Bruce ML: The association between depression and disability. Am J Geriatr Psychiatry 1999; 7:8–11Crossref, Medline, Google Scholar



