From Asylum to Hospital to Psychiatric Health Care System
In the 18th century, patients with mental illness were most often hidden and housed in jails, almshouses, and private homes. Dedicated settings, when they existed, provided little care and few activities and frequently used physical coercion, including chains, to restrain the actions of patients. The advancement of the theory of “moral treatment/management,” notably by Philippe Pinel at the Bicetre in Paris in 1792 and William Tuke at the York Retreat in England in 1796, led to the concepts of a compassionate staff, limiting restraint as much as possible, and providing occupations and diversions for the patients in a country environment as being thought conducive to health. With this new theory, the construction and maintenance of psychiatric care institutions began to play an increasingly important role in the treatment of the mentally ill.
Against this backdrop in February 1811, the Asylum was founded as a division of the Massachusetts General Hospital and as the first psychiatric hospital in New England. McLean Asylum , named for its largest early benefactor, accepted its first patients in 1818. It was situated for 77 years on Pleasant Hill in a section of Charlestown in quarters built around the mansion and grounds designed by Charles Bulfinch for Boston merchant Joseph Barrell. This former country estate, a beautiful and quiet retreat, was well suited to then-current precepts for treatment of the mentally ill.
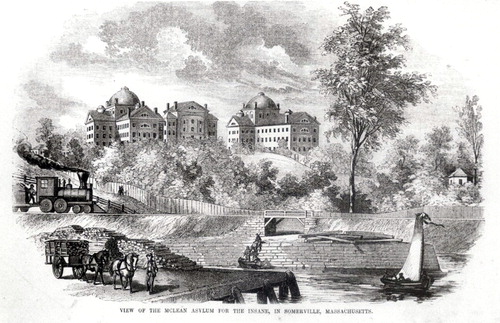
With the steady expansion of railroads through and around the property and with industrialization after the Civil War polluting the adjacent river, the pastoral and pleasant landscape of the Asylum became compromised. After site selection, assisted by famed landscape architect Frederick Law Olmsted in the early 1870s, 107 acres on Wellington Hill in Waverley, just outside of Cambridge, were purchased. The complex was designed for an era in which the mentally ill were usually hospitalized for long periods of time. It was a specialized world for its patients, a largely autonomous system, with its own steam, water, and electrical supplies, livestock farm, and fruit orchards. It functioned as a therapeutic community with physicians, nurses, and plant and operations staff living on the grounds. The importance of the institution’s physical facilities, the dominant role of the superintendent in the delivery of care and hospital construction, and the evolution of the “moral treatment” philosophy in the therapeutic physician-patient relationship were symbolized in the name change from “asylum” to “hospital” in 1892.
Throughout the 20th century, more land was purchased or received by gift, and more buildings were constructed to treat more patients. Six single-patient cottages were built, providing for patients of wealth, which added to the noninstitutional, retreat-like environment of the hospital. The increase in the number and diversity of programs, patients, and staff in the 1960s to the present day, the need to provide upgraded inpatient and medical facilities, and the growth of scientific investigation led to additional buildings, such as a large modern inpatient building, a new library/cafeteria, and a neuroimaging center, as well as several significant expansions of the research laboratories.
In the 1990s, McLean Hospital and similar psychiatric health care facilities were strongly affected by restrictions imposed by both the rise of managed care and limitations in Medicare and Medicaid reimbursement. The negative impact of these changes led some venerable, dedicated psychiatric institutions to close.
Today the goals of inpatient care have shifted to acute crisis intervention. With shorter stays, the number of inpatient buildings has been reduced, even as more patients than ever before are treated. Residential and off-site care have increased. Ironically, however, institutional and rehabilitative care in the United States are again less than that needed by the psychiatrically ill, and many patients are once more homeless or housed and treated in penal facilities. A willingness by modern society to provide and support appropriate care, similar to the commitment of the citizens of the new republic in 1811, would be more humane. Making a full spectrum of care available to more of those with psychiatric illness might even reduce disability, relieve the penal system of an expensive burden, and thereby be more affordable overall. Such an outcome, like the original plan for McLean, could be both economic and therapeutically wise.



