Comparison of Bifrontal and Bitemporal ECT for Major Depression
Abstract
OBJECTIVE: The authors compared the clinical and cognitive effects of bifrontal electrode placement with standard bitemporal electrode placement in the treatment of patients with major depression. METHOD: Forty-eight patients with unipolar or bipolar depression were treated with a course of bifrontal or bitemporal ECT. The Hamilton Rating Scale for Depression and the standardized Mini-Mental State were administered at baseline and repeated during the course of treatment. RESULTS: Forty-seven of the 48 patients who completed the course of treatment met remission criteria by the 12th treatment. There were no differences between the patients given bifrontal ECT and those given bitemporal ECT in the number of treatments required to reach remission criteria. The standardized Mini-Mental State scores of the patients given bitemporal ECT worsened more after treatment than did those of the patients given bifrontal ECT. CONCLUSIONS: Bifrontal electrode placement was as efficacious as bitemporal placement and resulted in less cognitive impairment. A study of the two placements with more cognitive measures is indicated.
Since its introduction in 1938, ECT has been administered as a safe and effective treatment for mental disorders, but public and professional concerns limit its use. The introduction of succinylcholine (to modify convulsive motor effects), continuous oxygenation, and brief-pulse stimuli make ECT more acceptable, but short-term cognitive effects remain a major concern.
Right unilateral ECT causes less cognitive impairment than bitemporal ECT (1, 2) but has less efficacy in treating major depression at threshold stimulus and at 2.5 times threshold (3). Bifrontal ECT has been shown to have equal efficacy to bitemporal ECT with less cognitive impairment, but the literature examining this placement is limited (4–6).
METHOD
The subjects were patients with major depressive disorder, either bipolar or unipolar, with or without psychosis, recruited from the inpatient service of Hillside Hospital. A clinical interview and a chart review confirmed the DSM-IV diagnosis. Patients also met the following inclusion/exclusion criteria: 1) 18 years old or above, 2) score higher than 17 on the 17-item version of the Hamilton Rating Scale for Depression (7) and score higher than 2 on the first item (sad mood), 3) score higher than 24 on the standardized Mini-Mental State (8), 4) no history of any psychotic disorder (other than as part of a mood disorder), cognitive disorder, psychoactive substance abuse or dependence within the previous year, rapid cycling bipolar disorder, or ECT within the past 6 months, and 5) no concomitant psychotropic medication, except up to 3 mg/day of lorazepam as needed for agitation or anxiety. Patients gave written informed consent, and the institutional review board of Hillside Hospital approved the study.
The patients received bifrontal or bitemporal ECT by random assignment. The psychiatrist who administered ECT (S.H.B.) did none of the ratings and was the only investigator who knew the patients’ electrode placements. Anesthetic medications consisted of glycopyrolate, 0.2 mg; methohexital, 1.0 mg/kg; and succinylcholine, 1.0 mg/kg, all given intravenously.
In bitemporal placement, each electrode was placed on the perpendicular line 3 cm above the midpoint of the line joining the external auditory meatus and the outer canthus of the eye. For bifrontal placement, each electrode was placed 5 cm above the outer angle of the orbit on a line parallel to the sagittal plane. Treatment was given with a square-wave, brief-pulse, constant-current device (MECTA SR1).
At the first treatment, the subject’s seizure threshold was established by titration. Subsequent treatments were given at 1.5 times the seizure threshold. If the patient had a missed or abortive seizure, we restimulated at 1.5 times the energy after a 20-second or 60-second interval, respectively.
The patients received treatments three times a week until they met the criteria for remission: 1) Hamilton depression scale score less than 10, 2) first Hamilton depression scale item score less than 3, 3) Clinical Global Impression improvement score less than 3. Patients who had not met these criteria by the 12th treatment were considered treatment failures.
We obtained Hamilton depression scale scores (using the Structured Interview Guide for the Hamilton Depression Rating Scale [7]), CGI scores, and standardized Mini Mental State scores at baseline and 24 hours after each treatment (8).
Baseline comparisons between patients given bitemporal and bifrontal placements were analyzed with chi-square tests for categorical variables and with t tests for continuous variables. A repeated measures analysis of variance was used to determine if there was a difference over time in the patients given bitemporal compared with bifrontal ECT.
RESULTS
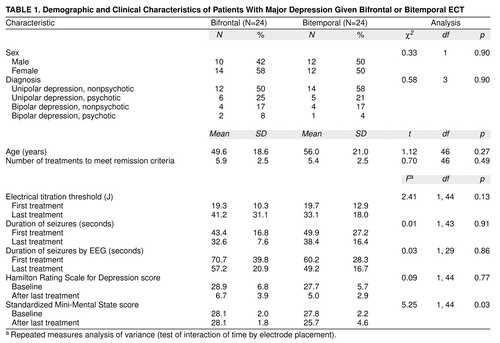
Fifty-eight patients began treatment in the study. Six had their treatments interrupted by medical problems unrelated to ECT, two required antipsychotic medication not allowed by our protocol, and two had to be discharged from the hospital before completing the study. Twenty-four of the remaining 48 patients received bifrontal ECT, and 24 received bitemporal ECT. Forty-seven of the 48 patients who completed the study met remission criteria by the 12th treatment. Patients receiving bifrontal and bitemporal ECT did not differ from each other in mean electrical titration thresholds or seizure durations (table 1).
Patients given bifrontal and bitemporal ECT did not differ in baseline Hamilton depression scale scores (table 1). All 24 patients in the bifrontal group and 23 of the 24 patients in the bitemporal group met the remission criteria before the 12th treatment (table 1>).
The two groups did not differ in baseline standardized Mini-Mental State scores (table 1). The difference between groups in these scores over time, however, was marked by a significant interaction between group and time (table 1): the scores of the group given bitemporal ECT were worse after the last treatment than the scores of the group given bifrontal ECT. Baseline standardized Mini-Mental State scores significantly and negatively correlated with age (r=–0.39, p=0.06). The lower standardized Mini-Mental State scores in the bitemporal group after treatment remained significant when covaried for age (F=4.81, df=1, 43, p=0.03).
DISCUSSION
With the more anterior and medial position described for bifrontal ECT, we avoided direct stimulation of the temporal areas, which mediate human learning and memory, but still delivered an effective bilateral stimulus. SPECT data reported by Sackeim and Prohovnik (9) suggesting that the frontal lobes might be the site where ECT exerts its main therapeutic effects serve to offer a theoretical explanation for the efficacy of the bifrontal placement.
Both placements proved conducive to effective treatment: 47 of the 48 patients responded to treatment. The mean number of treatments required to reach the study endpoint and the electrical and seizure variables were almost identical for both groups (table 1), but the group given bitemporal ECT showed statistically significant worsening in their standardized Mini-Mental State scores (p=0.03). This drop of 2.1 in the standardized Mini-Mental State score, although small, is approximately a full standard deviation and is clinically significant.
Another possible advantage of the bifrontal over the bitemporal placement is that the treatments might cause fewer dental injuries because the electrodes are farther away from the masseter muscles.
We found bifrontal electrode placement to be as effective as bitemporal electrode placement and to have fewer cognitive effects. Although right unilateral electrode placement also yields fewer cognitive effects than bilateral placement, the treatment needs to be administered at 2.5 to 5 times threshold to achieve acceptable efficacy (6). Thus, dose titration is always required to ensure the likelihood of acceptable results and often requires doses in excess of those available with standard ECT devices.
Received Dec. 7, 1998; revision received June 21, 1999; accepted July 29, 1999. From the Department of Psychiatry, Hillside Hospital. Address reprints to Dr. Bailine, Department of Psychiatry, Hillside Hospital, 75-59 263rd St., Glen Oaks, NY 11004. The authors thank Max Fink, M.D., for editorial assistance in the preparation of this article.
 |
1. Sackeim HA, Portnoy S, Neeley P, Steif BL, Decina P, Malitz S: Cognitive consequences of low-dosage electroconvulsive therapy. Ann NY Acad Sci 1986; 462:326–340Crossref, Medline, Google Scholar
2. Weiner RD, Rogers HJ, Davidson JR, Squire LR: Effects of stimulus parameters on cognitive side effects. Ann NY Acad Sci 1986; 462:315–325Crossref, Medline, Google Scholar
3. Sackeim HA, Prudic J, Devanand DP, Kiersky JE, Fitzsimons L, Moody BJ, McElhiney MC, Coleman EA, Settembrino JM: Effects of stimulus intensity and electrode placement on the efficacy and cognitive effects of electroconvulsive therapy. N Engl J Med 1993; 328:839–846Crossref, Medline, Google Scholar
4. Abrams R, Taylor MA: Anterior bifrontal ECT: a clinical trial. Br J Psychiatry 1973; 122:587–590Crossref, Medline, Google Scholar
5. Lawson JS, Inglis J, Delva NJ, Rodenburg M, Waldron JJ, Letemendia FJJ: Electrode placement in ECT: cognitive effects. Psychol Med 1990; 20:335–344Crossref, Medline, Google Scholar
6. Letemendia FJJ, Delva NJ, Rodenburg M, Lawson JS, Inglis J, Waldron JJ, Lywood DW: Therapeutic advantage of bifrontal electrode placement in ECT. Psychol Med 1993; 23:349–360Crossref, Medline, Google Scholar
7. Williams JB: A structured interview guide for the Hamilton Depression Rating Scale. Arch Gen Psychiatry 1988; 45:742–747Crossref, Medline, Google Scholar
8. Folstein MF, Folstein SE, McHugh PR: “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12:189–198Crossref, Medline, Google Scholar
9. Sackeim H, Prohovnik I: Brain imaging studies in depressive disorders, in Biology of Depressive Disorders. Edited by Mann JJ, Kupfer D. New York, Plenum, 1993, pp 205–258Google Scholar



