Neuropsychological Study of Frontal Lobe Function in Psychotropic-Naive Children With Obsessive-Compulsive Disorder
Abstract
OBJECTIVE: The authors’ goal was to evaluate cognition in children with obsessive-compulsive disorder (OCD) early in their illness. METHOD: They administered neuropsychological tests to 21 pediatric patients with OCD and 21 healthy children matched for age, sex, socioeconomic status, and intelligence. The children with OCD were not depressed, and none had ever received psychotropic medication. The neuropsychological tests were used to assess the relationship between psychiatric symptoms and cognitive function. RESULTS: The children with OCD performed as well as the healthy children on the neuropsychological tests. Psychiatric symptoms and cognitive performance were not related. CONCLUSIONS: Nondepressed children with recently diagnosed OCD who had never received psychotropic medication demonstrated no cognitive impairment according to their performance on neuropsychological tests. The authors conclude that OCD symptoms may not interfere with cognitive abilities early in the illness.
Obsessive-compulsive disorder (OCD) usually emerges during childhood and is characterized by repetitive, ritualistic behaviors and thoughts (1). Neuroimaging studies suggest that the basal ganglia and ventral prefrontal cortex are most frequently implicated in OCD (2). If brain dysfunction underlies OCD, decrements on neuropsychological tests should be found. Adult studies support this view: deficits have been found on measures of visuospatial integration (3), reasoning (3), memory (4), and motor coordination (4) in adults with OCD.
Investigations of cognitive function in children with OCD are limited. An early neuropsychological study of adolescents with OCD (5) found differences on tests of learning and on measures sensitive to frontal and parietal lobe lesions. Therefore, children with OCD may manifest visuospatial and problem-solving deficits similar to those of adults, but the results may be confounded by length of illness or disease-related variables. Because psychotropic medications may also influence neuropsychological function (6), in this study we evaluated nondepressed children with OCD early in their illness, when none had ever received psychotropic medication.
METHOD
Twenty-one children with OCD were matched with 21 healthy comparison subjects for age, sex, socioeconomic status, and intelligence. After the study was described to the subjects and their parents, written informed consent was obtained. Psychiatric interviews and reviews of diagnostic information (the Schedule for Affective Disorders and Schizophrenia [7] was used) confirmed that all patients met criteria for OCD.
Exclusion criteria for the patients included lifetime history of psychiatric diagnoses other than OCD, substance abuse or dependence, neurological disorders, head injury, chronic medical illness, mental retardation, and developmental disorders. None of the patients had experienced a depressive episode within 4 months of the study. Seven of the patients with OCD reported OCD in either first- or second-degree relatives. The children in the comparison group had no personal history of affective disorder or psychosis and none in their first-degree relatives.
Psychiatric instruments, described elsewhere (8), included the Yale-Brown Obsessive Compulsive Scale—Revised, Leyton Obsessional Scale, Beck Anxiety Inventory, Hamilton Anxiety Rating Scale, Children’s Depression Inventory, and Hamilton Depression Rating Scale.
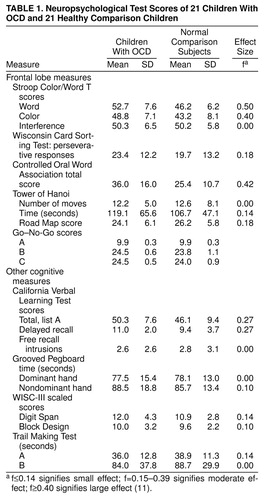
Test selection was based on the frontal lobe literature (9); the tests have been described in Lezak (10) and are listed in table 1.
We used paired t tests or chi-square tests to assess demographic and clinical group differences and analysis of variance (ANOVA) to examine cognitive group and sex effects. Wilcoxon matched pairs signed-ranks tests were used to evaluate Go–No-Go scores, and correlation coefficients were used to evaluate any association between neuropsychological results and age at onset, illness duration, and psychiatric symptoms. Two-tailed alpha equaled 0.05; analyses were completed by using SPSS (12).
RESULTS
The two groups of children did not differ in age (OCD group mean=12.3 years, SD=2.9; comparison group mean=12.2, SD=2.9), sex (OCD group was 57% male; comparison group was 57% male), socioeconomic status (OCD group mean=2.6, SD=0.9; comparison group mean=2.1, SD=0.07), IQ estimated by WISC-III Vocabulary (OCD group mean score=12.0, SD=3.1; comparison group mean score=11.2, SD=2.7), or handedness (OCD group was 8% right-handed and 62% mixed; comparison group was also 8% right-handed and 62% mixed).
Table 1 presents the mean scores of the two groups on the tests of cognitive function. Children with OCD performed better on Go–No-Go B (tap twice if one tap; tap once if two taps) (Wilcoxon T=10.50, N=16, p=0.04). ANOVA indicated a group main effect on three comparisons, but no effect of sex. Children with OCD performed better on the controlled oral word association task (F=6.57, df=1, 38, p=0.01) and had better Stroop word reading (F=9.32, df=1, 38, p=0.004) and color naming (F=6.18, df=1, 38, p=0.02) scores. After a Bonferroni procedure (13), the results for the controlled oral word association task and Stroop word reading remained significant. table 1 shows the effect sizes (11) for the analyses.
The neuropsychological test results were not correlated with either age at onset or duration of illness. The mean age at onset of OCD was 8.9 years (SD=4.5), and the mean duration of illness was 3.9 years (SD=3.9). Children with OCD had higher Yale-Brown Obsessive Compulsive Scale and Leyton Obsessional Scale scores and higher scores on measures of anxiety (Beck Anxiety Inventory, Hamilton anxiety scale) and depression (Children’s Depression Inventory, Hamilton depression scale). There was no relationship between psychiatric symptoms and cognitive function. Five of 152 correlations were significant (not more than would be expected due to experiment-wise error).
DISCUSSION
Nondepressed children who were recently diagnosed as having OCD and who had never received psychotropic medication did not demonstrate cognitive impairment when compared with matched healthy children. We found no evidence that childhood-onset OCD was associated with marked central nervous system dysfunction. The lack of association between psychiatric symptoms and test scores suggests that OCD may not interfere with cognition early in the illness.
Several factors could explain our null results. First, although the measures requiring defined responses were timed, the unstructured reasoning tests were not. Research with adult subjects (14) suggests that OCD symptoms influence problem-solving efficiency rather than problem-solving accuracy. Second, neuropsychological tests may not detect disruption of frontostriatal circuitry. We found abnormal basal ganglia volumes (8) and ventral prefrontal cortical volumes with an abnormality in the maturation of ventral prefrontal cortex (15) in similar youngsters with OCD. A selective oculomotor response suppression deficit, associated with symptom severity but not neuropsychological results (16), suggests that tests developed to assess clinically significant impairment (10) may be insensitive to subtle brain dysfunction. Third, current findings suggest that even tests with putative sensitivity to frontal lobe dysfunction may not detect subtle changes in children. Finally, limited power might account for our null results. table 1 shows that most effect sizes are small or moderate. Nevertheless, on the three cognitive tests that showed a large effect size, children with OCD performed better than the comparison group. A similar trend is seen for those variables showing a moderate effect size.
These results suggest that children with OCD do not exhibit clinically significant cognitive deficits early in the illness. Disturbance of cognitive function may become significant over time.
Presented in part at the 43rd annual meeting of the American Academy of Child and Adolescent Psychiatry, Philadelphia, Oct. 22–27, 1996. Received July 16, 1998; revision received Sept. 16, 1998; accepted Oct. 26, 1998. From the Department of Psychiatry, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine; the Departments of Psychiatry and Behavioral Neurosciences and Pediatrics, Wayne State University School of Medicine, Detroit; and Children’s Hospital of Pittsburgh. Address reprint requests to Dr. Beers, Western Psychiatric Institute and Clinic, 3811 O’Hara St., Pittsburgh, PA 15213; beerssr@MSX. upmc.edu (e-mail). Supported in part by NIMH grant MH-01372 (Dr. Rosenberg). The authors thank Dr. Neal Ryan for referring the healthy children and adolescents who participated in this study.
 |
1. Hanna GL: Demographic and clinical features of obsessive-compulsive disorders in children and adolescents. J Am Acad Child Adolesc Psychiatry 1995; 34:19–27Crossref, Medline, Google Scholar
2. Luxenberg JS, Swedo SE, Flament MF, Friedland RP, Rapoport J, Rapoport SI: Neuroanatomical abnormalities in obsessive-compulsive disorder detected with quantitative X-ray computed tomography. Am J Psychiatry 1988; 145:1089–1093Google Scholar
3. Head D, Bolton D, Hymas N: Deficit in cognitive shifting ability in patients with obsessive-compulsive disorder. Biol Psychiatry 1989; 25:929–937Crossref, Medline, Google Scholar
4. Hollander E, Schiffman E, Cohen B, Rivera-Stein MA, Rosen W, Gorman JM, Fyer AJ, Papp L, Liebowitz MR: Signs of central nervous system dysfunction in obsessive-compulsive disorder. Arch Gen Psychiatry 1990; 47:27–32Crossref, Medline, Google Scholar
5. Behar D, Rapoport JL, Berg CJ, Denckla MB, Mann L, Cox C, Fedio P, Zahn T, Wolfman MG: Computerized tomography and neuropsychological test measures in adolescents with obsessive-compulsive disorder. Am J Psychiatry 1984; 141:363–369Link, Google Scholar
6. Edwards E, Harkins K, Wright G, Menn F: Effects of bilateral adrenalectomy on the induction of learned helplessness. Behav Neuropsychopharmacol 1990; 3:109–114Medline, Google Scholar
7. Chambers WJ, Puig-Antich J, Hirsch M: The assessment of affective disorders in children and adolescents by semi-structured interview. Arch Gen Psychiatry 1985; 42:696–702Crossref, Medline, Google Scholar
8. Rosenberg DR, Keshavan MS, O’Hearn KM, Dick EL, Bagwell WW, Seymour AB, Montrose DM, Pierri JN, Birmaher B: Fronto-striatal morphology in treatment-naive pediatric obsessive compulsive disorder. Arch Gen Psychiatry 1997; 54:831–838Crossref, Medline, Google Scholar
9. Welsh MC, Pennington BF: Assessing frontal lobe functioning in children. Dev Neuropsychol 1988; 4:199–230Crossref, Google Scholar
10. Lezak MD: Neuropsychological Assessment, 3rd ed. New York, Oxford University Press, 1995Google Scholar
11. Cohen J: Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NY, Lawrence Erlbaum Associates, 1988Google Scholar
12. SPSS Base 7.5 for Windows. Chicago, SPSS, 1997Google Scholar
13. Keppel G: Design and Analysis, 3rd ed. Englewood Cliffs, NJ, Prentice-Hall, 1991Google Scholar
14. Gross-Isseroff R, Sasson Y, Voet H, Hendler T, Luca-Haimovici K, Kandel-Sussman H, Zohar J: Alternation learning in obsessive-compulsive disorder. Biol Psychiatry 1996; 39:733–738Crossref, Medline, Google Scholar
15. Rosenberg DR, Keshavan MS: Toward a neurodevelopmental model of obsessive compulsive disorder. Biol Psychiatry 1998; 43:623–640Crossref, Medline, Google Scholar
16. Rosenberg DR, Averbach D, O’Hearn K, Seymour A, Birmaher B, Sweeney JA: Response inhibition abnormalities in pediatric obsessive compulsive disorder. Arch Gen Psychiatry 1997; 54:831–838Crossref, Medline, Google Scholar



