Dimensional Approach to Delusions: Comparison Across Types and Diagnoses
Abstract
OBJECTIVE: A dimensional approach to the characterization of delusions was used to examine the use of non-content-related descriptors of delusions in revealing differences across diagnostic categories and delusion types. METHOD: Interviews with 1,136 acutely hospitalized psychiatric patients identified subjects as definitely or possibly delusional on the basis of screening questions derived from the Diagnostic Interview Schedule. Subjects with delusions were given the MacArthur-Maudsley Delusions Assessment Schedule, which generates scores on six dimensions of delusions. Delusions were classified by type, and diagnoses were assigned by using the DSM-III-R checklist. RESULTS: A total of 328 subjects (29%) were rated as definitely or possibly delusional. Their ratings on dimensions of the MacArthur-Maudsley Delusions Assessment Schedule were significantly but modestly intercorrelated. Subjects with schizophrenia generally had more intense delusions than those in other diagnostic categories. Grandiose and religious delusions were held with the greatest conviction, whereas persecutory delusions were marked by strong negative affect and a propensity to act. Factor analysis of the dimensions revealed a consistent two-factor solution—“intensity and scope” and “affect and action”—regardless of the diagnosis or delusion type. CONCLUSIONS: The stability of the dimensional structure of delusions across diagnoses and delusion types suggests that even seemingly diverse delusions are more like than unlike each other; this is consistent with common etiologic mechanisms. The utility of a dimensional approach is indicated, in addition, by the ability to characterize delusions of different types and diagnoses so as to highlight therapeutic and other implications.
Delusions are the quintessential symptoms of psychotic disorders. Systematic study of the phenomenology of delusions, however, is a relatively recent enterprise, and many fundamental questions remain unanswered. At the most basic level, it is unclear whether delusions, with their manifold presentations, represent a unitary phenomenon—perhaps with a common psychopathologic or neurophysiologic basis—or a cluster of discrete phenomena with superficial similarities (1, 2). Although definite resolution of this question awaits advances in the understanding of brain function and dysfunction, suggestive evidence might be derived from close analysis of the nature of delusional symptoms.
The study of delusions has been dominated to date by a focus on content-related aspects of their presentation; repeated attempts have been made to associate different content types of delusions (e.g., persecutory, grandiose) with different disorders. When these attempts are successful, they suggest the heterogeneity of psychopathological causation across content types. Probably the most durable findings have suggested that bizarre delusions, especially of the Schneiderian type (3), are most commonly found in schizophrenia, and mood-congruent delusions are most often present in affective disorders (4). But these conclusions have not gone unchallenged (5, 6); even when they are supported, violations of these rules are sufficiently common that delusional content has little power to discriminate among diagnostic groups (4).
A newer and promising approach to exploring the commonality or diversity of delusions may be to focus on their primarily non-content-related characteristics. Strauss (7) appears to have been the first to point out that delusions can be characterized along several dimensions that are largely independent of their content; he proposed the dimensions of conviction, preoccupation, external determinants, and implausibility (the last is actually content-related). His idea has been elaborated and operationalized by a number of investigators who have focused on a wide range of delusional characteristics (4, 8–16). As a group, these studies suggest that many of the proposed dimensions can be measured reliably and appear to constitute independent constructs. Few efforts have been made, however, to use the dimensional approach to explore the unitary or diverse nature of delusions by comparing their characteristics across diagnostic categories, and none has attempted to compare them across content types.
Of the existing studies, Harrow et al. (11) found no significant differences on three dimensions (conviction, perspective, and emotional commitment) across diagnostic groups, but the number of subjects was quite small (N=34). Jorgensen and Jensen (12), with a sample of 88 delusional subjects, showed generally similar patterns across diagnostic groups on five dimensions (conviction, extension, systematization, probability, and pressure) but did not subject their findings to tests of significance. It is difficult to draw any firm conclusions from these data regarding the phenomenological heterogeneity of delusions.
In this article, we take a dimensional approach to the analysis of delusions in a large and diverse group of acutely hospitalized psychiatric patients. In particular, we explore the utility of examining non-content-related descriptors of delusions to reveal differences across diagnostic categories and delusion types. We consider the implications of our findings for the general utility of a dimensional approach to delusions and for theories of the common or diverse etiology of delusional symptoms.
METHOD
Data presented in this article are drawn from a prospective multisite study of violence among persons with mental disorders—the MacArthur Violence Risk Assessment Study. The methods of the larger study are described in detail elsewhere (17). In brief, soon after hospitalization at one of the three study sites (Western Missouri Mental Health Center, Kansas City; Western Psychiatric Institute and Clinic, Pittsburgh; and Worcester State Hospital and the University of Massachusetts Medical Center, Worcester), the patients were asked for written informed consent to participate in the study. Those approached were selected randomly from all patients admitted to these facilities, within the constraints of a stratified sampling scheme designed to equalize the proportion of subjects recruited at each site by age, race, and gender. Of the 1,695 patients approached, 1,203 (71%) agreed to participate, and 1,136 completed the baseline interview a mean of 7 days after admission. Eligibility was limited to patients age 18 to 40 who were white, African American, or Hispanic. Patients with eligible primary diagnoses were grouped into the following categories: schizophrenia (including schizophreniform and schizoaffective disorders), depression (including major depression and dysthymia), bipolar disorder (including cyclothymic disorder), other psychotic disorders (including delusional disorder and brief reactive psychosis), alcohol or drug abuse or dependence, or personality disorder.
During the hospital admission, study clinicians (one Ph.D. and two with master’s degrees) used the DSM-III-R checklist (18, 19), a semistructured interview, to establish subjects’ diagnoses and, following the criteria in that instrument, to determine their primary diagnosis—i.e., the diagnosis of greatest immediate clinical significance. When multiple diagnoses were present, the primary diagnosis was almost always (in 84.5% of cases) the diagnosis judged most impairing. Interviewers underwent 3 days of intensive training in the use of the study instruments, including mock interviews and patient interviews supervised by experienced psychiatrists (P.S.A. and L.H.R.). Interrater reliability for the primary diagnoses was calculated by examining the ratings of the three study clinicians on 22 videotaped diagnostic interviews; 12 of the interviews were rated by all three clinicians, and 10 were rated by two of the clinicians. The resulting 46 clinician pairs had an overall agreement rate of 83%, which corresponded to a Cohen kappa of 0.59.
To determine whether each subject was delusional, the clinicians asked a series of 17 questions drawn primarily from the Diagnostic Interview Schedule (available from Dr. Appelbaum) (20). The interviewers were trained to apply the DSM-III-R definition of a delusion, and by further structured questioning and a review of the subjects’ medical records, to use their best judgment to determine whether the subjects were definitely or possibly delusional or whether the subjects’ responses reflected reality (e.g., someone in their neighborhood really was trying to harm them) or some other nondelusional motivation (e.g., malingering). In case of doubt, the interviewers were instructed to err on the side of inclusiveness—i.e., to categorize the belief as a delusion. To ensure the consistency of these determinations, the first author (P.S.A.) reviewed all of the screening forms, which contained the subjects’ verbatim descriptions of their beliefs and, when necessary, listened to audiotapes of the interviews. In only one case was the decision made to change the interviewer’s scoring by moving a subject from the delusional to the nondelusional group. All subjects who scored as definitely or possibly delusional were considered to have delusions for the purpose of this study, and interviewers categorized the delusions by using a standard, content-based typology based largely on DSM-III-R.
Delusional subjects were given a substantially modified version of the Maudsley Assessment of Delusions Scale (14), referred to as the MacArthur-Maudsley Delusions Assessment Schedule (available from Dr. Appelbaum). Subjects who had more than one delusion were asked to identify the delusional belief that had the greatest recent impact on their lives so that it could be subject to more detailed examination with the MacArthur-Maudsley Delusions Assessment Schedule. In those rare cases in which the subject was unable to identify such a delusion, the interviewer selected the delusion that appeared to meet the criterion.
The MacArthur-Maudsley Delusions Assessment Schedule generates scores on seven dimensions: conviction, negative affect, action, inaction, preoccupation, pervasiveness, and fluidity. Specific questions are asked about the first four dimensions; the last three are rated on anchored scales on the basis of the interviewers’ global impressions. (Appendix 1 provides descriptions of each dimension.) For the purpose of this article, data are reported for actions within the last 2 months before hospitalization. In addition, interviewers were asked to indicate the delusions being evaluated by content type. This identification and rating process was also done by trained, usually nonclinician, field interviewers in the community for all subjects at five follow-ups over the 1 year following their discharge from the hospital.
The reliability of interviewer scoring of the MacArthur-Maudsley Delusions Assessment Schedule was evaluated by a review of videotapes of five subjects with delusions that were made by each of the three clinicians (a total of 15 interviews). All interviewers (N=19) reviewed the tapes independently and completed the MacArthur-Maudsley Delusions Assessment Schedule. Results from the intraclass correlation coefficients (ICCs) were poor only for the fluidity dimension, which was dropped from subsequent analyses. For all other dimensions of the MacArthur-Maudsley Delusions Assessment Schedule, the ICCs were in the acceptable range (>0.83), except for pervasiveness (ICC=0.46). However, a two-way analysis of variance of rater effect yielded no significant interrater discrepancies for this item, which indicated no consistent pattern in rater bias, and the item was retained. In addition, to ensure reliability in the classification of types of delusions—some of which had not been rated reliably by the interviewers—the first author (P.S.A.) reviewed all MacArthur-Maudsley Delusions Assessment Schedule interview forms and rescored the type of delusion; rescoring of at least one type of delusion (usually adding additional descriptors) occurred in 172 of the 328 cases reported in this article.
RESULTS
Presentation of Delusions
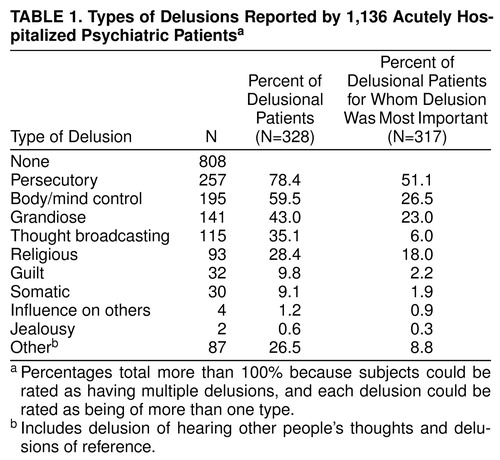
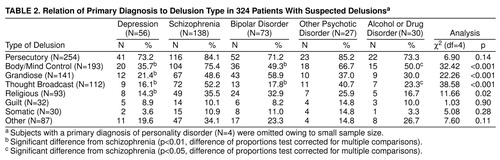
Of the 1,136 subjects screened for delusions, 328 (29%) were rated as possibly (N=43) or definitely (N=285) delusional. Only 55 of the delusional subjects (16.8%) were scored as delusional on just one screening question. The median number of delusional responses was four. Similarly, 75.9% (N=249) of the delusional subjects were rated as having delusions that fell into more than one category in the content-based typology; the median was three. table 1 shows that persecutory delusions and delusions of body/mind control predominated, and when present, persecutory and religious delusions were proportionately most likely to be chosen as having the greatest impact on subjects’ lives. The prevalence of delusions in this sample was highest in patients with schizophrenia (71%, N=138 of 194) and lowest in patients with depression (12%, N=56 of 467) and alcohol or drug abuse (11%, N=30 of 273). Comorbidity with alcohol or drug abuse did not affect the prevalence of delusions in the other diagnostic categories. table 2 illustrates the distribution of delusion types by diagnostic category. Of note is the very high prevalence of persecutory delusions across diagnoses and the disproportionate presence of persecutory, body/mind control, thought broadcasting, and religious delusions in schizophrenia compared with depression or bipolar disorder. As expected, grandiose delusions were less prevalent in depression. Delusions in alcohol and drug abusers had no content-related distinguishing features.
Dimensions of Delusions
With the exception of the relationship between conviction and action or inaction, all of the MacArthur-Maudsley Delusions Assessment Schedule dimensions were significantly correlated with each other (p<0.01) but generally only to a modest extent (range of Pearson correlation coefficient, r=0.15–0.53; p values ranged from <0.05 to <0.001).
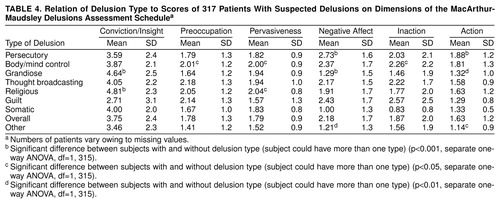
When we compared dimensional scores by diagnosis in table 1, significant differences were found for conviction/insight, preoccupation, and pervasiveness; subjects with schizophrenia scored higher on all three dimensions. When subjected to post hoc multiple-comparisons Bonferroni tests, subjects with schizophrenia were likely to score significantly higher on pervasiveness than subjects with bipolar disorder (mean difference=0.44, SD=0.14, p=0.01) and subjects with alcohol or drug disorder (mean difference=0.83, SD=0.19, p=0.001) as a primary diagnosis. A similar analysis for type of delusion is shown in table 4. Of particular note are the significantly higher scores on the conviction dimension for grandiose and religious delusions and the combination of higher scores on inaction and action for persecutory delusions. Somewhat surprising, perhaps, are the significantly lower scores on action in subjects with grandiose delusions.
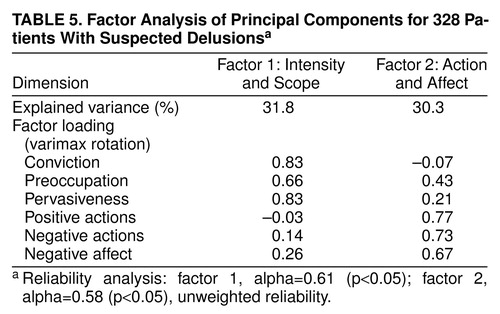
A rotated component factor analysis, displayed in table 5, revealed two factors: one we labeled “intensity and scope” (consisting of conviction, pervasiveness, and preoccupation); the second we labeled “action and affect” (consisting of action, inaction, and negative affect). Each factor accounted for approximately 30% of the variance. The results of additional factor analyses were essentially identical for all diagnostic groups when completed for each separately, except for the heterogeneous category of “other psychoses.” The factor results also held across all types of delusions. These results suggest a strong underlying similarity in the dimensional structure, regardless of diagnosis or delusion type.
DISCUSSION
A dimensional approach to the characterization of delusions in 328 acutely hospitalized psychiatric patients revealed a low to moderate degree of correlation among the dimensions, a finding consistent with previous work (8, 21). There was, however, a strong similarity in the factor structure of the dimensions across diagnoses and types of delusions. “Intensity and scope” and “action and affect” provided a robust two-factor solution for almost all diagnostic and typological categories. This indicates that from the perspective of their non-content-related phenomenology, seemingly diverse delusions are more like than unlike each other. Although similarity in the characteristics of delusions is not determinative of etiologic homogeneity (i.e., disparate neurophysiologic or psychopathologic processes could result in similar symptoms), it is certainly consistent with such a hypothesis.
It is difficult to compare these findings on factor structure to the small number of previous investigations that have taken a dimensional approach, because each research group to date has selected a different set of dimensions to measure. Kendler and colleagues (8), for example, examined five dimensions in 52 subjects—conviction, extension (similar to our concept of pervasiveness), bizarreness, disorganization, and pressure (which resembles preoccupation in this study). They found two factors. The one encompassing conviction, extension, and pressure was called “delusional involvement” and seems similar to our first factor—“intensity and scope.” Their second factor, which consisted of bizarreness, disorganization, and extension, they labeled “delusional construct.” In contrast, Eisen et al. (16), looking at six dimensions in 50 subjects, found that they all loaded onto a single factor; most of the dimensions, however, seemed to relate to our “conviction” dimension (i.e., conviction, perception of others’ views of belief, explanation of differing views, attempt to disprove beliefs, and insight—but not fixity of ideas), making this finding less surprising. By using a broader approach, Garety and Hemsley (9), employing 11 dimensions with 55 subjects, found a four-factor solution: distress, belief-strength, obtrusiveness, and concern. However, the stability of the factor structure demonstrated in our data raises the question of whether “intensity and scope” and “affect and action” may represent fundamental characteristics of delusions. This appears to be worth further investigation with similar methods in other patient samples.
Examination of the absolute dimensional scores suggests that this approach can be helpful in elucidating other properties of delusions as well. Persecutory delusions, for example, had significantly higher scores on action and negative affect, a combination that raises the question of whether persons with these delusions may be more likely to act, perhaps violently, in response to the dysphoric aspects of their symptoms. Wessely and colleagues (13, 22), in fact, by using the original version of the Maudsley Assessment of Delusions Scale, found that persecutory delusions and negative affect were significantly associated with acting on delusions, and Cheung et al. (23) recently extended these findings to violent actions per se. Our findings here may suggest a mechanism for a relationship between delusions and violence (24), particularly for how “threat/control override” delusions, of which persecutory delusions are a component, may predispose a patient to violence (25–27). On the other hand, body/mind control delusions, also a type of threat/control override delusion, revealed no greater propensity in our data for inducing negative affect or for resulting in violence. Indeed, this category of delusions was significantly more likely to lead to abstention from action (“inaction”) than were other types of delusions.
Recent efforts to treat delusions by means of cognitive behavioral therapy may also be informed by these data. One group of investigators (28, 29) has suggested that such efforts are most likely to be successful when patients begin with some inherent doubts about their delusional beliefs. If that proves to be correct, patients with schizophrenia and with grandiose and religious delusions, all of whom scored significantly higher on ratings of conviction, may be least susceptible to cognitive behavioral interventions.
The MacArthur-Maudsley Delusions Assessment Schedule appears to offer a practical means of assessing the dimensions of delusional beliefs. In this study, even with a majority of the interviewers lacking clinical backgrounds, most dimensions were scored reliably; this points to the potential use of the MacArthur-Maudsley Delusions Assessment Schedule in large-scale, community-based studies. The data on dimensional characteristics associated with diagnoses and types of delusions provide substantial reassurance regarding the validity of the resulting scores. Further exploration of the characteristics of the instrument and its relationship to other approaches of assessing delusions is warranted.
Received May 18, 1998; revisions received Nov. 20, 1998, and April 16, 1999; accepted April 30, 1999. From the Department of Psychiatry, University of Massachusetts Medical School; the Policy Research Associates, Inc., Delmar, N.Y.; and Health Sciences, University of Pittsburgh School of Medicine. Address reprint requests to Dr. Appelbaum, Department of Psychiatry, University of Massachusetts Medical School, Worcester, MA 01655; [email protected] (e-mail). Supported by the Research Network on Mental Health and the Law of the John D. and Catherine T. MacArthur Foundation; by NIMH grant MH-49696; and in part by a fellowship from the Center for Advanced Studies in the Behavioral Sciences (to Dr. Appelbaum), funded by the Center’s Foundations Fund for Research in Psychiatry and National Science Foundation grant SBR-9022192. The authors thank their collaborators in the MacArthur Violence Risk Assessment Study: John Monahan, Ph.D., Henry Steadman, Ph.D., Ed Mulvey, Ph.D., Thomas Grisso, Ph.D., and Roumen Vesselinov, M.A.
 |
 |
 |
 |
 |
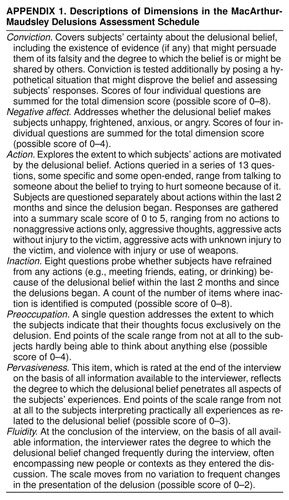 |
APPENDIX 1. Descriptions of Dimensions in the MacArthur-Maudsley Delusions Assessment Schedule
1. Markova IS, Berrios GE: Mental symptoms: are they similar phenomena? Psychopathology 1995; 28:147–157Google Scholar
2. Berrios GE: The History of Mental Symptoms: Descriptive Psychopathology Since the Nineteenth Century. Cambridge, UK, Cambridge University Press, 1996, pp 85–139Google Scholar
3. Schneider K: Clinical Psychopathology. New York, Grune & Stratton, 1959Google Scholar
4. Junginger J, Barker S, Coe D: Mood theme and bizarreness of delusions in schizophrenia and mood psychosis. J Abnorm Psychol 1992; 101:287–292Crossref, Medline, Google Scholar
5. Berner P, Gabriel E, Kronberger ML, Kufferle B, Schanda H, Trappl R: Course and outcome of delusional psychoses. Psychopathology 1984; 17:28–36Crossref, Medline, Google Scholar
6. Pope HG Jr, Lipinski JF Jr: Diagnosis in schizophrenia and manic-depressive illness: a reassessment of the specificity of “schizophrenic” symptoms in the light of current research. Arch Gen Psychiatry 1978; 35:811–828Crossref, Medline, Google Scholar
7. Strauss JS: Hallucinations and delusions as points on continua function. Arch Gen Psychiatry 1969; 21:581–586Crossref, Medline, Google Scholar
8. Kendler KS, Glazer WM, Morgenstern H: Dimensions of delusional experience. Am J Psychiatry 1983; 140:466–469Link, Google Scholar
9. Garety PA, Hemsley DR: Delusions: Investigations Into the Psychology of Delusional Reasoning. Oxford, UK, Oxford University Press, 1994Google Scholar
10. Oltmanns TF: Approaches to the definition and study of delusions, in Delusional Beliefs. Edited by Oltmanns TF, Maher BA. New York, John Wiley & Sons, 1988, pp 3–11Google Scholar
11. Harrow M, Rattenbury F, Stoll F: Schizophrenic delusions: an analysis of their persistence, of related premorbid ideas, and of three major dimensions, in Delusional Beliefs. Edited by Oltmanns TF, Maher BA. New York, John Wiley & Sons, 1988, pp 184–211Google Scholar
12. Jorgensen P, Jensen J: A dimensional approach to severe delusional psychoses. Psychopathology 1990; 23:9–14Crossref, Medline, Google Scholar
13. Buchanan A, Reed A, Wessely S, Garety P, Taylor P, Grubin D, Dunn G: Acting on delusions, II: the phenomenological correlates of acting on delusions. Br J Psychiatry 1993; 163:77–81Crossref, Medline, Google Scholar
14. Taylor PJ, Garety P, Buchanan A, Reed A, Wessely S, Ray K, Dunn G, Grubin D: Delusions and violence, in Violence and Mental Disorder: Developments in Risk Assessment. Edited by Monahan J, Steadman HJ. Chicago, University of Chicago Press, 1994, pp 161–182Google Scholar
15. Oulis PG, Mavreas VG, Mamounas JM, Stefanis CN: Formal clinical characteristics of delusional beliefs. Psychopathology 1996; 29:201–208Crossref, Medline, Google Scholar
16. Eisen JL, Phillips KA, Baer L, Beer DA, Atala KD, Rasmussen SA: The Brown Assessment of Beliefs Scale: reliability and validity. Am J Psychiatry 1998; 155:102–108Link, Google Scholar
17. Steadman HJ, Mulvey EP, Monahan J, Robbins PC, Appelbaum PS, Grisso T, Roth LH, Silver E: Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry 1998; 55:393–401Crossref, Medline, Google Scholar
18. Janca A, Helzer J: DSM-III-R criteria checklist. Diagnostic Interview Schedule Newsletter 1990; 7:17Google Scholar
19. Hudziak JJ, Helzer JE, Wetzel MW, Kessel KB, McGee B, Janca A, Przybeck T: The use of the DSM-III-R Checklist for initial diagnostic assessments. Compr Psychiatry 1993; 34:375–383Crossref, Medline, Google Scholar
20. Robins LN, Helzer JE, Croughan J (eds): National Institute of Mental Health Diagnostic Interview Schedule, version III: PHS Publication ADM-T-42-3. Rockville, Md, NIMH, 1981Google Scholar
21. Brett-Jones J, Garety P, Hemsley D: Measuring delusional experiences: a method and its application. Br J Clin Psychol 1987; 26:257–265Crossref, Medline, Google Scholar
22. Wessely S, Buchanan A, Reed A, Cutting J, Everitt B, Garety P, Taylor PJ: Acting on delusions, I: prevalence. Br J Psychiatry 1993; 163:69–76Crossref, Medline, Google Scholar
23. Cheung P, Schweitzer I, Crowley K, Tuckwell V: Violence in schizophrenia: role of hallucinations and delusions. Schizophr Res 1997; 26:181–190Crossref, Medline, Google Scholar
24. Junginger J, Parks-Levy J, McGuire L: Delusions and symptom-consistent violence. Psychiatr Serv 1998; 49:218–220Link, Google Scholar
25. Link BG, Stueve A: Psychotic symptoms and the violent/illegal behavior of mental patients compared to community controls, in Violence and Mental Disorder: Developments in Risk Assessment. Edited by Monahan J, Steadman HJ. Chicago, University of Chicago Press, 1994, pp 137–159Google Scholar
26. Link BG, Monahan J, Stueve A, Cullen FT: Real in their consequences: a sociological approach to understanding the association between psychotic symptoms and violence. Am Sociol Rev 1999; 64:316–332Crossref, Google Scholar
27. Swanson J, Borum R, Swartz M, Monahan J: Psychotic symptoms and disorders and the risk of violent behavior in the community. Criminal Behavior and Ment Health 1996; 6:317–338Crossref, Google Scholar
28. Chadwick PDJ, Lowe CF: Measurement and modification of delusional beliefs. J Consult Clin Psychol 1990; 58:225–232Crossref, Medline, Google Scholar
29. Chadwick PDJ, Lowe CF: A cognitive approach to measuring and modifying delusions. Behav Res Ther 1994; 32:355–367Crossref, Medline, Google Scholar



