Perceptions of Need and Help Received for Substance Dependence in a National Probability Survey
Most individuals with alcohol or drug use disorders do not seek help or receive treatment for these problems. National surveys suggest that fewer than half of those with past-year psychiatric disorders (including substance use disorders) receive any treatment ( 1 , 2 ). Research from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) indicated that 24% of individuals with alcohol dependence during their lifetime ever received treatment and that only 12% of individuals with past-year alcohol dependence received treatment in that year ( 3 ). Although treatment is generally higher among individuals with drug dependence, it is still far from comprehensive; current estimates suggest that 38% of those with lifetime drug dependence and 31% of those with the disorder in the past year receive treatment within those time frames ( 4 ).
Health services research has identified several factors associated with treatment. Treatment utilization is higher among individuals who have multiple types of substance use problems as well as co-occurring mental disorders ( 5 , 6 , 7 ). In addition to the nature and severity of disorders, the perception of need and the willingness to seek help vary by several sociodemographic characteristics ( 8 ). Unmet need for treatment appears to be highest among the elderly population, persons from racial-ethnic minority groups, those with low incomes, those without insurance, and residents of rural areas ( 1 ).
Furthermore, factors that improve access to care, such as health insurance coverage, employment, and geographic locale, may influence the perceived need for and ability to seek help ( 9 ). Notably, a significant proportion of individuals in the general population who do not meet criteria for a psychiatric disorder nonetheless reported having received treatment in the past year ( 10 ). Thus the perceived need for help and the actual receipt of help for a substance use disorder are not simply a function of meeting diagnostic criteria for a disorder.
The broader health services literature has identified sociodemographic and need-related factors that are associated with health services utilization and barriers that impede access to these services. This study contributed to this body of work by examining individual characteristics that are related not only to the receipt of help but also to the perception of the need for help among individuals with alcohol or drug dependence. We applied the Andersen behavioral model of health services utilization ( 11 , 12 ) to understand the perception of need for help and help seeking among individuals with past-year substance dependence. The model included predisposing characteristics that were fixed characteristics of the individuals; enabling resources that facilitated or impeded health services utilization; and need-related variables that pertained to the number, type, and severity of disorders and associated problems. On the basis of prior research, we hypothesized that the following types of characteristics would contribute to both the perceived need for and the receipt of help for substance dependence: predisposing characteristics, such as sociodemographic characteristics; enabling characteristics, such as health insurance status, marital status, and employment; and need-related characteristics that referred to the severity of the disorder and problems related to substance use. In particular, we hypothesized that a greater number of problems related to substance use would increase both the perception of need and help received for substance dependence.
Methods
Sample
The 2001–2002 NESARC used a representative sample from the United States. The study methodology has been described in detail elsewhere ( 13 ). The target population of the NESARC was the civilian, noninstitutional population of the United States residing in households as well as in group quarters (such as group homes and halfway houses). Face-to-face interviews were conducted with 43,093 respondents. The overall survey response rate was 81%. African Americans, Hispanics, and young adults (ages 18–24 years) were oversampled, with data adjusted for oversampling and household- and person-level nonresponse. The weighted data were then adjusted to represent the U.S. civilian population as of the 2000 census.
The sample for this study (N=1,602) included all individuals in the 2001–2002 NESARC who met criteria for past-year dependence on alcohol or any drug. This sample represented approximately 4.1% of the total (weighted) NESARC general population sample (approximately 8.5 million individuals). All interviewed participants provided voluntary consent for their participation after having received detailed information about the nature of the survey, statistical uses of the survey data, the voluntary aspect of their participation, and the federal laws that protect their confidentiality.
Diagnostic assessment
Diagnosis of past-year dependence on alcohol or drugs was based on the Alcohol Use Disorder and Associated Disabilities Interview Schedule—DSM-IV Version (AUDADIS-IV). The AUDADIS-IV includes an extensive list of symptom questions that separately operationalize DSM-IV criteria for abuse of and dependence on alcohol and ten classes of illicit or prescription drugs (referred to as "medicines" in the interview). Consistent with the DSM-IV, AUDADIS-IV past-year dependence diagnoses require at least three of the seven DSM-IV criteria for dependence to be met during the past year.
The AUDADIS-IV was also used to generate diagnoses of past-year mood disorders, including major depression, dysthymia, mania, and hypomania; past-year anxiety disorders, including panic disorder with and without agoraphobia, social phobia, specific phobia, and generalized anxiety disorder; and personality disorders, including schizoid, paranoid, avoidant, dependent, obsessive-compulsive, histrionic, and antisocial. Mood and anxiety diagnoses in NESARC are consistent with DSM-IV criteria for primary or independent diagnosis, meaning that mental disorders that are substance induced, a result of a general medical condition, or entirely accounted for by bereavement were excluded ( 14 ). Numerous studies conducted with clinical and general population samples have demonstrated good to excellent reliability and validity of the AUDADIS-IV diagnoses ( 13 , 14 , 15 , 16 ).
Variables
Dependent variable. Respondents were asked, "Have you ever gone anywhere or seen anyone for a reason that was related in any way to your drinking or use of medicine or drugs?" Responses included Alcoholics Anonymous or any other type of 12-step meeting; family services or another social service agency; alcohol or drug detoxification program; inpatient ward of a psychiatric or general hospital or community mental health program; outpatient clinic, including outreach programs and day or partial hospital programs; alcohol or drug rehabilitation program, including methadone maintenance; emergency service; halfway house or therapeutic community; crisis center; employee assistance program; clergyman, priest, rabbi, or any type of religious counselor; private physician, psychiatrist, psychologist, social worker, or any other medical or social services professional or agency.
Respondents who indicated that they had sought help from any of the options within the past 12 months were coded as 1, for having received help, on the dependent variable. Those who indicated they had not received help were asked, "Was there ever a time when you thought you should see a doctor, counselor, or other health professional or seek any other help for your drinking or medicine or drug use?" Respondents who indicated yes with reference to the past 12 months were coded as 2, for perceived a need for help but did not receive it. All others were coded as 3, for no perceived need for help and no help received in the past year.
Predictor variables. These variables were selected on the basis of the conceptual model of health services utilization and organized into three groups, as described below.
Predisposing variables referred to fixed characteristics of the individual and included gender, ethnicity (dichotomized into nonwhite and white because of small cell sizes for some of the categories), age, and educational status (categorized into less than high school, high school graduate, and some college or higher).
Enabling variables represented factors that may facilitate or impede help-seeking behavior. These were marital status (categorized into married or living with someone; widowed, separated, or divorced; and never married), household income, place of residence (urban or rural), U.S. region of residence (Northeast, Midwest, South, or West), and health insurance status (yes or no).
Need-related variables pertained to the type, history, and severity of substance dependence and associated problems. These included whether the individual had ever sought help for an alcohol or drug problem prior to the past year and the type of substance dependence (alcohol only, drug only, or alcohol and drug). The average number of years since the onset of dependence was calculated on the basis of earliest age of onset of alcohol or any drug dependence for cases in which there was dependence on more than one type of substance. Mean imputation was used for 56 cases with missing values, with imputation based on both age category and type of substance. A square-root transformation was performed on this variable because of data skewness. Past-year mood or anxiety disorder or lifetime personality disorder were coded as separate dichotomous variables. Having a family member with alcohol or drug problems comprised "natural or blood relatives," including parents, siblings, children, aunts or uncles, or grandparents who had physical, emotional, legal, familial, work, or health problems related to their use of alcohol or drugs.
Problems related to substance use were determined by asking respondents whether they had had problems in the past year stemming from their use of alcohol or drugs with regard to job or school, driving, risk of getting hurt, trouble with family or friends, physical fights, taking care of home or family, or legal issues. Positive responses to each item (responses taken separately for alcohol and drugs) that had occurred in the past year were coded as 1 and summed for an aggregate measure that ranged from 0 to 14 and was entered as a continuous variable in the multivariate models. Current health status was assessed by an item that asked respondents to classify their health as poor, fair, good, very good, or excellent; this variable was dichotomized as good to excellent, coded 1, or fair to poor, coded 0.
Statistical methods
Descriptive statistics were used to compare the predisposing, enabling, and need-related characteristics of individuals who had received help for substance dependence in the past year, those who perceived a need for help but did not receive any, and those who neither perceived a need for nor received help. Next, a multinomial logistic regression model was constructed in which having received help or perceiving a need for help but not receiving it were compared with the referent category of neither perceiving a need for help nor receiving it. Variables from the three domains that were significantly associated with the outcome variable were entered into the multivariate model, with one exception. We dropped the variable indicating treatment received before the past year because it was strongly correlated with the dependent variable and was thus endogenous. In addition, having a family history of alcohol problems and having a family history of drug problems were combined into one variable because they were highly correlated.
Variables were considered statistically significant at p<.05. Odds ratios (ORs) and 95% confidence intervals are reported. Analyses were conducted with SUDAAN, version 9.0, a software program that uses Taylor-series linearization to adjust for NESARC's sample design characteristics ( 17 ). Unweighted sample sizes are reported in the tables; all statistics were weighted.
Results
Bivariate relationships of characteristics and help status
Overall, 14.7% of the weighted sample had received help in the past year, 8.5% perceived a need for help but did not receive it, and 76.8% had no perceived need for help and received no help. There were no significant differences among the three help status groups by gender ( Table 1 ). There were proportionately more nonwhites than whites who perceived a need for help but did not receive it (45%), relative to their proportions in the other help status groups (31% who received help and 27% who did not perceive a need for it). Similarly, there were proportionately more individuals in the youngest age group (18–29 years) who did not perceive a need for help (58%) compared with the other help status groups (33% who received help and 43% who perceived a need for help but did not receive it). In contrast, proportionately more persons in the older age groups (30–44 and 45 and older) had either received help or had perceived a need for help but not received it compared with the proportions in the other help status groups. Proportionately more individuals who had not graduated from high school (25%) or who were high school graduates (38%) perceived a need for help but had not received it, whereas proportionately fewer individuals with some college education were in this category (37%) relative to their proportions in the other help status groups.
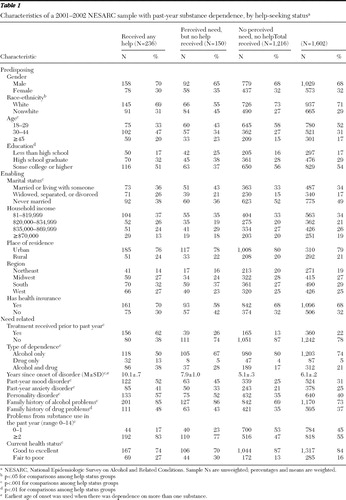 |
Among the enabling characteristics, proportionately more individuals who were widowed, separated, or divorced had received help; proportionately more married individuals had perceived a need for help but had not received it; and proportionately more of those who had never been married had no perceived need for help, relative to their proportions in the other help status groups. There were no significant differences in help status associated with household income, place of residence, or region.
Among the need-related characteristics, a history of having received prior help was strongly associated with receipt of help in the past year. Overall 62% of those who had received help in the past year had a history of help seeking prior to the past year, compared with 26% of those who perceived a need for help but did not receive help and 13% of those who did not perceive a need for help.
Help status was strongly associated with the type of substance dependence. About 80% of those who had no perceived need for help were alcohol dependent, compared with about half of those who had received any help and two-thirds who perceived a need for help but did not receive it. In contrast, a greater proportion of those who had received help were dependent on both alcohol and other substances (38%), compared with 28% of those who perceived a need for help but did not receive it and 17% of those who did not perceive a need for help. Greater proportions of those who had received help or who perceived a need for it also had mood, anxiety, or personality disorders. Greater proportions of those who either had received help or perceived a need for it had a family history of alcohol or drug problems compared with those who had no perceived need for help. Individuals who reported two or more problems in the past year from their substance use were proportionately more likely to have received help (83%) or to have perceived a need for it but not receive it (77%), whereas a greater proportion of those with one or no problems did not perceive a need for treatment and did not receive it (53%) compared with the other help status groups. Individuals who had received help or who perceived a need for it were more likely to describe their health status as fair to poor, rather than as good to excellent, compared with those who had no perceived need for help.
Results from multinomial logistic regression model
With regard to predisposing factors, nonwhites had over twice the odds of whites (OR=2.2) of perceiving a need for help but not receiving it ( Table 2 ). Compared with individuals aged 18–29 years, individuals aged 30–44 years were over three times as likely (OR=3.2) to have received help, and those aged 45 and older were over two times as likely (OR=2.4) to have received help. Educational status was not significantly associated with help status.
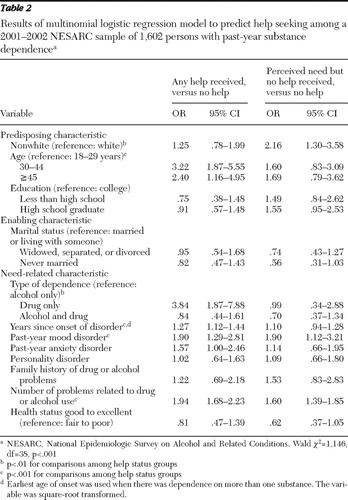 |
After analyses controlled for the other variables in the model, the only enabling characteristic entered into the model, marital status, was not significantly associated with help status.
Several need-related characteristics were significantly associated with help status. Individuals with only drug dependence had almost four times the odds (OR=3.8) of seeking help compared with those with only alcohol dependence. A longer duration since onset of dependence increased the odds of both perceiving a need for help and receiving it in the past year. Similarly, individuals with a past-year mood disorder were approximately twice as likely as those without to receive help as well as to perceive a need for help but not receive it. Having a greater number of problems associated with substance use significantly increased the likelihood of both perceiving a need for help and receiving it. After analyses controlled for the other variables in the model, we found that family history of alcohol or drug problems, perceived health status, past-year anxiety disorder, and personality disorder were not associated with help status.
Discussion
Consistent with other national surveys ( 1 , 2 , 5 , 6 , 7 , 8 , 9 ), this study showed that most individuals with substance dependence did not receive any treatment or services related to these disorders, although individuals who had a co-occurring mood disorder were more likely to receive help. The study extended these prior findings by identifying individual characteristics that were associated with both the perception of need for help and the receipt of help. Both predisposing and need-related variables were associated with help status, but contrary to prior research ( 1 ) and our hypothesis, none of the enabling factors were associated.
Of note is that those who were drug dependent were approximately four times as likely as those who were dependent only on alcohol to receive help. The illegal versus legal status of drugs and alcohol, respectively, may underlie this distinction, where misuse of alcohol is more socially normative and drug dependence is more easily identified as problematic. Further, some have suggested that the low rate of treatment seeking among those with alcohol-related problems stems from the abstinence orientation of most alcohol treatment, which creates a barrier for those who cannot envision total abstinence from alcohol or who do not consider themselves to be alcoholics ( 18 ). Others have suggested that the stigma associated with substance use problems, as well as low levels of motivation and dissatisfaction stemming from prior treatment, are barriers to seeking help ( 19 ).
Several variables that were significantly associated with help status at the bivariate level were not significant in the multivariate analyses; these included marital and educational status, having a family history of alcohol or drug problems, past-year anxiety disorder, personality disorder, and current health status. Although these factors may be associated with the recognition of a need for help, their influence on help seeking may have been mitigated by other factors.
As hypothesized, this study demonstrated that having more problems related to alcohol or other substance use was associated with help status, after analyses controlled for predisposing factors (race-ethnicity, age, and education), enabling factors (marital status), and severity of disorder (co-occurring disorders, duration of dependence, and health status). Because more problems associated with substance use may be indicative of greater severity, this finding was expected. However, the causal direction of this relationship could not be discerned; that is, individuals who had received help may have been better able to identify problems related to their substance use, perhaps because of the help they had received. Nevertheless, the findings suggest that greater awareness of problems stemming from one's substance use may help to leverage treatment participation and other help-seeking behaviors, consistent with the premise of motivational enhancement interventions ( 20 ).
Findings about the relatively low levels of help seeking among those with substance use disorders have prompted a debate regarding the extent to which clinical diagnosis is an accurate indicator of need for treatment. Some have argued that "clinical significance," as indicated by symptom severity, psychological distress, or impairments in functioning, may more accurately represent need for treatment than DSM -based diagnostic categories ( 10 , 21 , 22 ). Moreover, this debate has relevance to criteria that should be used to determine a threshold for "unmet need for treatment," which may be the basis for determining the adequacy of the treatment system in providing treatment to those who "need" it ( 23 ). Our findings on the lower level of problem severity among those who did not receive help suggest that meaningful distinctions can be made between the diagnosis of a substance use disorder and need for care. Clearly, more research is warranted to specify the indicators of need for treatment, apart from reliance solely on diagnostic criteria.
The findings with regard to the effects of race-ethnicity on help status were mixed, as has been shown in other studies ( 24 , 25 ). Although race-ethnicity was not significantly associated with having received help, nonwhites were more likely than whites to perceive a need for help but not receive it. Other research conducted with NESARC showed no difference between African Americans and whites in lifetime help received for alcohol problems, although whites were less likely to receive help for drug problems ( 26 ). Other studies have shown that attitudinal and perceptual factors account for some of the underutilization of mental health services among ethnic minority groups; these may include perceived discrimination, prior negative experiences associated with services utilization, and limited knowledge regarding available treatment and services ( 27 , 28 , 29 , 30 ). Our findings suggest that such factors should be explored to better understand the reasons why individuals from racial-ethnic minority groups who perceive a need for help with substance use problems do not receive it.
Interpretation of the study findings should include consideration of limitations that are inherent in the use of retrospective surveys, in which recall of specific symptoms over time may be inaccurate and influenced by the respondent's current mental and general medical health status ( 31 ). Moreover, substance use and mental disorders were assessed by nonclinical personnel and diagnosed in the absence of evaluations of clinical severity. However, the validity of such data can be enhanced by use of standardized procedures and rigorous staff training and oversight ( 32 ), all of which were implemented in the NESARC study. Moreover, recall error may have been minimized by the discrete time period examined (the past year), rather than over the lifetime.
Conclusions
Help seeking for substance use disorders has been shown to enhance the likelihood of recovery ( 33 ). A better understanding of the factors that facilitate or inhibit help seeking can help to improve the organization and delivery of treatment services to those who need them ( 34 ). This study showed that a wide range of factors influenced the perception of need for help and the receipt of help for alcohol or drug dependence. Longer duration of the disorder, specifically drug dependence, and more severe problems in functioning were key factors that promoted the receipt of treatment or other forms of assistance. Increasing the recognition of problems associated with substance dependence, particularly alcohol dependence, may facilitate help seeking, although barriers persist, especially among racial-ethnic minority groups and younger individuals.
Acknowledgments and disclosures
This work was supported by grant DA020944 from the National Institute on Drug Abuse (Dr. Karno, principal investigator).
The authors report no competing interests.
1. Wang PS, Lane M, Olfson M: Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Archives of General Psychiatry 62:629–640, 2005Google Scholar
2. Kessler RC, Nelson CB, McGonagle KA, et al: The epidemiology of co-occurring addictive and mental disorders: implications for prevention and service utilization. American Journal of Orthopsychiatry 66:17–31, 1996Google Scholar
3. Hasin DS, Stinson FS, Ogburn E, et al: Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States. Archives of General Psychiatry 64:830–842, 2007Google Scholar
4. Compton WM, Thomas YF, Stinson FS, et al: Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States. Archives of General Psychiatry 64:566–576, 2007Google Scholar
5. Wu L, Ringwalt CL, Williams CE: Use of substance abuse treatment services by persons with mental health and substance use problems. Psychiatric Services 54:363–369, 2003Google Scholar
6. Kessler RC, Zhao S, Katz SJ, et al: Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. American Journal of Psychiatry 156:115–123, 1999Google Scholar
7. Harris KM, Edlund MJ: Use of mental health care and substance abuse treatment among adults with co-occurring disorders. Psychiatric Services 56:954–959, 2005Google Scholar
8. Mojtabai R, Olfson M, Mechanic D: Perceived need and help-seeking in adults with mood, anxiety, or substance use disorder. Archives of General Psychiatry 59:77–84, 2002Google Scholar
9. Elhai JD, Ford JD: Correlates of mental health service use intensity in the National Comorbidity Survey and National Comorbidity Survey Replication. Psychiatric Services 58:1108–1115, 2007Google Scholar
10. Druss BG, Wang PS, Sampson NA, et al: Understanding mental health treatment in persons without mental diagnoses: results from the National Comorbidity Survey Replication. Archives of General Psychiatry 64:1196–1203, 2007Google Scholar
11. Andersen RM: Behavioral Model of Families' Use of Health Services. Research series no 25. Chicago, University of Chicago, Center for Health Administration Studies, 1968Google Scholar
12. Andersen RM: Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior 36:1–10, 1995Google Scholar
13. Grant BF, Dawson DA, Stinson FS, et al: The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence 71:7–16, 2003Google Scholar
14. Grant BF, Stinson FS, Dawson DA, et al: Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry 61:807–816, 2004Google Scholar
15. Conway KP, Compton W, Stinson FS, et al: Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry 67:247–257, 2006Google Scholar
16. Grant BF, Stinson FS, Dawson DA, et al: Co-occurrence of DSM-IV personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Comprehensive Psychiatry 46:1–5, 2005Google Scholar
17. Software for Survey Data Analysis (SUDAAN), Version 9.0. Research Triangle Park, NC, Research Triangle Institute, 2005Google Scholar
18. McLellan AT: Reducing heavy drinking: a public health strategy and a treatment goal? Journal of Substance Abuse Treatment 33:81–83, 2007Google Scholar
19. Urbanoski KA, Cairney J, Bassani DG, et al: Perceived unmet need for mental health care for Canadians with co-occurring mental and substance use disorders. Psychiatric Services 59:283–289, 2008Google Scholar
20. Miller WR, Rollnick S: Motivational Interviewing: Preparing People to Change Addictive Behavior. New York, Guilford, 1991Google Scholar
21. Regier DA, Kaelber CT, Rae DS, et al: Limitations of diagnostic criteria and assessment instruments for mental disorders: implications for research and policy. Archives of General Psychiatry 55:109–115, 1998Google Scholar
22. Narrow WE, Rae DS, Robins LN, et al: Revised prevalence estimates of mental disorders in the United States: using a clinical significance criterion to reconcile 2 surveys' estimates. Archives of General Psychiatry 59:115–123, 2002Google Scholar
23. Mechanic D: Is the prevalence of mental disorders a good measure of the need for services? Health Affairs 22(5):8–20, 2003Google Scholar
24. Mojtabai R: Use of substance abuse and mental health services in adults with substance use disorders in the community. Drug and Alcohol Dependence 73:345–354, 2005Google Scholar
25. Wells K, Klap R, Koike A, et al: Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. American Journal of Psychiatry 158:2027–2032, 2001Google Scholar
26. Keyes KM, Hatzenbuehler ML, Alberti P, et al: Service utilization differences for axis I psychiatric and substance use disorders between white and black adults. Psychiatric Services 59:893–901, 2008Google Scholar
27. Hines-Martin VP, Usui W, Kim S, et al: A comparison of influences on attitudes towards mental health service use in an African-American and white community. Journal of National Black Nurses Association 15:17–22, 2004Google Scholar
28. Alegría M, Canino G, Ríos R, et al: Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino whites. Psychiatric Services 53:1547–1555, 2002Google Scholar
29. Alvidrez J: Ethnic variations in mental health attitudes and service use among low-income African American, Latina, and European American young women. Community Mental Health Journal 35:515–530, 1999Google Scholar
30. Diala CC, Muntaner C, Walrath C, et al: Racial differences in attitudes toward seeking professional mental health care and in the use of services. American Journal of Orthopsychiatry 70:455–464, 2000Google Scholar
31. Anthony J, Neumark Y, Van Etten M: Do I do what I say? A perspective on self-report methods in drug dependence epidemiology; in The Science of Self-Report: Implications for Research and Practice. Edited by Stone A, Turkkan J, Bachrach C. Hillsdale, NJ, Erlbaum, 2000Google Scholar
32. Del Boca FK, Noll JA: Truth or consequences: the validity of self-report data in health services research on addictions. Addiction 95(suppl):S347–S360, 2000Google Scholar
33. Dawson DA, Grant BF, Stinson FS, et al: Estimating the effect of help-seeking on achieving recovery from alcohol dependence. Addiction 101:824–834, 2006Google Scholar
34. Stockdale SE, Klap R, Belin TR, et al: Longitudinal patterns of alcohol, drug, and mental health need and care in a national sample of US adults. Psychiatric Services 57:93–99, 2006Google Scholar



