Religiosity and Remission of Depression in Medically Ill Older Patients
Abstract
OBJECTIVE: The effects of religious belief and activity on remission of depression were examined in medically ill hospitalized older patients. METHOD: Consecutive patients aged 60 years or over who had been admitted to medical inpatient services at a university medical center were screened for depressive symptoms. Of 111 patients scoring 16 or higher on the Center for Epidemiologic Studies Depression Scale, 94 were diagnosed with depressive disorder (DSM-III major depression or subsyndromal depression) by a psychiatrist using a structured psychiatric interview. After hospital discharge, depressed patients were followed up by telephone at 12-week intervals four times. At each follow-up contact, criterion symptoms were reassessed, and changes in each symptom over the interval since last contact were determined. The median follow-up time for 87 depressed patients was 47 weeks. Religious variables were examined as predictors of time to remission by means of a multivariate Cox model, with controls for demographic, physical health, psychosocial, and treatment factors. RESULTS: During the follow-up period, 47 patients (54.0%) had remissions; the median time to remission was 30 weeks. Intrinsic religiosity was significantly and independently related to time to remission, but church attendance and private religious activities were not. Depressed patients with higher intrinsic religiosity scores had more rapid remissions than patients with lower scores. CONCLUSIONS: In this study, greater intrinsic religiosity independently predicted shorter time to remission. To the authors' knowledge, this is the first report in which religiosity has been examined as a predictor of outcome of depressive disorder.
Depression is a common problem among older patients hospitalized with medical illness. While the rate of major depression in community-dwelling older adults is less than 1% (1), it rises to above 10% in medically ill hospitalized elders (2). Including subsyndromal depression increases the percentage of elderly patients with depressive disorders to 35% or more (3). Many of these depressions are not transient and persist long after treatment of the medical illness and discharge from the hospital. Follow-up of depressed medical patients has shown that one-half to two-thirds continue to experience substantial depression at least 3 months after hospital discharge (4, 5). Besides reducing quality of life, depressive disorder appears to delay recovery from physical illness (6, 7), increase length of hospital stay (8, 9), and increase mortality (8, 10).
Despite depression's effects on morbidity and mortality, only a few studies have examined demographic, psychosocial, or health factors that influence changes in mood state over time in medical patients (4, 11). These studies have shown that severe medical illness, greater functional impairment, and poorer cognitive status are associated with persistent depressive symptoms, although no consistent predictors of outcome have been identified. A majority of these depressions, no doubt, result from difficulties older persons have adjusting to the discomfort, physical disability, and loss of control caused by their medical conditions. While coping resources such as social support or religion might facilitate such adaptation, their effects on recovery from depression in medical patients have been largely ignored—despite evidence suggesting their potential importance (12–14).
There has been increasing interest in the effects of religious belief and activity on mental health (15), particularly in regard to depression (16). Studies of elderly medical patients have shown that a substantial proportion (more than 50%) use religious belief or activity to cope with the stress of physical illness, and these patients appear less depressed than those who do not rely on religion (14, 17). Although the exact mechanism is uncertain, religious beliefs may provide a world view in which medical illness, suffering, and death can be better understood and accepted. Alternatively, they may provide a basis for self-esteem that is more resilient than sources that decline with increasing age and worsening health. To our knowledge, however, no study of either medical or psychiatric patients has examined the impact of religious factors on the course of depression.
This report comes out of a larger ongoing study of the diagnosis, course, and impact of depression in the medically ill elderly. Here we examined the effects of religious beliefs (intrinsic religiosity) and activities (prayer and Bible reading, church attendance) on time to remission from depression. We hypothesized that after the usual predictors of depression outcome, including change in physical functioning, were controlled for, these religious factors would be associated with a shorter time to remission.
METHOD
Between November 1993 and March 1996, consecutive patients admitted to the general medicine, cardiology, and neurology services of Duke University Medical Center were screened for depression. A patient was eligible if he or she was aged 60 years or over, was physically and cognitively well enough to undergo baseline evaluation, had consent from the attending physician, and was between days 3 and 7 of the hospital stay. After fully explaining the procedures and obtaining written informed consent from the patient, a research aid conducted a baseline evaluation in the patient's hospital room. The Center for Epidemiologic Studies Depression Scale (CES-D Scale) (18), the Mini-Mental State (19), and a wide range of other measures of physical and psychosocial functioning were included in the 1–2-hour baseline evaluation. Patients who scored 16 or higher on the CES-D Scale and 22 or higher on the Mini-Mental State were referred to a specialist in geriatric psychiatry for evaluation. Within 24 hours, the patient underwent a 1-hour structured psychiatric evaluation and physical examination. Patients who experienced three or more criterion symptoms of major depression and scored 11 or higher on the Hamilton Depression Rating Scale (20) were enrolled as “cases” in the longitudinal portion of the study. A research aid contacted the patients four times by telephone at 12-week intervals after study entry for 30–60-minute interviews.
Measures
Baseline depression. A cutoff score of 16 or higher on the self-rated 20-item CES-D Scale has a sensitivity of 73% and specificity of 84% for detecting depression in medically ill older inpatients (3, 21). To determine whether a depressive disorder was present in patients scoring 16 or higher on this scale, a psychiatrist administered the depressive disorders section of the National Institute of Mental Health Diagnostic Interview Schedule (DIS), a version that made depression diagnoses by using DSM-III criteria (22, 23). This interview schedule was expanded to assess 13 criterion symptoms—the traditional nine symptoms of major depression plus four substitute symptoms (irritability, feeling punished, feeling tearful, and social withdrawal)—since a study aim was to assess depressive disorder by using different diagnostic schemes (reported elsewhere) (24). The reliability of the expanded interview has been demonstrated previously in this population (25).
The diagnostic system used here to count symptoms used in the diagnosis of depression was the “inclusive” approach (26); this method is the most reliable and best overall method for counting symptoms for the diagnosis of depression in medically ill older patients (24, 25). To be considered as having a case of depression, a patient had to have experienced at least three out of the 13 criterion symptoms for 2 weeks or longer during the past month, score 11 or higher on the 17-item Hamilton depression scale, and score 16 or higher on the CES-D Scale.
Follow-up depression. Depressed patients were contacted at 12-week intervals by a research aid who administered the Duke Telephone Follow Up Schedule, a structured interview that follows the DIS, tracking each of the criterion symptoms on a weekly basis. If a criterion symptom had been present at the time of the previous interview (either the baseline psychiatric evaluation or the previous telephone contact), the patient was asked whether he or she still had the symptom and, if not, how many weeks previously the symptom had improved. If a criterion symptom had not been present at the previous interview, the patient was asked whether he or she had experienced 2 weeks or more of the symptom at any time during the interval since last contact; if so, he or she was asked when the symptom had begun and whether the symptom was still present. This was done for each of the 13 criterion symptoms. Thus, a week-by-week count of symptoms (ranging from 0 to 13) was obtained, allowing a reconstruction of the course of depression during the interval since the last interview. The reliability of the DIS when administered by telephone has been previously established (27), as has the reliability of the DIS-like structured telephone follow-up schedule used in the present study (24).
Criteria for remission of depression. In accordance with guidelines set by Frank et al. (28), a full remission was defined as 2 weeks or more of fewer than three of the nine traditional DSM-III criterion symptoms. Time to remission was the number of weeks between the baseline evaluation and the first time when this criterion was met during the follow-up period.
Physical health. Physical illness severity was measured by using four methods based on review of the patient's medical record and a physical examination. First, the primary medical diagnosis and all other active medical conditions were categorized into 28 major classes according to ICD-9; the total number of medical conditions was determined by summing the number of positive categories (score range=0–28). Next, the physician completed the Duke University Severity of Illness scale (29) and the Cumulative Illness Rating Scale (30). The Duke University Severity of Illness scale assesses prognosis (score range=0–3), complications (score range=0–3), and symptom level (score range=0–3) for up to four active medical diagnoses (total score range=0–36). The Cumulative Illness Rating Scale assesses impairment on 5-point scales (score range=0–4) for 12 major organ systems (total score range=0–48). Finally, the research aid asked the patient about his or her ability to perform eight physical (31) and 12 instrumental (32) activities of daily living during the baseline evaluation and at each of the four follow-ups; for analysis purposes, change in physical functioning was determined by subtracting the number of impaired activities of daily living during the last follow-up interview from the number at baseline.
Mental health. Past psychiatric history was determined by asking each patient whether he or she had 1) ever had any mental or nervous condition that required some form of treatment and 2) ever taken nerve medication for any reason. Family psychiatric history was assessed by asking the patient whether any blood relative had 1) ever had a mental or nervous condition, 2) ever seen a psychiatrist or been admitted to a psychiatric hospital, 3) ever took nerve medicine for 3 months or more, and 4) ever made a suicide attempt or committed suicide. Dysfunctional attitudes were assessed by means of a 15-item scale developed specifically for medically ill hospitalized elders (score range=15–60) (Cronbach's alpha=0.83) (33). Life stressors were assessed with a 12-item index that includes questions about common negative life events experienced during the past year and the degree to which these events affected the patient's life (score range=0–84). Finally, quality of life was measured by using the Quality of Life Index (34), which globally assesses five domains: general activity, ability to perform self-care activities, overall physical health, supportive relationships, and outlook on life (score range=0–10).
Religion. Intrinsic religiosity was measured by using a scale consisting of 10 statements about religious belief or experience (35). Patients were asked to mark on a 1–5 scale the extent to which they felt each statement was true for them (score range=10–50). The scale has both high internal reliability (Cronbach's alpha=0.87) and high test-retest reliability (91.3% agreement after a 6-week interval). Its validity has been examined in two studies. In the original study, Hoge (35) found a high correlation between scale scores and ministers' judgments (r=0.59). In the second study, the scale was administered to 85 ministers representing 18 Christian denominations and two Jewish groups; the ministers were asked to predict the response they felt an intrinsically religious person would make to each item. A predicted score of 50 indicates perfect scale validity; the mean score predicted by the ministers was 46.5 (SD=5.1) (36). The scale is also strongly correlated with Allport's intrinsic religiosity subscale (r=0.86) and Feagin's intrinsic religiosity scale (r=0.87) (35).
Nonorganizational religious activities were measured by asking the single question “How often do you spend time in private religious activities such as prayer, meditation, or Bible study?” (“rarely or never” to “more than once/day”; score range=1–6). Organizational religious activities were measured by asking the question “How often do you attend church or other religious meetings?” (“never” to “more than once/week”; score range=1–6). The patient was also asked to give his or her religious denomination, which was categorized into one of 57 different groups.
Social support. The 11-item version of the Duke Social Support Index assessed two major components of social support—social network and subjective support (37). This version was developed specifically for chronically ill elders and differs from the full 35-item version primarily by not containing the social interaction and instrumental support subscales.
Treatment of depression. After discharge, the patient's medical record was systematically reviewed by a physician for antidepressant use; this record included the final medication record, which listed all medicines received during hospitalization, and the discharge summary, which listed all discharge medications. The reliability of this method for identifying antidepressant use during hospitalization has been established (38). In addition, all nurses' and physicians' notes were examined for documentation of psychotherapy during hospitalization or plans for it after discharge. Finally, the patients were asked at each of the four telephone follow-up contacts to list the medications they were currently taking, including any medications for depression or nerves; only antidepressant use was considered for this report. No one received ECT.
Statistical Analyses
The outcome variable, time to first remission, was determined from yes/no weekly assessments of depression during the follow-up period (as already described); patients whose depression did not remit during follow-up were censored at the time they were last known to be depressed. Bivariate and multivariate predictors of time to first remission were examined by using a Cox proportional hazards regression model (39). The validity of the proportional hazards assumption was examined both graphically and with the normal score test of proportionality (40).
To test the primary hypothesis, each of the three religious variables was examined separately as a predictor of time to remission. If an association was found, other significant predictors of remission were included in a multivariate Cox model in order to control for their effects on the relationship between religion and depression outcome. To determine which variables to control for, the effects of 27 candidate predictor variables on outcome were examined bivariately; significant predictors (defined as p<0.10) were included in the multivariate Cox model just described. A backwards elimination procedure removed nonsignificant variables from the model. Interactions between the religious variable and other predictors in the final model were assessed. The results were presented as estimated hazard ratios with 95% confidence intervals. For continuous variables (e.g., quality of life, intrinsic religiosity), hazard ratios were calculated on the basis of the change from the 25th to 75th percentile in the distribution of the variables. Finally, Kaplan-Meier curves were used to compare the low-, medium-, and high-religiosity groups on time to first remission.
RESULTS
Study Group
At baseline, 113 patients scored 16 or higher on the CES-D Scale; of these, 111 (98.2%) were examined by a psychiatrist within 24 hours by means of the expanded DIS. Patients fulfilling the criteria for depression (N=94) were enrolled in the follow-up study. Of the enrolled patients, five died before the first follow-up and two dropped out, leaving 87 patients (92.6%) with at least one follow-up. Of these, 67 (77.0%) completed all follow-ups, 15 died before all follow-ups were completed, three refused one or more interviews, and two could not be located for one interview each. Because of patient disability, sickness, or refusal, proxy interviews were performed in 22 (7.4%) of the 299 follow-up contacts. Characteristics of the study group are listed in table 1; 96.6% (N=84) came from Christian backgrounds (56.3% were Baptist, N=49).
Of the 87 patients in the final study group, 50 had major depression and 37 did not (subsyndromal depression). According to the Clinical Global Impressions scale (41), 62.1% (N=54) had mild depression (score<4), 31.0% (N=27) had moderately severe depression (score=4), and 6.9% (N=6) had markedly severe depression (scores>4). The average duration of depressed mood before evaluation was 12.8 weeks (SD=22.7); only two patients had mood symptoms lasting 2 years or longer (dysthymia). The median follow-up time was 47 weeks (range=2–60).
Course of Depression
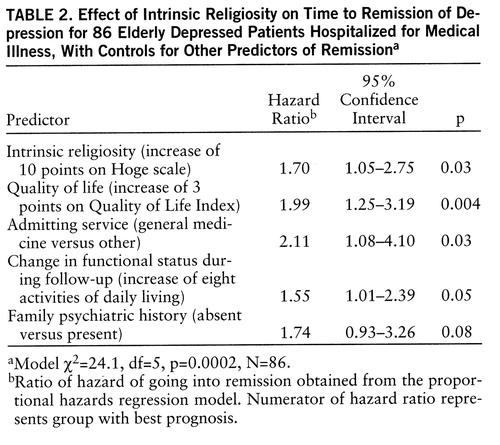
Of the 87 patients with at least one contact, 47 (54.0%) experienced remission during the follow-up period. Of the 67 who completed all four follow-up contacts, 39 (58.2%) had remissions. The median time to remission was 30 weeks, and the range was 1 to 50 weeks (estimated from Kaplan-Meier curve, figure 1).
Religion and Time to Remission
Intrinsic religiosity was significantly related to time to remission of depression (hazard ratio=1.54, 95% confidence interval=1.00–2.39, p=0.05) in the bivariate analysis. While the effects were in the expected direction, the frequency of church attendance (hazard ratio=1.35, 95% confidence interval=0.91–1.97) and private religious activities (hazard ratio=1.09, 95% confidence interval=0.77–1.66) were unrelated to time to remission.
Twenty-seven demographic, physical health, mental health, social, and treatment factors (variables in table 1) were then examined as potential covariates needing to be controlled for in assessing the association between intrinsic religiosity and time to remission. Six of these variables significantly predicted time to remission: quality of life, change in functional status during follow-up, family psychiatric history, number of medical diagnoses, social support, and treatment with antidepressants during follow-up. These variables were then included along with intrinsic religiosity in a multivariate Cox model to control for their effects.
Four variables predicted shorter time to remission in this model: high intrinsic religiosity, high quality of life, change in functional status (e.g., decreased impairment in activities of daily living), and absence of family psychiatric history. The nonsignificant variables from table 1 were again examined one at a time in the final model to ensure that none was confounding the relationship between intrinsic religiosity and depression outcome; in this way, admitting service (general medicine versus other) became significant and was added to the model. Thus, the final model included intrinsic religiosity, quality of life, admitting service, change in functional status, and family psychiatric history (table 2).
Thus, after other significant predictors were controlled for, patients with higher intrinsic religiosity scores experienced faster remission of depression than did those with lower scores. For every 10-point increase in intrinsic religiosity score, there was a 70% increase in speed of remission (table 2). No interactions between intrinsic religiosity and the other variables in the final model reached statistical significance; however, the relationship between intrinsic religiosity and time to remission tended to be stronger among those whose physical functioning worsened or only minimally improved after discharge (hazard ratio=2.06, 95% confidence interval=1.02–4.15, for 48 patients with changes in the score for activities of daily living of –12 to 3) than among those who had a more substantial improvement in physical functioning (hazard ratio=1.43, 95% confidence interval=0.74–2.81, for 38 patients with changes in the score for activities of daily living greater than 3). In order to visually display the relationship between intrinsic religiosity and time to remission, we divided the patients into three groups on the basis of their intrinsic religiosity scores (lower one-third, middle one-third, and upper one-third) and constructed a Kaplan-Meier depression survival curve for each group (figure 2).
Because of concern that religious patients may be more likely to deny or conceal depressive symptoms, we examined the relationship between baseline intrinsic religiosity and baseline depression. For this analysis we compared the 87 depressed patients with 77 nondepressed comparison subjects (patients with CES-D Scale scores of 10 or less, Hamilton depression scale scores of 10 or less, and two or fewer criterion symptoms). The average intrinsic religiosity scores for the depressed (mean=39.4, SD=8.2) and comparison subjects (mean=39.6, SD=7.8) at baseline were similar. On initial evaluation, then, religiosity did not appear to affect symptom report.
DISCUSSION
To our knowledge, this is the first prospective study to examine the effects of religiosity on depression outcome. Depressed older adults hospitalized with medical illness were identified, and the course of their depressive disorders was tracked for almost a year. A little over one-half of these patients went into full remission during this period, many (almost 50%) without any formal treatment for their depression. On the basis of prior studies, we hypothesized that religious factors might play a role in the remission of depression in this population.
Intrinsic religiosity did predict shorter time to remission, an effect that persisted after we controlled for multiple demographic, psychosocial, physical health, and treatment factors. For every 10-point increase in intrinsic religiosity score, there was a 70% increase in the speed of remission. There was no evidence that this effect was due to religious persons being less likely to report depressive symptoms. While the effects were in the expected direction, neither church attendance nor private religious activities significantly predicted faster resolution of depression. This was true despite the fact that both church attendance and private religious activities were strongly related to intrinsic religiosity (Pearson r=0.39 and r=0.44, respectively, N=87, p<0.0005).
Might confounding explain this association? While it is possible that some unmeasured variable related to both intrinsic religiosity and faster remission of depression might explain this association, it is unlikely, given that we measured and controlled for almost all known predictors of depression course. What about biased outcome assessments? Research assistants doing the telephone follow-up evaluations were blind to the study hypotheses and were largely blind to the religiosity of patients, which was assessed only once (in the midst of a 1–2-hour baseline interview) and never examined again.
What about a chance association? A major research question in 1993, when this study was initiated, was whether or not religiousness predicted faster remission of depression. This was of particular interest because we had found in an earlier study of 850 hospitalized veterans that religious coping was inversely related to depressive symptoms both at baseline and on follow-up (202 patients followed an average of 6 months). In that study, the religious variable accounted for 45% of the explained variance in follow-up depression scores (14).
Finally, as part of the current study, we asked the 87 depressed patients at study entry an open-ended question about what they thought enabled them to cope with the stress of their physical illness and other depressing things in their lives. One-third (32.6%, 28 of 86) spontaneously and without prompting gave religious responses (“God,” “the Lord,” “my faith,” “prayer,” “Jesus,” and so forth). All patients were then asked to rate on a 0 to 10 scale the extent to which they used religion to help them to cope with their condition; almost two-thirds (63.5%, 54 of 85) indicated 7.5 (“a large extent”) or higher. Thus, before any outcome assessments, we were told by patients that religion was an important factor that enabled them to cope. This supports the credibility of the finding that higher intrinsic religiosity predicted faster remission of depression and argues against it being due to confounding, chance, or bias of study investigators.
While this may be the first report on religion's effects on the course of depression, it is not the first time that investigators have examined the relationship between intrinsic religiosity and depression in older adults. Three (42–44) of four such studies showed a significant inverse relationship between these variables, with an average uncontrolled correlation of r=–0.27; they also showed significant associations with high self-esteem, with uncontrolled correlations averaging r=0.34. The fourth study of bereaved elders (45) indicated no relationship between depression and intrinsic religiosity, but there was a significant positive association between depression and extrinsic religiosity. Other studies have examined relationships between intrinsic religiosity and variables such as well-being (46) and internal locus of control (47); in both studies there were significant and positive correlations. Allport and Ross (48) described the intrinsically religious person as follows:
Persons with this orientation find their master motive in religion. Other needs, strong as they may be, are regarded as of less ultimate significance, and they are, so far as possible, brought into harmony with the religious beliefs and prescriptions. Having embraced a creed, the individual endeavors to internalize it and follow it fully. It is in this sense that he lives his religion. (p. 434)
Thus, intrinsic religiosity, while related to church going and frequency of private religious activities, is not the same. Neither of these religious activities measures the extent to which religion is the master, motivating factor in peoples' lives that drives their behavior and decision making. Furthermore, unlike church attendance, intrinsic religiosity is not limited by health problems, which may even increase it.
Older persons with an intrinsically motivated religious faith may indeed be more able to cope with changes in their physical health and living circumstances because their self-esteem and sense of well-being are not as tied to either their ability to produce or their material circumstances. As these latter resources diminish with increasing health problems and disability, religious beliefs and cognitions may remain little affected. In this study we found that intrinsic religiosity was a particularly strong predictor of time to remission in patients whose physical functioning since hospitalization had either worsened or improved only minimally. Religious faith may provide such persons with a sense of hope that things will turn out all right regardless of their problems and, thus, foster greater motivation to achieve emotional recovery.
Treatment had no effect on depression outcome, regardless of whether patients had major depression or subsyndromal depression. Such a finding is not surprising and is likely due to 1) the case mix of patients in a naturalistic study (some who had recently begun treatment, others having been treated for many months) and 2) inadequate treatment by nonpsychiatrists (subthera~peutic doses of tricyclics such amitriptyline, excessive doses of selective serotonin reuptake inhibitors, short duration of treatment due to discontinuation, and lack of follow-up or dose monitoring) (38).
The results of this study should be generalized with caution for several reasons. First, our study group was unique in that it consisted of patients hospitalized for medical problems who had relatively mild depressions. These results may not necessarily generalize to depressed older adults seen for treatment in psychiatric settings or to those with melancholic or more severe depressions. Second, this study took place in the Bible Belt region of the United States, where religion is deeply ingrained in the culture and social fabric of society. A comparison of the religious characteristics of our study group with those of older adults in the overall United States, however, shows smaller differences than one might expect. For example, 45% of our study group reported attending church weekly or more often, compared with 53% of older adults nationally (49). Likewise, 63% of our study group said they spent time in prayer, meditation, or Bible study once a day or more, compared with 95% of older Americans who say they pray (50) and 59% who read the Bible three or more times per week (51). The religious activity of our study group, then, is consistent with the high degree of religious activity among older Americans in general.
Religious beliefs and behaviors are commonly used by depressed older adults to cope with medical problems and may lead to faster resolution of some types of depression. Psychiatrists should feel free to inquire about and support the healthy religious beliefs and activities of older patients with disabling physical health problems, realizing that these beliefs may bring comfort and facilitate coping.
 |
 |
Received Jan. 15, 1997; revision received Aug. 29, 1997; accepted Oct. 31, 1997. From the Department of Psychiatry, the Department of Medical Sociology, the Center for the Study of Aging and Human Development, and the Biometry Division, Department of Family and Community Medicine, Duke University Medical Center. Address reprint requests to Dr. Koenig, Department of Psychiatry, Box 3400, Duke University Medical Center, Durham, NC 27710; [email protected] (e-mail). Funded by NIMH Clinical Mental Health Academic Award MH-01138 (Dr. Koenig) and, in part, by National Institute on Aging Claude D. Pepper Older Americans Independence Centers grant AG-11268, NIMH Clinical Research Center grant MH-40159, and a grant from the John Templeton Foundation (Dr. Koenig).
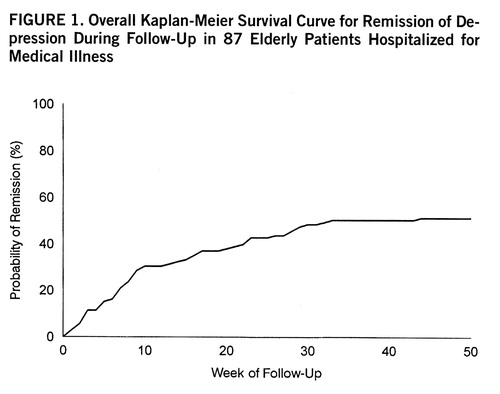
FIGURE 1. Overall Kaplan-Meier Survival Curve for Remission of Depression During Follow-Up in 87 Elderly Patients Hospitalized for Medical Illness

FIGURE 2. Kaplan-Meier Survival Curves for Remission of Depression During Follow-Up in 87 Elderly Patients Hospitalized for Medical Illness Who Were Classified by Level of Intrinsic Religiositya
aSubjects were subdivided into thirds on the basis of scores on the Hoge scale (35).
1 Regier DA, Boyd JH, Burke JD Jr, Rae DS, Myers JK, Kramer M, Robins LN, George LK, Karno M, Locke BZ: One-month prevalence of mental disorders in the United States: based on five Epidemiologic Catchment Area sites. Arch Gen Psychiatry 1988; 45:977–986Crossref, Medline, Google Scholar
2 Koenig HG, Blazer DG: Epidemiology of geriatric depression. Clin Geriatr Med 1982; 8:235–251Google Scholar
3 Koenig HG, O'Connor C, Guarisco S, Zabel M, Ford S: Depressive disorder in elderly inpatients admitted to general medicine and cardiology services at a private hospital. Am J Geriatr Psychiatry 1993; 1:197–210Crossref, Medline, Google Scholar
4 Koenig HG, Goli V, Shelp F, Kudler HS, Cohen HJ, Blazer DG: Major depression in hospitalized medically ill men: documentation, treatment, and prognosis. Int J Geriatr Psychiatry 1992; 7:25–34Crossref, Google Scholar
5 Schleifer SJ, Macari-Hinson MM, Coyle DA, Salter WR, Kahn M, Gorlin R, Zucker HD: The nature and course of depression following myocardial infarction. Arch Intern Med 1989; 149:1785–1789Crossref, Medline, Google Scholar
6 Parikh R, Robinson RG, Lipsey JR, Starkstein S, Fedoroff J, Price TR: The impact of poststroke depression on recovery in activities of daily living over a 2-year followup. Arch Neurology 1990; 47:785–789Crossref, Medline, Google Scholar
7 Mossey JM, Knott K, Craik R: The effects of persistent depressive symptoms on hip fracture recovery. J Gerontol 1990; 45:M163–M168Google Scholar
8 Koenig HG, Shelp F, Goli V, Cohen HJ, Blazer DG: Survival and healthcare utilization in elderly medical inpatients with major depression. J Am Geriatr Soc 1989; 37:599–606Crossref, Medline, Google Scholar
9 Fulop G, Strain JJ, Vita J, Lyons JS, Hammer JS: Impact of psychiatric comorbidity on length of hospital stay for medical/surgical patients: a preliminary report. Am J Psychiatry 1987; 144:878–882Link, Google Scholar
10 Frasure-Smith N, Lesperance F, Talajic M: Depression following myocardial infarction: impact on 6-month survival. JAMA 1993; 270:1819–1825Crossref, Medline, Google Scholar
11 Rapp SR, Parisi SA, Wallace CE: Comorbid psychiatric disorders in elderly medical patients: a 1-year prospective study. J Am Ger~iatr Soc 1991; 39:124–131Crossref, Google Scholar
12 George LK: Social factors and the onset and outcome of depression, in Aging, Health Behaviors, and Health Outcomes. Edited by Schaie KW, House JS, Blazer DG. Hillsdale, NJ, Lawrence Erlbaum Associates, 1992, pp 137–159Google Scholar
13 George L, Blazer D, Hughes D, Fowler N: Social support and the outcome of major depression. Br J Psychiatry 1989; 154:478–485Crossref, Medline, Google Scholar
14 Koenig HG, Cohen HJ, Blazer DG, Pieper C, Meador KG, Shelp F, Goli V, DiPasquale R: Religious coping and depression among elderly, hospitalized medically ill men. Am J Psychiatry 1992; 149:1693–1700Link, Google Scholar
15 Marwick C: Should physicians prescribe prayer for health? spiritual aspects of well-being considered. JAMA 1995; 273:1561–1562Crossref, Medline, Google Scholar
16 Andreasen NJ: The role of religion in depression. J Religion & Health 1972; 11:153–166Crossref, Medline, Google Scholar
17 Pressman P, Lyons JS, Larson DB, Strain JJ: Religious belief, depression, and ambulation status in elderly women with broken hips. Am J Psychiatry 1990; 147:758–760Link, Google Scholar
18 Radloff LS: The CES-D Scale: a self-report depression scale for research in the general population. J Applied Psychol Measurement 1977; 1:385–401Crossref, Google Scholar
19 Folstein MF, Folstein SE, McHugh PR: “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12:189–198Crossref, Medline, Google Scholar
20 Hamilton M: Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol 1967; 6:278–296Crossref, Medline, Google Scholar
21 Radloff L, Teri L: Use of the CES-D Scale with older adults. Clin Gerontologist 1986; 5:119–136Crossref, Google Scholar
22 Robins LN, Helzer JE, Croughan J, Ratcliff KS: The National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Arch Gen Psychiatry 1981; 38:381–389Crossref, Medline, Google Scholar
23 Koenig HG, Goli V, Shelp F, Meador KG, Blazer DG: Major depression and the NIMH Diagnostic Interview Schedule: validation in medically ill hospitalized patients. Int J Psychiatry Med 1989; 19:123–132Crossref, Medline, Google Scholar
24 Koenig HG, George LK, Peterson BL, Pieper CF: Depression in medically ill hospitalized older adults: prevalence, characteristics, and course of symptoms according to six diagnostic schemes. Am J Psychiatry 1997; 154:1376–1383Link, Google Scholar
25 Koenig HG, Pappas P, Holsinger T, Bachar JR: Assessing diagnostic approaches to depression in medically ill older adults: how reliably can mental health professionals make judgments about the cause of symptoms? J Am Geriatr Soc 1995; 43:472–478Google Scholar
26 Cohen-Cole SA, Stoudemire A: Major depression and physical illness: special considerations in diagnosis and biologic treatment. Psychiatr Clin North Am 1987; 10:1–17Crossref, Medline, Google Scholar
27 Wells KB, Burnam MA, Leake B, Robins LN: Agreement between face-to-face and telephone-administered versions of the depression section of the NIMH Diagnostic Interview Schedule. J Psychiatr Res 1988; 22:207–220Crossref, Medline, Google Scholar
28 Frank E, Prien RF, Jarrett RB, Keller MB, Kupfer DJ, Lavori PW, Rush AJ, Weissman MM: Conceptualization and rationale for consensus definitions of terms in major depressive disorder: remission, recovery, relapse, and recurrence. Arch Gen Psychiatry 1991; 48:851–855Crossref, Medline, Google Scholar
29 Parkerson G, Michener J, Wu L, Finch J, Mulhbaier L, Magruder-Habib K, Kertesz J, Clapp-Channing N, Morrow D, Chen A, Jokerst E: Associations among family support, family stress, and personal functional health status. J Clin Epidemiol 1989; 42:217–229Crossref, Medline, Google Scholar
30 Conwell Y, Forbes NT, Cox C, Caine ED: Validation of a measure of physical illness burden at autopsy: the Cumulative Illness Rating Scale. J Am Geriatr Soc 1993; 41:38–41Crossref, Medline, Google Scholar
31 Katz S, Ford A, Moskowitz R, Jackson B, Jaffe M: Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA 1963; 185:94–99Crossref, Google Scholar
32 Multidimensional Functional Assessment: The OARS Methodology. Durham, NC, Duke University Center for the Study of Aging and Human Development, 1978Google Scholar
33 Koenig HG, George LK, Robins CJ, Stangl D, Tweed DL: The development of a Dysfunctional Attitudes Scale for Medically Ill Elders (DASMIE). Clin Gerontologist 1994; 15(2):3–22Google Scholar
34 Spitzer WO, Dobson AJ, Hall J, Chesterman E, Levi J, Shepherd R, Battista RN, Catchlove BR: Measuring the quality of life of cancer patients: a concise QL-index for use by physicians. J Chronic Dis 1981; 34:585–597Crossref, Medline, Google Scholar
35 Hoge DR: A validated intrinsic religious motivation scale. J Scientific Study of Religion 1972; 11:369–376Crossref, Google Scholar
36 Koenig HG, Smiley M, Gonzales J: Religion, Health, and Aging. Westport, Conn, Greenwood Press, 1988, p 175Google Scholar
37 Koenig HG, Westlund RE, George LK, Hughes DC, Hybels C: Abbreviating the Duke Social Support Index for use in chronically ill older adults. Psychosomatics 1993; 34:61–69Crossref, Medline, Google Scholar
38 Koenig HG, George LK, Meador KG: Use of antidepressants by nonpsychiatrists in the treatment of medically ill hospitalized depressed elderly patients. Am J Psychiatry 1997; 154:1369–1375Link, Google Scholar
39 Cox DR: Regression models and life tables. J R Statistical Society 1972; 34(Series B):187–220Google Scholar
40 Grambsch PM, Therneau TM: Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 1994; 81:515–526Crossref, Google Scholar
41 Guy W (ed): ECDEU Assessment Manual for Psychopharmacology: Publication ADM 76-338. Rockville, Md, US Department of Health, Education, and Welfare, 1976, pp 217–222Google Scholar
42 Nelson PB: Ethnic differences in intrinsic/extrinsic religious orientation and depression in the elderly. Arch Psychiatr Nursing 1989; 3:199–204Medline, Google Scholar
43 O'Connor BP, Vallerand RJ: Religious motivation in the elderly: a French-Canadian replication and an extension. J Soc Psychol 1990; 130:53–59Crossref, Medline, Google Scholar
44 Koenig HG: Religion and older men in prison. Int J Geriatr Psychiatry 1994; 10:219–230Crossref, Google Scholar
45 Rosik CH: The impact of religious orientation in conjugal bereavement among older adults. Int J Aging Hum Dev 1989; 28:251–260Crossref, Medline, Google Scholar
46 Koenig HG, Kvale JN, Ferrel C: Religion and well-being in later life. Gerontologist 1988; 28:18–28Crossref, Medline, Google Scholar
47 Kivett VR: Religious motivation in middle age: correlates and implications. J Gerontol 1979; 34:106–115Crossref, Medline, Google Scholar
48 Allport GW, Ross JM: Personal religious orientation and prejudice. J Pers Soc Psychol 1967; 5:432–443Crossref, Medline, Google Scholar
49 Princeton Religion Research Center: Religion in America. Princeton, NJ, Gallup Poll, 1996, p 29Google Scholar
50 Princeton Religion Research Center: Religion in America 1992–1993: 1994 Supplement. Princeton, NJ, Gallup Poll, 1994, p 10Google Scholar
51 Barna G: What Americans Believe. Ventura, Calif, Regal Books, 1991, p 291Google Scholar



