From Postmortem Molecular Studies to Social Determinants of Health Relevant to Racial and Ethnic Disparities
Understanding and taking measures to mitigate race and ethnic-related disparities in mental health, well-being, and psychiatric care should be among the highest priorities for our field. Consistent with this priority, this issue of the Journal highlights how social determinants of health contribute to such race and ethnic-related disparities, beginning with an overview by Dr. Margarita Alegría from Harvard Medical School and her co-authors (1) on the social determinants of health as they relate to disparities in psychiatric care and mental health. In addition to reviewing what is known about the role of social determinants of health in mental illness, this piece provides recommendations for designing studies and implementing remedies aimed at the social determinants of health that lead to race and ethnic-related disparities. This overview complements a research paper and an accompanying editorial that focus on disparities in depression symptoms, measures of cognition, and self-reported assessments of health in older Black and Hispanic/Latinx individuals.
Additionally, this issue brings together papers that are relevant to schizophrenia and dementia. Two studies add to the understanding of molecular alterations and biomarkers in schizophrenia. The first uses postmortem brain tissue from individuals with schizophrenia to characterize alterations in dorsolateral prefrontal cortical interneurons that may play a mechanistic role in the cognitive symptoms associated with schizophrenia. The second is a priority data letter that has direct implications for treating schizophrenia as it characterizes the effects of drugs with anticholinergic effects on brain electrophysiological biomarkers that accompany anticholinergic-related cognitive alterations. Also in this issue is a study that uses repeated neuroimaging to longitudinally assess a large cohort of individuals to establish how small vessel cerebrovascular disease relates to the later development of dementia.
Social Determinants of Health Associated With Depression and Well-Being in Older Black, Hispanic/Latinx, and White Individuals
Jester and colleagues (2) identify critical factors that are associated with mental health disparities in older Black and Hispanic/Latinx individuals. In this report, using data from over 11,000 individuals (51–89 years old) from the Health and Retirement Study, the researchers characterize differences among Black, Hispanic/Latinx, and White individuals in relation to symptoms of depression, measures of cognition, and self-rated health. Consistent with previous studies, Black and Hispanic/Latinx, compared to White, individuals scored worse for depression symptoms as well for measures of cognition and health. The researchers next assessed the extent to which the social determinants of health were associated with these race and ethnic-related differences. The measures used for the social determinants of health included education years, parents’ education years, number of years worked, marital status, veteran status, living in different regions of the United States, foreign or U.S. born, household income, employer-sponsored health insurance, Medicare, and Medicaid. When comparing Black and White individuals, the social determinants of health accounted for 51% of the differences in depression symptoms, 39% of the differences in cognition ratings, and 37% of the differences in self-assessments of health. These effects were greater than those for other health-related factors such as age, sex, health-related behaviors, and health care utilization. When comparing Hispanic/Latinx to White individuals, the social determinants of health accounted for only 28% of the differences in depression symptoms but explained 76% of the differences in cognition and 75% of the differences in self-reported health. In their editorial (3), Drs. Javier Escobar and William Vega from Florida International University and Dr. Carlos Jaramillo from the University of Antioquia discuss the importance and implications of these findings while providing a broad overview of issues relevant to research that is focused on health care disparities related to race and ethnicity.
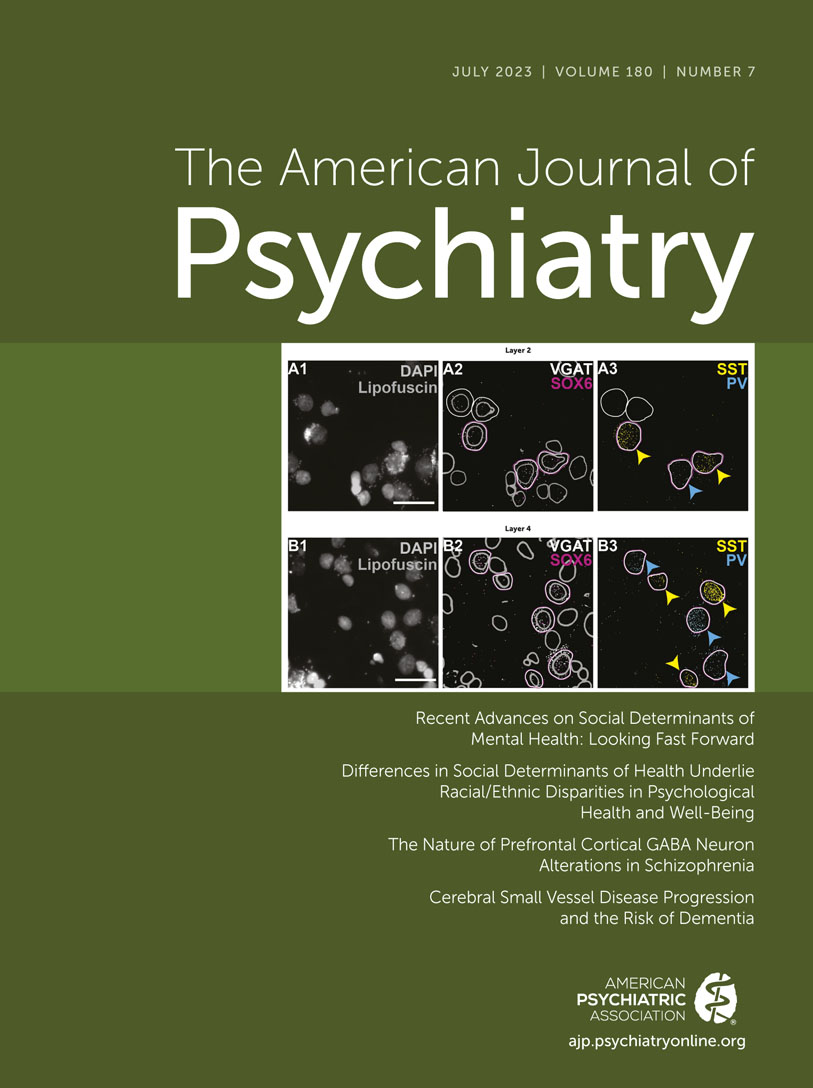
Schizophrenia-Related GABA Neuronal Alterations in the Dorsolateral Prefrontal Cortex
Numerous neuroimaging and postmortem studies have described functional, structural, and molecular alterations in the dorsolateral prefrontal cortex (dlPFC) of individuals with schizophrenia. Understanding the molecular alterations that underlie altered dlPFC function in schizophrenia patients is a critical step toward conceptualizing new treatments directed at symptoms associated with altered cognition and executive function. Of particular interest are postmortem findings that have implicated changes in prefrontal cortical GABA interneurons, which function to provide inhibitory input to other cortical neurons, especially excitatory glutamatergic neurons. There are numerous subtypes of GABA interneurons, and two subtypes relevant to schizophrenia are identified by the presence of mRNAs for either the calcium binding protein parvalbumin (PV) or the peptide somatostatin (SST). In both cases, reductions in mRNAs for these molecules have been reported in the prefrontal cortex of brains from individuals with schizophrenia. An important issue with therapeutic implications that has not yet been clearly resolved is whether the reductions in PV and SST mRNAs are due to a decrease in the number of neurons that express these molecules or rather to decreased production of PV and SST within a normal number of neurons. To resolve this question, Dienel and colleagues (4) report findings from a method that independently and concurrently identifies the density of PV and SST GABA neurons in layers two and four of the dlPFC and the amount of mRNA for PV and SST within these neurons. Dorsolateral prefrontal cortex tissue from 30 brains from individuals with schizophrenia and 30 matched controls was studied. It is important to note that the schizophrenia brains selected for study had previously been demonstrated to have low levels of PV and SST mRNA in dlPFC neurons. The findings from this subset of individuals with schizophrenia revealed that the observed reduction in PV and SST mRNA levels are due to decreased gene expression occurring in a normal number of neurons rather than a decreased density of PV or SST GABA neurons. Moreover, the authors covaried for other factors associated with schizophrenia such as death by suicide, substance use disorder at time of death, and use of psychopharmacologic agents at time of death, and found that these analyses did not affect the findings. To the extent that dlPFC PV and SST GABA neurons are involved in the pathophysiology of schizophrenia, these findings point to therapeutic strategies aimed at modulating the function of these dlPFC GABA interneuron subtypes. In their editorial (5), Drs. Joel Kleinman and Thomas Hyde from the Lieber Institute for Brain Development discuss the meaning of the findings while emphasizing the importance of postmortem brain studies in psychiatry.
Small Vessel Disease in the Brain and the Development of Dementia
While cerebrovascular disease has been associated with dementia, it has been difficult to causally link small vessel cerebrovascular disease to the later development of dementia. In this regard, Jacob and colleagues (6) followed a cohort of individuals with cerebral small vessel disease (SVD) to characterize cerebrovascular risk factors associated with the later onset of dementia. The participants in the study with sporadic SVD and not dementia (N=503) were recruited from a neurology outpatient clinic in the Netherlands and followed for 14 years. MRIs were performed to characterize SVD, which included assessment of white matter hyperintensities, lacunes, and evidence of cerebral microbleeds as well as the integrity of white matter. Of the 498 participants in whom dementia was assessed, 21.5% or 108 individuals developed dementia (of these: 35% Alzheimer’s, 32%, vascular, and 24% mixed). Results demonstrated that the degree of SVD at initial evaluation, and the magnitude of the progression of SVD characterized in the 364 individuals in which at least two MRIs were acquired, predicted the development of dementia. The SVD markers tended to be more associated with the development of vascular dementia, whereas decreased hippocampal volume, less white matter hyperintensities, and less affected white matter tracts were associated with the development of Alzheimer’s disease. This study is distinguished by its long period of follow-up, which the authors argue allows them to infer a causal relationship between the severity of SVD and the later development of dementia. Additionally, the authors suggest that intervention strategies aimed at reducing the progression of SVD could protect vulnerable individuals from developing dementia. In his editorial, Dr. David Steffens (7) from the University of Connecticut provides a general discussion related to cerebrovascular dementias and highlights the strengths of the Jacob et al. study, including the methods used and the importance of the long-term follow-up period.
Anticholinergic Burden Is Associated With Schizophrenia-Related Alterations in Neurophysiological Biomarkers
Psychotropic medications with anticholinergic effects, most notably antipsychotic and some antidepressant drugs, are commonly used to treat psychiatric patients. The peripheral effects associated with the anticholinergic action of these drugs (e.g., dry mouth, constipation, urinary retention, and blurred vision) are well known and generally obvious to patients and their providers. Anticholinergics also have central effects and depending on the dose and age of the patient can result in sedation and cognitive impairment. Joshi and colleagues (8) previously demonstrated that an individual’s overall anticholinergic burden (ACB) score, calculated by estimating ones’ total amount of anticholinergic exposure from all medications, was associated with cognitive impairment in patients with schizophrenia. This is an important observation that helps to explain the complex factors that contribute to cognitive deficits in patients with schizophrenia and has direct treatment implications. In the current issue of the Journal, Joshi and colleagues extend this work by examining whether ACB scores are also related to alterations in EEG biomarkers of early information processing that occur in individuals with schizophrenia (9). The specific EEG biomarkers used are sequential components of auditory event-related potentials elicited by unexpected background stimuli, i.e., mismatch negativity and P3a. The neurophysiological processes reflected by these markers are fundamental to normal cognitive processing. The data reported in this study was collected from 555 patients and was compared to 1,062 controls. Most of the patients were diagnosed with schizophrenia, with a small number diagnosed with schizoaffective disorder, depressed type. Consistent with the previously reported relation between increased ACB scores and cognitive impairment, the current results demonstrated a negative relation between an individual’s ACB score and the magnitude of their mismatch negativity and P3a EEG responses. When performing regression analyses to include the effects of other factors such as functional and neurocognitive measures, ACB was still found to be associated with the mismatch negativity response, whereas this was not the case for the P3a response. Taken together, these findings point to the importance of accounting for ACB, both clinically and in research studies, when assessing factors related to cognitive impairments in individuals with schizophrenia. In his editorial, Dr. Steven Siegel from the University of Southern California (10) describes in more depth what evoked response potentials are and more specifically discusses the meaning of the findings linking ACB to alterations in the mismatch negativity and the P3a responses.
Conclusion
This issue of the Journal presents articles that cover a broad array of topics and methods, ranging from post-mortem molecular studies in brains from schizophrenia patients to identifying societal issues that are important in determining racial and ethnic disparities in mental health and well-being. The major findings from the papers in this issue include: 1) in older Black, Hispanic/Latinx and White individuals the social determinants of health are associated with marked disparities in depression, cognition, and self-assessments of health, 2) in brains from a subset of individuals with schizophrenia, decreased parvalbumin and somatostatin gene expression occurs within a normal number of dorsolateral prefrontal cortical GABA interneurons, 3) in schizophrenia patients, the anticholinergic burden from all medications that are taken is associated with a reduction in the magnitude of neurophysiological biomarkers that are linked to cognitive processing, and 4) in nondemented individuals, the severity and progression of small cerebrovascular disease can predict the likelihood of developing dementia.
The studies in this issue of the Journal reflect the breadth of our field and illustrate the importance of performing research at different levels of analysis (e.g., molecular, cellular, circuit, individual, societal) to fully understand the complex interactions among risk and resiliency factors that lead to illness and affect treatment outcomes. I particularly want to highlight the works of Alegría et al., Jester et al., and Escobar et al. that focused on characterizing how race- and ethnic-related differences in the social determinants of health are associated with disparities in mental health and well-being. These contributions are especially important for our readership to help understand the origins of the disparities in mental health care experienced by individuals of color and to form a basis for developing strategies to change and mitigate the factors that lead to these biases.
1. : Recent advances on social determinants of mental health: looking fast forward. Am J Psychiatry 2023; 180:473–482 Link, Google Scholar
2. : Differences in social determinants of health underlie racial/ethnic disparities in psychological health and well-being: study of 11,143 older adults. Am J Psychiatry 2023; 180:483–494 Link, Google Scholar
3. : Isolating socioenvironmental correlates of race/ethnicity: a promising strategy to understand and address health disparities. Am J Psychiatry 2023; 180:462–464 Link, Google Scholar
4. : The nature of prefrontal cortical GABA neuron alterations in schizophrenia: markedly lower somatostatin and parvalbumin gene expression without missing neurons. Am J Psychiatry 2023; 180:495–507 Link, Google Scholar
5. : Sutton’s law. Am J Psychiatry 2023; 180:465–466 Link, Google Scholar
6. : Cerebral small vessel disease progression and the risk of dementia: a 14-year follow-up study. Am J Psychiatry 2023; 180:508–518 Link, Google Scholar
7. : Cerebrovascular disease and neuropsychiatric disorders: translating findings from the MRI scanner to the clinic. Am J Psychiatry 2023; 180:467–469 Link, Google Scholar
8. : Anticholinergic medication burden-associated cognitive impairment in schizophrenia. Am J Psychiatry 2021; 178:838–847Link, Google Scholar
9. : Sensitivity of schizophrenia endophenotype biomarkers to anticholinergic medication burden. Am J Psychiatry 2023; 180:519–523 Link, Google Scholar
10. : The power of potentials. Am J Psychiatry 2023; 180:470–472 Link, Google Scholar