Coming of Age?: Neuroimaging Biomarkers in Youth
Diagnosis of psychiatric illnesses is conventionally made by evaluating behavior and subjective report of abnormal experiences to group individuals into illness categories. These categories mask a great deal of heterogeneity, however, particularly in child-onset psychiatric illnesses such as bipolar disorder, an illness that remains notoriously difficult to differentiate from other psychiatric illnesses in youth. In the absence of objective biological markers—"biomarkers"—diagnostic accuracy for psychiatric illnesses therefore remains severely compromised. In this issue of the Journal, Brotman and colleagues (1) provide preliminary evidence that specific neuroimaging measures can help distinguish youth with bipolar disorder from youth with attention deficit hyperactivity disorder (ADHD) and severe mood dysregulation characterized by chronic, nonepisodic presentations of marked irritability and hyperarousal (2). These findings thereby highlight the future promise of neuroimaging to identify biomarkers of psychiatric illnesses in youth.
Put into context, bipolar disorder is a devastating illness that affects up to 5% of the adult population (3). It often has its onset in childhood and adolescence (4). Furthermore, early-onset bipolar disorder may be a particularly severe form of the illness (4, 5). Identifying and treating bipolar disorder as early as possible in youth therefore has huge potential to improve the course of illness. Yet, sometimes this can be extremely difficult using current clinical methods, for two main reasons. First, there is considerable overlap between symptoms of bipolar disorder and symptoms of other psychiatric illnesses (6). Many bipolar disorder symptoms, such as irritability, motor hyperactivity, and sleep problems, overlap with other, more common pediatric psychiatric illnesses, including ADHD. As early-onset bipolar disorder is associated with worse symptom and functional outcomes in adulthood, intervening with effective treatment before the illness can permanently damage long-term outcome is an important public health goal. Misdiagnosing bipolar disorder as ADHD could therefore result in exposure to psychostimulant medications in bipolar youth, without the protective effect of mood stabilizing medications. On the other hand, overdiagnosis of bipolar disorder could lead to inappropriate treatment with mood stabilizers and antipsychotic medications in youth who may have ADHD. Other psychiatric illnesses that might be difficult to differentiate from bipolar disorder, such as conduct disorder, major depressive disorder, or anxiety disorders, may even be effectively treated by psychosocial interventions instead of medications. A second reason for the difficulty in accurately diagnosing bipolar disorder in youth is that many children and adolescents present in community, clinical, and research settings with what appear to be significant manic symptoms but do not meet DSM-IV criteria for bipolar disorder. For these youth, differentiating between bipolar disorder and other illnesses, such as severe mood dysregulation, is extremely difficult.
It is therefore imperative to find objective biomarkers of bipolar disorder to help differentiate youth who will clearly progress to bipolar disorder from the heterogeneous group of youth that present with bipolar disorder as a potential diagnosis but who may instead have ADHD or severe mood dysregulation. Objective biomarkers of psychiatric illnesses, as for general medical illnesses, will necessarily reflect, or be related to, underlying pathophysiologic illness mechanisms (7, 8). Abnormal emotion processing and emotion dysregulation are key clinical features of mood disorders such as bipolar disorder and severe mood dysregulation, and neuroimaging techniques, including functional magnetic resonance imaging, have already been employed to identify abnormalities in key neural circuitry supporting these processes in bipolar disorder (9). While much remains to be understood regarding the mediating role that abnormal neural circuitry may play between the myriad developmental, familial, psychosocial, and environmental factors and subthreshold mood and anxiety symptoms that predispose individuals to psychiatric illnesses such as bipolar disorder, it is becoming clear that neuroimaging techniques have promise for use in the search for objective biomarkers of psychiatric illnesses in youth (Figure 1).
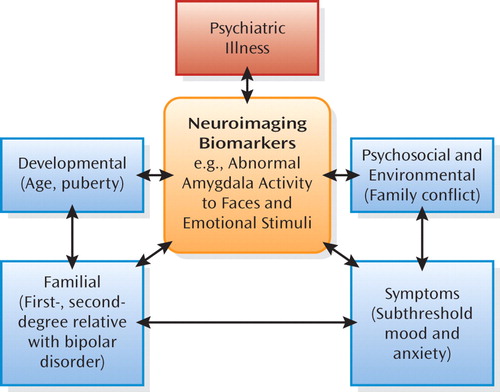
aThe flow chart illustrates the interrelationships between developmental, familial, psychosocial, environmental, and clinical factors that predispose individuals to develop psychiatric illness; the potential role of abnormal neural circuitry in mediating these relationships; and the use of neuroimaging to help identify biomarkers reflecting underlying neural mechanisms associated with the illness.
In a carefully designed study, Brotman and colleagues provide preliminary evidence that youth with "narrow-phenotype" bipolar disorder (with clear episodes of elevated mood and mania symptoms), youth with ADHD without severe mood dysregulation, and youth with severe mood dysregulation can be distinguished by patterns of neural activity to socially (and emotionally) salient stimuli: neutral faces. Recruiting an impressively large number of 127 children and adolescents between the ages of 8 and 17 years, including 43 with bipolar disorder, 18 with ADHD, 29 with severe mood dysregulation, and 37 healthy comparison youth, Brotman and colleagues report, for the first time, that while rating subjective fear in response to viewing neutral faces, youth with ADHD showed left amygdala hyperactivity, whereas youth with severe mood dysregulation showed left amygdala hypoactivity relative to all other groups. This study is important for several reasons. First, the study indicates that neuroimaging measures of relevance to affective disorders, namely amygdala activity during face processing, may help distinguish youth with different psychiatric illnesses. Second, the ecologically valid face processing task employed by the authors measures a key process relevant to understanding psychiatric illness: the subjective experience of threat-related emotions, such as fear, in response to looking at faces of other people. It was mainly during this specific face processing task component that Brotman and colleagues were able to show dissociable patterns of amygdala activity in the different illness groups. Third, while a possible limitation of the study is its focus on one neural region, the amygdala, the pivotal role of the amygdala in emotion and face processing makes it an important region to examine in neuroimaging studies of psychiatric populations. It is encouraging that simple measures of activity in this region can differentiate different psychiatric illness groups, and findings suggest that amygdala activity in response to specific face or emotional stimuli may be a useful neuroimaging measure to include in future studies aiming to identify potential biomarkers of psychiatric illnesses across the lifespan. A recent study has indeed demonstrated that the magnitude of amygdala activity to sad facial expressions differentiates adults with bipolar depression form adults with unipolar depression (10).
The promising findings of Brotman and colleagues indicate that neuroimaging techniques have the potential to be used to help identify biomarkers that may reflect underlying pathophysiologic illness processes to discriminate youth with different psychiatric illnesses, despite the fact that these illnesses are often extremely difficult to differentiate based on clinical evaluation alone. Further studies are clearly needed to elucidate whether functional abnormalities in key neural circuitry in emotion processing and emotion regulation, including not only the amygdala but also other neural regions interconnected with the amygdala, can accurately differentiate between bipolar disorder and other psychiatric illnesses in youth. It will also be critical that prospective validation studies are performed to examine whether neuroimaging measures can help identify which individual vulnerable youth will develop illnesses such as bipolar disorder as opposed to other illnesses in the future. The extent to which neuroimaging has "come of age" as a reliable method to help with diagnosis of psychiatric illnesses remains to be determined. For now, however, it is to be hoped that more studies will take advantage of the promise that the findings of Brotman and colleagues provide for the use of neuroimaging techniques in helping to increase understanding of neural mechanisms mediating vulnerability to future development of psychiatric illnesses across the lifespan.
1 : Amygdala activation during emotion processing of neutral faces in children with severe mood dysregulation versus ADHD or bipolar disorder. Am J Psychiatry 2010; 167:61–69 Link, Google Scholar
2 : Defining clinical phenotypes of juvenile mania. Am J Psychiatry 2003; 160:430–437 Link, Google Scholar
3 : Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2007; 64:543–552 Crossref, Medline, Google Scholar
4 : Long-term implications of early onset in bipolar disorder: data from the first 1,000 participants in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Biol Psychiatry 2004; 55:875–881 Crossref, Medline, Google Scholar
5 : Course and outcome of bipolar spectrum disorder in children and adolescents: a review of the existing literature. Dev Psychopathol 2006; 18:1023–1035 Crossref, Medline, Google Scholar
6 : Treatment guidelines for children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 2005; 44:213–235 Crossref, Medline, Google Scholar
7 : Toward constructing an endophenotype strategy for bipolar disorders. Biol Psychiatry 2006; 60:93–105 Crossref, Medline, Google Scholar
8 : Redefining bipolar disorder: toward DSM-V (editorial). Am J Psychiatry 2006; 163:1135–1136 Link, Google Scholar
9 : A neural model of voluntary and automatic emotion regulation: implications for understanding the pathophysiology and neurodevelopment of bipolar disorder. Mol Psychiatry 2008; 13:829, 833–857 Crossref, Medline, Google Scholar
10 : Elevated amygdala activity to sad facial expressions: a state marker of bipolar but not unipolar depression. Biol Psychiatry (in press) Google Scholar



