Overcrowding in Hospital Wards as a Predictor of Antidepressant Treatment Among Hospital Staff
Abstract
Objective: This report assessed whether hospital ward overcrowding predicts antidepressant use among hospital staff. Method: The extent of hospital ward overcrowding was determined using administrative records of monthly bed occupancy rates between 2000 and 2004 in 203 somatic illness wards in 16 Finnish hospitals providing specialized health care. Information on job contracts for personnel was obtained from the employers’ registers. Comprehensive daily data on purchased antidepressant prescriptions (World Health Organization’s Anatomical Therapeutic Chemical classification code N06A) for nurses (N=6,699) and physicians (N=641) was derived from national registers. Cox proportional hazards models were used to examine the association between bed occupancy rate and subsequent antidepressant treatment. Monthly bed occupancy rates were used as a time-dependent exposure that could change in value over the course of observation. Hazard ratios were adjusted for sex, age, occupation, type and length of employment contract, hospital district, specialty, and calendar year. Results: Exposure over 6 months to an average bed occupancy rate over 10% in excess of the recommended limit was associated with new antidepressant treatment. This association followed a dose-response pattern, with increasing bed occupancy associated with an increasing likelihood of antidepressant use. There was no evidence of reverse causality; antidepressant treatment among employees did not predict subsequent excess bed occupancy. Conclusions: The increased risk of antidepressant use observed in this study suggests that overcrowding in hospital wards may have an adverse effect on the mental health of staff.
In hospitals, overcrowding and excess staff workload have been widely recognized as a serious problem for both patients and staff (1 – 7) . Overcrowding, as indicated by excess bed occupancy, has been shown to be associated with increased hospital infections and patient mortality (3 – 5) . Other reports have found that a high patient to nurse ratio is related to adverse patient outcomes (1 , 6 , 7) and increased self-reports of staff burnout and job dissatisfaction (1) . Furthermore, self-reported excess staff workload appears to be associated with an increased risk of depression (8 – 10) . However, research on the associations between hospital overcrowding and mental health in hospital staff is lacking.
In this report, we present results from a prospective study of 6,699 nurses and 641 physicians from 203 somatic illness wards in 16 Finnish hospitals. Monthly bed occupancy records for each ward over a 5-year period and daily information on antidepressant prescriptions purchased by the staff enabled us to assess the effect of excess occupancy rate on the likelihood of new antidepressant treatment among hospital employees.
Method
Participants
In Finland, specialized hospital care is provided by 21 separate hospital districts. Five of these participated in the Work and Health in Finnish Hospital Personnel Study (11) . The study was coordinated by the Finnish Institute of Occupational Health and approved by its ethics committee.
Data on bed occupancy were collected from 203 somatic illness wards in five city hospitals and 11 regional hospitals between January 2000 and December 2004. Employees who worked on these wards were identified from the employers’ registers. To ensure the study participants were exposed to conditions on the wards for a reasonable length of time, we selected all employees who had at least one 6-month job contract during the study period and less than 2 months absence from work during that time (N=7,509). The ward in which the employee was working was checked every month to ensure that the study participant was assigned the correct bed occupancy exposure. In order to determine prevalence of new-onset antidepressant treatment, we excluded those who were already on treatment at the end of the first 6-month exposure period (N=169). The final cohort consisted of 7,340 participants, of whom 6,699 (91.3%) were registered nurses and licensed practical nurses and 641 (8.7%) were physicians. The mean age of participants was 38.6 years (SD=10.1) and 92% were women.
Procedure
Participating hospitals routinely collected monthly figures on bed occupancy for each ward according to the procedure set by the National Research and Development Centre for Health and Welfare. Bed occupancy was calculated as the ratio between the sum of the number of inpatient days and the number of beds available (i.e., the number of beds multiplied by the number of days the ward was in use) and expressed as a percentage. Days the ward was closed were excluded from the denominator. The day of admission but not the day of discharge for each patient was included in the numerator. The rate above which a hospital ward is considered overcrowded is <100% and is usually defined as >85% (5 , 12 , 13) . Occupancy rates exceeding 85% have been associated with nonoptimal patient outcomes in previous studies (5 , 12) . In this study, ward-level monthly rates of bed occupancy between January 2000 and December 2004 were used. The mean of the bed occupancy rates in excess of 85% across 6 months was used as the exposure measure.
Data on the purchase of prescribed antidepressants for each employee were derived from the prescription register of the Social Insurance Institution of Finland, which comprises outpatient prescription data classified according to the World Health Organization’s Anatomical Therapeutic Chemical classification code (14) . The data included the exact dates of all purchases of antidepressants (code N06A) between Jan. 1, 2000, and Dec. 31, 2004, and the corresponding defined daily dosages. We used defined daily dosages to calculate the maximum length of treatment covered by each purchase. We used a 50-day washout period to define a new treatment (i.e., at least 50 days of nontreatment, calculated from the maximum length of treatment afforded by the latest purchase of antidepressants, if any). The main outcome in this study was the beginning of a new period of antidepressant treatment after the assessment of exposure to excess bed occupancy. The overall mean bed occupancy rate among the wards over time was 78.2% (range=26.1%–142.5%, SD=13.6). The mean follow-up time to antidepressant treatment was 29.8 months (SD=18.9).
From the employers’ registers we obtained sex, age, occupation (nurse versus physician), type of employment contract (temporary versus permanent), length of present employment contract, hospital district, specialty, and calendar year to include in the analyses as potential confounding factors (15 , 16) .
Statistical Analyses
We used Cox proportional hazards models to examine the associations between excess bed occupancy and employee antidepressant treatment. We constructed a measure of excess occupancy, with bed occupancy ≤85% coded as 0% and bed occupancy >85% coded as the percent occupancy minus 85%. Monthly excess bed occupancy rates were considered time-dependent exposures that could change in value over the period of observation (17) . In the Cox model, a time-dependent exposure is treated in a manner similar to a time-dependent covariate. Employees were followed until either the start of the first new antidepressant treatment, the end of their employment on a participating ward, or Dec. 31, 2004, whichever came first. After the first 6 months of follow-up, each subsequent month of follow-up contributed data to one of the outcome categories: new antidepressant event or no event. For each employee, only the 6-month period that immediately preceded an event defined the exposure category for the event. All previous 6-month exposure periods for that employee, as well as all 6-month exposure periods for employees with no event, contributed data to the exposure categories associated with no event. These data were assigned to exposure categories according to the mean of the monthly excess bed occupancy rates over the preceding 6 months. Hazard ratios and their 95% confidence intervals were adjusted for all measured potential confounding factors.
As there is usually a time lag between a person feeling depressed and that person seeking treatment (18 – 20) , we would expect that exposure to excess bed occupancy would also predict antidepressant treatment several months after the end of the exposure period—that is, after an intervening period of untreated depression. We tested this by introducing a 6-month and a 12-month lag period into our basic study design. The present study could also have been subject to reverse causality if depression among the employees was to contribute substantially to the overcrowding of the hospital wards (21 , 22) . In principle, this could occur if the impact of depression on the productivity of affected individuals (23) resulted in failure to discharge patients in a timely manner. We tested the potential for reverse causality in a subpopulation previously unexposed to excess bed occupancy by examining whether new antidepressant use during the preceding month predicted excess bed occupancy in the next month. Null findings in these analyses would provide evidence against the reverse causality hypothesis. All analyses were conducted using the SAS Version 9.1.3 statistical software (SAS Institute, Cary, N.C.).
Results
Demographic characteristics of employees at the beginning of the follow-up period are presented in Table 1 . The majority of participants (91%) were nurses and 69% had a permanent job contract. At the beginning of the follow-up period, 40% of participants were working in a ward with no excess bed occupancy, 35% in wards with an excess bed occupancy of ≤5%, 15% in wards with an excess bed occupancy of >5% to ≤10%, and 10% in a ward with an excess bed occupancy of >10%. Variation in bed occupancy was found between hospital districts, and excess bed occupancy was more common in internal medicine than in surgical wards and other specialties. Short job contracts were more common in groups with high bed occupancy.
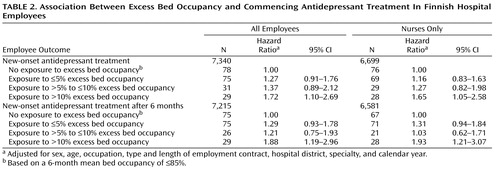
Table 2 shows the association between the mean level of bed occupancy during a 6-month period and subsequent antidepressant treatment. After adjustment for potential confounding factors, excess bed occupancy of >10% was found to be related to a 1.7-fold increase in risk of new antidepressant treatment. A similar effect (hazard ratio=1.7) was found in the analysis for nurses alone ( Figure 1 ). The association followed a dose-response pattern for a continuous measure of bed occupancy rate (all employees: p=0.013; nurses only: p=0.031). The time-dependent interaction between bed occupancy rate and the follow-up period was nonsignificant (p=0.145); thus there was no evidence that the association would have changed over time.

The effects of overcrowding after a 6-month time lag (i.e., after a period of potential untreated depression subsequent to exposure) are also shown in Table 2 . These analyses reveal a similar or even slightly stronger effect of ward overcrowding (all employees: hazard ratio=1.9; nurses only: hazard ratio=1.9). As a test of sensitivity, we repeated these analyses using a 12-month rather than a 6-month time lag. The effect of ward overcrowding was diluted with this extended time period (all employees: hazard ratio=0.91, 95% CI=0.55–1.51; nurses only: hazard ratio=0.97, 95% CI=0.59–1.61; results not shown).
Table 3 shows a test of reverse causality—that is, whether antidepressant use in the preceding month predicts overcrowding in the next month among employees previously not exposed to overcrowding. The results suggest that this is not the case.
Discussion
Our results indicate that ward overcrowding, expressed as excess bed occupancy, predicts new periods of antidepressant use among hospital nurses and physicians. We also found that the relationship between excess bed occupancy and antidepressant use followed a dose-response pattern. Direct comparison with earlier studies is not possible because our study is unique in many respects. For instance, in this study bed occupancy rate was assessed each month over a 5-year period, which has not been previously feasible. Furthermore, this study had daily data on employees’ antidepressant purchases.
The reason overcrowding may affect the mental health of employees is related to its association with high workload. Overcrowding will increase workload, for example, if an insufficient number of employees is available to cover patient peaks. Workload may increase even if agency staff are used to help cover it, as a certain level of mentoring will be involved. Overcrowding is also related to poor patient outcomes (3 – 5) , which implies that patients are sicker and have increased needs. It is also noteworthy that associations between high patient to nurse ratios and burnout among hospital nurses (1) and between self-reported high job demands and incidence of depressive disorders and antidepressant use have been reported (8 – 10) .
Antidepressant medication can be considered as a proxy measure for clinically significant depressive or anxiety disorders. However, many affected individuals wait long periods after a depressive episode begins before initiating pharmacologic treatments. With a 6-month time lag we replicated the robust association between overcrowding in the ward and subsequent antidepressant use. Earlier studies, which focused on the first episode of depression rather than new-onset depression, found a large variation in the time lag between the onset of depression and seeking help, ranging from 4 months (18) to several years (19 , 20) .
At the individual level, depression is associated with diminished productivity and might therefore contribute to a failure to discharge patients in a timely manner, a potential source of ward overcrowding. To address this possibility of reverse causality between occupancy rate and depression, we tested whether antidepressant use predicted overcrowding in a subpopulation previously unexposed to excess bed occupancy. These analyses provided no evidence to support reverse causation as an explanation for the association between ward overcrowding and antidepressant use.
Some limitations of our study are noteworthy. First, selection of variables included in the analysis was dependent on the availability of data in source registers. This meant that some variables of interest, such as marital status and adverse events outside work, were not available to this study (24 , 25) . Register data on antidepressant prescriptions are based on a visit to the physician and cover virtually all outpatient prescriptions in Finland. Lack of information on the diagnosis for which antidepressants were prescribed made it impossible for us to exclude those prescriptions that were for indications other than mental disorders, such as chronic pain or sleeping problems.
Furthermore, as our measure of depression was antidepressant treatment, we were not able to take account of employees with unrecognized or untreated depression or those treated using nonpharmacological methods. Thus, we cannot fully eliminate the possibility of reverse causality arising from a protopathic bias (21 , 22) if reduced productivity among employees with untreated depression substantially influenced ward-level overcrowding. Moreover, differences in treatment practice among physicians may also affect the choice of treatment (i.e., whether or not to prescribe antidepressants). However, such variability is likely to be random in relation to bed occupancy and is probably not a source of major bias in our results.
The possibility of unmeasured confounding can never be totally ruled out in observational studies such as ours. However, adjustment for sex, age, occupational group, and type of employment contract allowed us to control for confounding by these risk factors for depression (15 , 16) . Adjustment for hospital district enabled us, to some extent, to control for area differences in the prevalence of depression and variation in organizational structure and occupational health service practices between hospital districts. Further adjustment for specialty allowed us to partially control for variation in organizational factors between specialties, and by adjusting for calendar year we sought to control for period effects on antidepressant use.
Finally, our cohort was from public sector hospitals and was 92% female and ethnically homogeneous (mostly white employees). Future research with more diverse samples is needed to evaluate the generalizability of our findings.
With the limitations of our study in mind, we conclude that overcrowding in hospital wards may have an adverse effect on the mental health of employees. Our findings have important implications for hospital administration. Depression is a serious problem worldwide in terms of human suffering, disability, mortality, and productivity (23 , 26) . Overcrowding may not only be a consequence of lack of resources but also a byproduct of patient flow problems (27) . As depression is a major cause of work disability, our findings suggest that minimizing overcrowding in hospital wards would not only be beneficial to patients but should also be regarded as a target worthy of priority in the promotion of mental health and working capacity among hospital staff.
1. Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH: Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA 2002; 288:1987–1993Google Scholar
2. Aiken LH, Clarke SP, Sloane DM, Sochalski JA, Busse R, Clarke H, Giovannetti P, Hunt J, Rafferty AM, Shamian J: Nurses’ reports on hospital care in five countries. Health Aff (Millwood) 2001; 20:43–53Google Scholar
3. Cunningham JB, Kernohan WG, Rush T: Bed occupancy, turnover intervals and MRSA rates in English hospitals. Br J Nurs 2006; 15:656–660Google Scholar
4. Tarnow-Mordi WO, Hau C, Warden A, Shearer AJ: Hospital mortality in relation to staff workload: a 4-year study in an adult intensive-care unit. Lancet 2000; 356:185–189Google Scholar
5. Sprivulis PC, Da Silva JA, Jacobs IG, Frazer AR, Jelinek GA: The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust 2006; 184:208–212Google Scholar
6. Hugonnet S, Harbarth S, Sax H, Duncan RA, Pittet D: Nursing resources: a major determinant of nosocomial infection? Curr Opin Inf Dis 2004; 17:329–333Google Scholar
7. Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K: Nurse-staffing levels and the quality of care in hospitals. N Engl J Med 2002; 346:1715–1722Google Scholar
8. Stansfeld S, Candy B: Psychosocial work environment and mental health—a meta-analysis. Scand J Work Environ Health 2006; 32:443–462Google Scholar
9. Plaisier I, de Bruijn JG, de Graaf R, ten Have M, Beekman AT, Penninx BW: The contribution of working conditions and social support to the onset of depressive and anxiety disorders among male and female employees. Soc Sci Med 2007; 64:401–410Google Scholar
10. Virtanen M, Honkonen T, Kivimäki M, Ahola K, Vahtera J, Aromaa A, Lönnqvist J: Work stress, mental health and antidepressant medication: findings from the Health 2000 Study. J Affect Disord 2007; 98:189–197Google Scholar
11. Kivimäki M, Elovainio M, Vahtera J, Virtanen M, Stansfeld SA: Association between organizational inequity and incidence of psychiatric disorders in female employees. Psychol Med 2003; 33:319–326Google Scholar
12. U.K. Department of Health: Shaping the Future NHS: Long Term Planning for Hospitals and Related Services: Consultation Document on the Findings of the National Beds Inquiry. London, U.K. Department of Health, 2000Google Scholar
13. Bagust A, Place M, Posnett JW: Dynamics of bed use accommodating emergency admissions: stochastic simulation model. BMJ 1999; 319:155–158Google Scholar
14. WHO Collaborating Centre for Drug Statistics Methodology: Guidelines for ATC Classification and DDD Assignment, 2004. Oslo, World Health Organization Collaborating Centre for Drug Statistics, 2004Google Scholar
15. Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M: Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol 2003; 157:98–112Google Scholar
16. Virtanen M, Kivimäki M, Ferrie JE, Elovainio M, Honkonen T, Pentti J, Klaukka T, Vahtera J: Temporary employment and antidepressant medication: a register linkage study. J Psychiatr Res 2008; 42:221–229Google Scholar
17. Allison PD: Survival Analysis Using the SAS System: A Practical Guide, 2nd ed. Cary, NC, SAS Institute, 1995Google Scholar
18. Gormley N, O’Leary D, Costello F: First admissions for depression: is the “no-treatment interval” a critical predictor of time to remission? J Affect Disord 1999; 54:49–54Google Scholar
19. Kessler RC, Olfson M, Berglund PA: Patterns and predictors of treatment contact after first onset of psychiatric disorders. Am J Psychiatry 1998; 155:62–69Google Scholar
20. Wang PS, Angermeyer M, Borges G, Bruffaerts R, Tat Chiu W, De Girolamo G, Fayyad J, Gureje O, Haro JM, Huang Y, Kessler RC, Kovess V, Levinson D, Nakane Y, Oakley Brown MA, Ormel JH, Posada-Villa J, Aguilar-Gaxiola S, Alonso J, Lee S, Heeringa S, Pennell BE, Chatterji S, Ustün TB: Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry 2007; 6:177–185Google Scholar
21. Horwitz RI, Feinstein AR: The problem of “protopathic bias” in case-control studies. Am J Med 1980; 68:255–258Google Scholar
22. Delgado-Rodriguez M, Llorca J: Bias. J Epidemiol Community Health 2004; 58:635–641Google Scholar
23. Wang PS, Beck AL, Berglund P, McKenas DK, Pronk NP, Simon GE, Kessler RC: Effects of major depression on moment-in-time work performance. Am J Psychiatry 2004; 161:1885–1891Google Scholar
24. Kendler KS, Gardner CO, Prescott CA: Toward a comprehensive developmental model for major depression in women. Am J Psychiatry 2002; 159:1133–1145Google Scholar
25. Kendler KS, Gardner CO, Prescott CA: Toward a comprehensive developmental model for major depression in men. Am J Psychiatry 2006; 163:115–124Google Scholar
26. Murray CJ, Lopez AD: Global mortality, disability, and the contribution of risk factors: global burden of disease. Lancet 1997; 349:1436–1442Google Scholar
27. Simmons FM: Hospital overcrowding: an opportunity for case managers. Case Manager 2005; 16:52–54Google Scholar