Delayed-Onset Posttraumatic Stress Disorder: A Systematic Review of the Evidence
Abstract
Objective: Since the diagnosis of delayed-onset posttraumatic stress disorder (PTSD) was introduced in DSM-III, there has been controversy over its prevalence and even its existence. The authors sought to resolve discrepant findings concerning the prevalence of delayed-onset PTSD by conducting a systematic review of the evidence. Method: A literature search was conducted for case reports and group studies with adequate measurement of delayed-onset PTSD according to DSM criteria. Studies that met inclusion criteria were examined for the defined length of delay for delayed-onset PTSD, presence of symptoms before full diagnostic criteria were met, length of follow-up, prevalence estimates, and other variables. Studies were also examined for differences between immediate-onset PTSD, delayed-onset PTSD, and no-PTSD cases. Results: Ten case studies and 19 group studies met criteria for inclusion in the review. Studies consistently showed that delayed-onset PTSD in the absence of any prior symptoms was rare, whereas delayed onsets that represented exacerbations or reactivations of prior symptoms accounted on average for 38.2% and 15.3%, respectively, of military and civilian cases of PTSD. Conclusions: The discrepant findings in the literature concerning prevalence can be largely, but not completely, explained as being due to definitional issues. Little is known about what distinguishes the delayed-onset and immediate-onset forms of the disorder. Continuing scientific study of delayed-onset PTSD would benefit if future editions of DSM were to adopt a definition that explicitly accepts the likelihood of at least some prior symptoms.
The delayed-onset subtype of posttraumatic stress disorder (PTSD) was formally described in 1980 when PTSD was first recognized as a diagnostic entity in DSM-III. Its inclusion in DSM was based on existing literature indicating that many soldiers do not develop symptoms until they return home, as stress reactions are not adaptive in combat (1) . Since then, numerous studies have investigated the condition in samples of combat veterans and civilians, with no consensus emerging as to its prevalence. Reported rates have varied between 0% and 68% of PTSD cases, and some authors have even expressed skepticism about whether the condition exists at all (2 , 3) . In this article, anticipating the possible revision of the PTSD entry in DSM-V, we attempt to resolve these conflicting findings through a systematic review of the evidence from both case and group studies. We also examine evidence for triggers to onset from the case reports and review the evidence for initial differences between individuals with delayed-onset, acute-onset, and no PTSD from the group studies. The wide variety of research designs and definitions of delayed onset in the literature precludes the use of formal meta-analytic techniques.
DSM-IV-TR describes delayed onset as a specifier for PTSD indicating “that at least 6 months have passed between the traumatic event and the onset of the symptoms” (p. 465). This criterion has remained consistent in all editions since its introduction in DSM-III. It is also specifically noted that PTSD symptom onset usually occurs within 3 months after the trauma, indicating that delayed onset is the exception to the rule. The inclusion of delayed-onset PTSD in DSM-III led to its acceptance as a potentially compensable disorder by the U.S. Veterans Administration (VA), which in turn led to a rise in benefit claims for the disorder, presumably by veterans previously denied the opportunity (4) . Within 2 years of the publication of DSM-III, Atkinson et al. (4) cautioned against accepting all claims of delayed onset as genuine because of the secondary gains involved. In this context, Sparr and Pankratz (5) reported five cases of factitious PTSD among men presenting at a VA medical center claiming to be Vietnam veterans.
Before summarizing the literature, we discuss sources of variation in definition, design, and assessment that have a bearing on inclusion criteria for studies in our review and evaluation of the evidence. Starting with definition, one of the main stumbling blocks concerns ambiguity in the criterion for delayed onset in DSM. There is no clarification of whether “the onset of the symptoms” refers to any symptoms that might eventually lead to the disorder or only to full-blown PTSD itself. In the former interpretation (which we term definition 1), an individual with minimal initial symptoms that gradually worsened until full PTSD criteria were met after a substantial period would not be classified as having delayed-onset PTSD. Given that it is common for trauma-exposed individuals to develop at least some symptoms in the short term (6 , 7) , definition 1 delayed-onset PTSD should be relatively uncommon if it exists at all. Alternatively, defining delayed onset as relating to the full disorder (which we term definition 2) means that, in theory, the onset of just one additional symptom in an already highly symptomatic individual could be sufficient for a diagnosis of delayed-onset PTSD. Definition 2 delayed-onset PTSD should be relatively more common, which therefore leads to the prediction that the definition adopted will have a major impact on the estimated prevalence of the condition.
Only two prospective studies investigating delayed-onset PTSD explicitly interpret the DSM definition as ruling out any prior symptoms (2 , 3) , although both provide data on delayed onset of full PTSD with prior symptoms. There are, however, some retrospective studies in which it is unclear how the definition has been interpreted (e.g., reference 8 ). Given this lack of clarity in the formal definition and in most research studies, we did not exclude studies from our review that permitted delayed-onset PTSD cases to include some prior symptoms. Nevertheless, evidence in any way suggestive of a prior episode meeting full criteria for PTSD, or insufficient information to rule this out, was taken into account in the selection of case reports.
Another definitional issue concerns the length of the delay between trauma exposure and onset of symptoms. A number of studies have not adhered to the specified delay of at least 6 months in their research design but have investigated a shorter period. We have excluded these from our review. Other studies have specified onset delays of 12 months or more, and we included these in the review as a separate category.
Retrospective studies of delayed-onset PTSD typically assess lifetime episodes with standardized clinical interviews to track the onset and offset of posttrauma symptoms over time. One disadvantage of this method is the problem of memory reliability, particularly when a long time has elapsed between trauma and interview. Thus, a growing number of researchers have conducted prospective studies using clinical interviews, questionnaires, or a combination of the two at predetermined assessment points. This method also has its disadvantages, as individuals may have had onsets of PTSD after one assessment that then remitted before the next. If, as has often been the case, there has been no retrospective assessment between time points, estimates of delayed-onset PTSD may be unreliable; if these undetected remitted onsets occurred within 6 months after trauma exposure, an overestimate is likely, whereas if they occurred more than 6 months after exposure, an underestimate is likely.
To summarize data on the prevalence of delayed-onset PTSD, it is crucial to be able to use the same metric when comparing rates between studies. Three different ways of expressing frequency are apparent in the literature. The first is as a proportion of all respondents, the second as a proportion of all respondents with no prior (acute) PTSD, and the third as a proportion of all respondents with PTSD. Estimates using the first two calculations appear to be the most favored, but they are dependent on the overall rate of PTSD in the study sample. Because PTSD rates vary considerably according to the characteristics of the sample and the type of trauma experienced (9) , estimates based on these two calculations cannot be used to make valid comparisons. For review purposes, the optimal way to express the rate of delayed-onset PTSD is as a proportion of all those with PTSD.
The purpose of this review is to resolve the uncertainty about how to interpret existing data on delayed-onset PTSD. We use rigorous selection criteria to identify the case reports and group studies that can tell us the most about the existence, prevalence, and characteristics of delayed-onset PTSD. Case studies are uniquely valuable in establishing whether a condition exists and in generating hypotheses about its causes and characteristics. Group studies yield less detailed information but provide a basis for making prevalence estimates and comparisons between immediate-onset PTSD, delayed-onset PTSD, and no-PTSD cases.
Method
Selection of Articles
English-language articles published since 1980 that included data on delayed-onset PTSD (defined in a way consistent with DSM-III, DSM-III-R, or DSM-IV) were located in bibliographic databases, recent journal issues, and secondary sources, such as journal articles and book chapters. The Social Science Citation Index, PsycINFO, PubMed, and the PILOTS database managed by the National Center for PTSD were searched using the terms PTSD or posttraumatic stress disorder and delayed onset (with and without the hyphen) or delay. In another search the terms longitudinal and prospective were used with PTSD or posttraumatic stress disorder.
Articles describing group studies were included if they met the following criteria: 1) delayed onset referred to syndromal (i.e., meeting full DSM criteria) or subsyndromal PTSD rather than nonspecific symptoms or behaviors, such as help seeking; 2) the study included a valid PTSD assessment, such as a diagnostic interview, a questionnaire with all PTSD criteria symptoms included and a valid designated diagnostic cutoff score, or a retrospective assessment of case records as long as PTSD was the explicit focus when the case record was taken; 3) delayed onset of symptoms could be assessed as occurring more than 6 months after trauma exposure; 4) time to onset was measured from the time of a specific trauma exposure or the end of a potential exposure, such as the end of deployment to a war zone; 5) the study included a clinical, community, military, or specific trauma sample (e.g., motor vehicle accident survivors); and 6) the study sample did not comprise a special population, such as litigants or delayed help-seekers.
For articles describing case studies, we had two inclusion criteria: 1) because it was uncommon for standardized diagnostic interviews to have been used, we required explicit mention that a formal PTSD diagnosis was made using DSM criteria; 2) the study had to provide clear information to establish onset of full PTSD for the first time more than 6 months after the trauma; earlier symptoms suggestive of full PTSD were explicitly ruled out.
The search yielded 74 relevant studies, of which 39% met our inclusion criteria. Of 31 case studies, 10 met inclusion criteria. Of the 21 that did not, 16 did not report a formal PTSD diagnosis, seven reported evidence indicative of a reactivation of an immediate posttrauma condition, and seven did not provide sufficient information to rule this out (numbers sum to more than 21 because of overlapping categories). Of the 43 group studies, 19 met inclusion criteria. The cohort of prisoners of war used in Engdahl et al. (10) , which was included, was also used in Speed et al. (11) and Kluznik et al. (8) , which were excluded because of overlap. Of the 22 other excluded studies, eight did not include a valid PTSD assessment to detect delayed onset, 12 included onsets with a delay of less than 6 months after the trauma, and two described special populations. Authors of group studies were contacted for clarification of assessment procedures when we thought it useful.
Results
Case Studies
Of the 10 studies that met inclusion criteria for review (12 – 21) , seven reported delayed-onset PTSD in relation to war experiences (14 – 17 , 19 – 21) and three in relation to motor vehicle accidents (12 , 13 , 18) . Four of the studies used DSM-IV diagnostic criteria, which include clinically significant distress or impairment in social, occupational, or important areas of functioning (criterion F). Close inspection of the text indicated clear evidence of impairment in all studies, including the six that used earlier versions of DSM in which the diagnostic criteria did not require impairment. Overall, the war experience articles described 23 cases, with 15 accounted for by one article (20) . With one exception (21) , the cases were of elderly veterans of World War II or the Korean War (age range=63–86 years) with PTSD onsets delayed by at least 30 years. The young soldier described by Solomon et al. (21) had an onset around 12 months after his tour of duty. In contrast, all four patients described in the articles on motor vehicle accident trauma were younger (age range=23–45 years) and had onset delays ranging from 10 months to 4 years. The most convincing evidence for delayed-onset PTSD was from three motor vehicle accident victims who were under continuing medical care for their physical injuries prior to onset, making detection of symptoms in the posttrauma period more likely if present (12 , 13) . In the six studies describing elderly war veterans with very long intervals to first onset, 18 of the 22 cases were corroborated by someone else, in most cases a relative and usually the spouse (15 , 19 , 20) . Given the age of the veterans, this does not rule out the possibility of episodes in the early months or years posttrauma that might have gone undisclosed or been forgotten, a limitation noted in two studies (20 , 15) . The corroborative evidence suggests at least that the veterans in question had long relatively symptom-free periods before onset in old age.
All the case studies reported events or circumstances that could have triggered onset. More than half of the cases (15/27) were attributed to an onset of a physical illness in the elderly veterans (14 – 16 , 20) . With one exception (16) , all were neurological illnesses or conditions that may affect cognition. In nearly a quarter of the cases (6/27), the triggers described were reminders of the original trauma (12 , 14 , 17 , 18 ). Two examples were a subsequent near-miss accident experienced by a motor vehicle accident victim (12) and a severe head injury to the son of a veteran who had himself sustained a head injury as part of his traumatic experiences (14) . Details of these studies are included in a supplemental table in the data supplement accompanying the online version of this article.
Group Studies
In 13 of the 19 group studies, delayed onset could be defined as at least 6 months after trauma exposure. Four of these (22 – 25) yielded data on the proportion of respondents for whom no posttraumatic symptoms at all were observed in this period (corresponding to definition 1 of delayed-onset PTSD above), whereas the other nine studies reported the proportion of people who met full criteria for PTSD only after this period (corresponding to definition 2 above). In the remaining six studies, delayed onset of full PTSD could be defined as 1 year or more after trauma exposure (also corresponding to definition 2). It is notable that only two of the 19 studies (26 , 27) used DSM-IV, which includes criterion F—clinically significant distress/impairment—and both studies appear to have assessed it, although this was not explicitly stated. Studies using earlier editions of DSM were not required to assess criterion F, and none reported any relevant data.
Of the four studies that provide evidence relevant to definition 1 ( Table 1 ), two report the number of respondents with full PTSD (23 , 24) , and two report the numbers of respondents with both syndromal or subsyndromal PTSD after 6 months (24 , 25) . Of all the group studies reviewed, these were the only ones to include subsyndromal cases. In the Prigerson et al. study (25) , 37 of the 172 PTSD cases (22%) were subsyndromal. The majority met all DSM-III-R symptom cluster criteria but did not meet the symptom duration criterion (Maciejewski, personal communication, 2006). In the Helzer et al. study (24) , PTSD was rare, and nearly all (94%) of the 422 cases were subsyndromal, defined as having any PTSD symptoms. All of these studies are distinguished from other group studies reviewed inasmuch as they are epidemiological investigations of a variety of traumas with varying lengths of time between trauma and assessment. Given that all used retrospective interviews, it was assumed that earlier, now remitted onsets were taken into account in the assessment. Helzer et al. (24) and Prigerson et al. (25) reported higher rates of delayed symptom onset in combat trauma than in civilian traumas. In the Helzer et al. study, there were no delayed symptom onsets among those with civilian traumas. In two studies, Breslau and colleagues (22 , 23) similarly found minimal or no evidence of delayed onset in studies of young mothers and of adults too young to have been Vietnam conscripts.
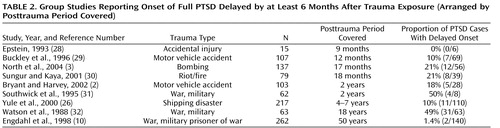
Table 2 presents details of the nine studies (2 , 3 , 10 , 26 , 28 – 32) in which onset of full PTSD was delayed by at least 6 months. Studies are arranged by the length of the period covered after trauma exposure, which ranged from 9 months to 50 years. Six were longitudinal and the three with the longest assessment periods were retrospective in design. With one exception (31) , all used clinical interviews to assess PTSD. We looked for factors that might affect the rates of delayed-onset PTSD, the first being the length of the posttrauma assessment period, on the assumption that the longer the period assessed beyond the first 6 months, the more opportunity there would be for respondents to develop delayed-onset PTSD. Table 2 shows that with two exceptions (10 , 26) , the pattern of delayed onset rates broadly fitted our assumptions. The study with the shortest period covered, 9 months (28) , found no onsets delayed by more than 6 months. It should be noted that the Yule et al. study (26) differed from the others in that the respondents were schoolchildren at the time of the trauma. Also notable is that two of the three studies with military samples reported similar delayed-onset rates that were much higher than the civilian studies (31 , 32) despite differences in study design and duration. However, the Engdahl et al. retrospective investigation (10) of veterans who were all prisoners of war is inconsistent with this pattern. These authors found only two cases of delayed onset in 140 PTSD cases.
Another factor considered was whether the studies assessed whether respondents could have had onsets of PTSD that then remitted before the next assessment point. As noted, lack of such an assessment could lead to both over- and underestimates of delayed-onset rates. We investigated whether the studies assessed remitted onsets between time points as well as whether earlier episodes of PTSD within 6 months of the trauma could be ruled out. Three of the longitudinal studies were negative on both counts (2 , 30 , 31) , but this did not appear to affect the delayed-onset rates relative to the other studies that had included these assessments. For example, both North et al. (3) and Sungur and Kaya (30) , with similar study durations, reported delayed-onset rates of 21%, although only the former assessed symptoms between time points. One possible explanation is that the under- and overestimates that might be a consequence of assessment omissions cancel each other out.
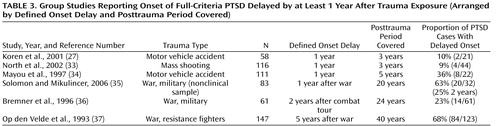
Table 3 lists the six studies (27 , 33 – 37) in the final category, in which onset of full PTSD was delayed by at least 1 year after trauma exposure. Four of these studies were longitudinal, and these all defined delayed onset as 1 year after trauma exposure (27 , 33 – 35) . The remaining two studies were retrospective and defined onset delay as 2 years (36) or 5 years after trauma exposure (37) . The posttrauma period covered ranged from 3 years to 40 years in the six studies. Three studies were of war-related trauma and included two military samples (35 , 36) and a sample of resistance fighters (37) . The other three involved motor vehicle accidents (27 , 34) and a mass shooting (33) . As with the studies listed in Table 2 , it was expected that the longer the posttrauma period covered, the higher the delayed-onset rate would be. However, this trend might be moderated by the defined posttrauma delay: the longer the delay, the lower the likelihood that delayed onsets would develop subsequently.
The four longitudinal studies with delayed onset defined as 1 year after trauma exposure confirmed the pattern found in the 6-month delayed-onset studies—the longer the period covered, the higher the rate of delayed onsets. The two studies covering a 3-year period after trauma exposure (27 , 33) had similar delayed-onset rates despite the fact that prior episodes were not ruled out in one of the studies (27) . Solomon and Mikulincer (35) , with the longest period covered (20 years) of the four studies defining delay as at least 1 year, reported a particularly high rate of 63% in Israeli combat veterans assessed as having no combat stress reaction during the 1982 Lebanon war. This study is of particular interest, as it had four assessment points, at 1, 2, 3, and 20 years, and reported delayed-onset rates at each time point. The study showed that the majority of delayed onsets (12 of 20) occurred in the relatively brief interval between 1 and 2 years after exposure. It was possible to compare this study with the Bremner et al. investigation (36) of U.S. war veterans, which used a retrospective interview to cover a similar period and had delayed onset defined as 2 years after exposure. As shown in Table 3 , the 2-year rates of delayed onset, expressed as a proportion of all PTSD cases, were remarkably similar (25% and 23%).
The last study in this category is that of Op den Velde et al. (37) , who reported that about two-thirds of all PTSD cases in their sample of Dutch World War II resistance fighters were delayed by as much as 5 years. This investigation used a retrospective clinical interview. The authors distinguished PTSD onsets that gradually developed from an earlier subsyndromal condition from delayed PTSD in which the first symptoms did not appear until at least 5 years after the war. It is of interest to contrast the delayed-onset rate in all PTSD cases in this study (84 of 123, or 68%) with that of Engdahl et al. (10) (2 of 140, or 1.4%; see Table 2 ), as both involved male combatants and used retrospective interviews to cover 40 years or more after trauma exposure (the longest posttrauma periods in the studies reviewed). The reason for the discrepancy is unclear. It cannot be explained by the element of captivity, as over half of the resistance fighters had been in concentration camps.
To summarize the frequency of delayed-onset PTSD for the six military and nine civilian studies in Tables 2 and 3 , we calculated the mean rates, weighting for sample size, length of delay, and length of follow-up period. The weighted means were 38.2% and 15.3%, respectively, for military and civilian studies. These were similar to the unweighted means (42.4% and 15%, respectively). Considering these 15 studies overall, eight reported information on prior symptoms, and in six of these, all cases of delayed onset had prior symptoms (information for reference 10 supplied by personal communication with first author, 2006). However, none of these studies systematically reported information to indicate how many symptoms were involved in the transition to full syndromal criteria.
Supplementary details of all 19 studies described in this section, including mean age, gender, and assessment, are available in a data supplement accompanying the online version of this article.
Evidence for Differences Between Groups With Delayed-Onset, Acute-Onset, and No PTSD
We examined the studies reviewed to identify those that had conducted systematic group comparisons, and we found three. The retrospective study by Watson et al. (32) on combat veterans found no significant differences between 32 acute and 31 delayed-onset cases on current symptom profiles or measures of current repression or life stress. However, all respondents had current PTSD. The two longitudinal studies of civilian trauma did not always compare the same groups, and numbers in the delayed-onset groups were very small (five and seven), making interpretation of nonsignificant differences questionable (2 , 29) . Both studies compared groups on at least some initial posttrauma PTSD symptom clusters, heart rate, and psychiatric history. Bryant and Harvey (2) compared delayed-onset cases with both acute cases and subjects without PTSD. The purpose of the study by Buckley et al. (29) was primarily to compare initially symptomatic delayed-onset cases with symptomatic trauma victims who did not develop PTSD. The only symptom cluster assessed in both studies was avoidance symptoms, and the only group comparison they had in common was between delayed-onset and no-PTSD groups. Neither study found differences between delayed-onset and no-PTSD groups on prior psychiatric history. However, Buckley et al. found a significant group difference on PTSD avoidance symptoms but no group difference on initial heart rate, the reverse of what Bryant and Harvey (2) found. Given the small numbers with delayed-onset PTSD, no further description of individual findings is warranted.
Discussion
The majority of the relevant studies did not adhere to DSM criteria in the assessment and diagnosis of delayed-onset PTSD, even though a number of them have been widely cited as evidence for the condition. This is likely to have hindered the field coming to reliable conclusions about delayed-onset PTSD. The evidence from studies that adhered to DSM criteria clearly indicates that definitional issues are critical in resolving the controversies about the existence of delayed-onset PTSD. If the most conservative definition is taken, namely, that the onset of any PTSD symptom is delayed by at least 6 months (definition 1), delayed-onset PTSD appears to be extremely rare outside of military samples. Even in these samples there is disagreement about whether it exists to any appreciable extent, and the higher prevalence estimates have been found only in large-scale surveys, where detailed questioning is unlikely to have been possible. If delayed-onset PTSD is defined this way, the scope for any scientific research will be very limited.
There is, on the other hand, no reason for skepticism concerning the existence of delayed-onset PTSD when the more inclusive definition 2 is used. This type of delayed-onset PTSD accounts for well over a third of PTSD cases in military samples and 15% of cases in civilian samples, according to our estimates. Prevalence seems to be affected, as might be expected, by the length of delay specified prior to onset and the length of the follow-up period, but adjusting for both these variables as well as sample size does not greatly alter the prevalence rates in existing studies. Likewise, longitudinal studies yield similar prevalence estimates whether or not remitted onsets between assessments are investigated. From the studies that included relevant information, we can conclude that this type of delayed-onset PTSD is preceded by prior symptoms in the great majority of cases. Little information is available on the level of these prior symptoms, but case reports are consistent in indicating that sudden sharp increases in the number and severity of symptoms are possible.
The accompanying Patient Perspective presents a description of this type of typical delayed onset. It is a composite we created from individual war veterans we studied who reported delayed-onset PTSD. The phenomenon is sufficiently common to pose important questions about the mechanisms that can explain why in some individuals initial symptoms are not followed by normal recovery but remain vulnerable to reactivation and even exacerbation. These mechanisms will probably include some brought into play by external triggers, along with some purely internal mechanisms, such as suppression and inhibition, and the interaction of these two types of mechanisms (38) .
With the exception of the only study based solely on a prisoner-of-war sample (10) , the military studies consistently showed high rates of delayed-onset PTSD, whether they were retrospective or longitudinal. Although only military samples have been followed over long periods, there is evidence that a substantial proportion of delayed-onset PTSD occurs soon after return from deployment. A recent study of soldiers evacuated from combat in Iraq and Afghanistan suggests that injuries, particularly severe ones, tend to retard the development of PTSD by several months, and this could account for at least some cases of delayed-onset PTSD (39) . Longer follow-up of civilian samples may also help to throw light on the apparent difference in rates. The consistency of findings from a variety of different research designs and settings in different countries and at different times suggests that exaggerated reporting due to a desire for compensation is unlikely to be a major factor. If it does occur, the pattern of findings suggests that it is most likely to involve exaggeration of symptoms previously experienced in a milder form. Furthermore, it is not clear that exaggerated reporting can explain the substantial difference in delayed-onset PTSD rates between military and civilian populations, as compensation is also likely to be a factor in nonmilitary trauma. In two civilian studies, compensation did not predict the development of PTSD, although the numbers involved were very small (29 , 34) . Finally, it may be noted that in the post-Vietnam War era, with the diagnosis of PTSD firmly established, there is less reason for the search for compensation to specifically involve delayed-onset rather than acute-onset PTSD.
Other explanations for high rates of delayed-onset PTSD in military samples rely on theory and clinical observation rather than systematic evidence but provide some hypotheses for future investigation. Some authors predicted a plethora of delayed stress reactions after the Vietnam War and pointed to the role of emotional numbing and denial facilitated by troop management and military training (40 , 41) . Horowitz and Solomon (40) speculated that the nature of modern warfare (short combat periods interspersed with periods of relative safety) is conducive to the maintenance of denial and numbing reactions. The perception of prolonged safety on repatriation might result in a relaxation of defensive coping strategies after a period of good functioning, leading to the reemergence of intrusive trauma recollections. In the same vein, Shatan (41) suggested that delayed stress reactions in Vietnam veterans were secondary to emotional anesthesia resulting both from the trauma and from military training that discouraged grief and intimacy. In the context of the 1982 Lebanon war, other authors have been mindful of the role of subsequent war stressors that might act as reminders of earlier combat stress in triggering delayed-onset PTSD (35) . Indeed, it cannot be ruled out that immediate reactions to trauma from subsequent tours of duty might account for some cases of supposed delayed-onset PTSD.
Review of the relevant case studies provides a further source of explanation specific to delayed-onset PTSD in the elderly. However, in this context we cannot rule out the possibility that the long delays involved may have concealed a reactivation of previous conditions rather than constituting true delayed onset. The most prevalent triggers to delayed-onset PTSD in the case studies were related to the onset of neurological and other disorders affecting cognition in elderly combat veterans. As mentioned by some authors (e.g., reference 15 ), such disorders are likely to involve damage to the prefrontal cortex, leading to disconnections with other brain areas. The inhibiting effect of the prefrontal cortex on regulating thoughts and emotions may therefore be lost (42) . A compatible explanation provided by Grossman et al. (15) is that decreased cognitive functioning leads to diminished capacity to utilize previously successful coping strategies to ward off aversive thoughts and symptoms.
This review has gone some way to resolving the uncertainty about how to interpret the existing data on delayed-onset PTSD. However, given the diversity of methodologies in existing studies, some ambiguities and uncertainties remain. Establishing reliable knowledge about delayed-onset PTSD will depend on the adoption in future editions of DSM of a more explicit definition that includes the likelihood of at least some prior symptoms becoming exacerbated or reactivated. This definition implies that there is a need to discriminate between those individuals whose initial symptoms are part of normal recovery and those who remain at risk. In addition, it would be valuable to know whether delayed-onset PTSD is equivalent to acute-onset PTSD in terms of risk factors, type of trauma exposure, clinical features, course, and response to treatment. For example, do formal interventions, social support, and subsequent life stress play more of a role in one condition than in the other? Finally, it should be borne in mind that few studies have had delayed-onset PTSD as their primary focus. Hence, they often have insufficient statistical power to examine this condition, and further research with larger samples of individuals with delayed-onset PTSD is needed to identify and shape interventions for vulnerable groups.

1. Andreasen NC: Acute and delayed posttraumatic stress disorders: a history and some issues (editorial). Am J Psychiatry 2004; 161:1321–1323Google Scholar
2. Bryant RA, Harvey AG: Delayed-onset posttraumatic stress disorder: a prospective evaluation. Aust NZ J Psychiatry 2002; 36:205–209Google Scholar
3. North CS, Pfefferbaum B, Tivis L, Kawasaki A, Reddy C, Spitznagel EL: The course of posttraumatic stress disorder in a follow-up study of survivors of the Oklahoma City bombing. Ann Clin Psychiatry 2004; 16:209–215Google Scholar
4. Atkinson RM, Henderson RG, Sparr LF, Deale S: Assessment of Viet Nam veterans for posttraumatic stress disorder in Veterans Administration disability claims. Am J Psychiatry 1982; 139:1118–1121Google Scholar
5. Sparr L, Pankratz LD: Factitious posttraumatic stress disorder. Am J Psychiatry 1983; 140:1016–1019Google Scholar
6. Brewin CR: Posttraumatic Stress Disorder: Malady or Myth? New Haven, Yale University Press, 2003Google Scholar
7. Shalev AY: Psycho-biological perspectives on early reactions to traumatic events, in Reconstructing Early Intervention After Trauma. Edited by Ørner R, Schnyder U. Oxford, England, Oxford University Press, 2002, pp 57–64Google Scholar
8. Kluznik JC, Speed N, Van Valkenburg C, Magraw R: Forty-year follow-up of United States prisoners of war. Am J Psychiatry 1986; 143:1443–1446Google Scholar
9. Brewin CR, Andrews B, Valentine JD: Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol 2000; 68:748–766Google Scholar
10. Engdahl B, Dikel TN, Eberly R, Blank A Jr: Comorbidity and course of psychiatric disorders in a community sample of former prisoners of war. Am J Psychiatry 1998; 155:1740–1745Google Scholar
11. Speed N, Engdahl B, Schwartz J, Eberly R: Posttraumatic stress disorder as a consequence of the POW experience. J Nerv Ment Dis 1989; 177:147–153Google Scholar
12. Bryant RA: Posttraumatic stress disorder, flashbacks, and pseudomemories in closed head injury. J Trauma Stress 1996; 9:621–629Google Scholar
13. Burstein A: How common is delayed posttraumatic stress disorder? (letter). Am J Psychiatry 1985; 142:887Google Scholar
14. Cassiday KL, Lyons JA: Recall of traumatic memories following cerebral vascular accident. J Trauma Stress 1992; 5:627–631Google Scholar
15. Grossman AB, Levin BE, Katzen HL, Lechner S: PTSD symptoms and onset of neurologic disease in elderly trauma survivors. J Clin Exp Neuropsychol 2004; 26:698–705Google Scholar
16. Herrmann N, Eryavec G: Delayed onset post-traumatic stress disorder in World War II veterans. Can J Psychiatry 1994; 39:439–441Google Scholar
17. Hilton C: Media triggers of post-traumatic stress disorder 50 years after the Second World War. Int J Geriatr Psychiatry 1997; 12:862–867Google Scholar
18. Lim LCC: Delayed emergence of PTSD. Singapore Med J 1991; 32:92–93Google Scholar
19. Ørner RJ, de Loos W: Second World War veterans with chronic post-traumatic stress disorder. Advances in Psychiatric Treatment 1998; 4:211–218Google Scholar
20. Ruzich MJ, Looi JCL, Robertson MD: Delayed onset of posttraumatic stress disorder among male combat veterans. Am J Geriatr Psychiatry 2005; 13:424–427Google Scholar
21. Solomon Z, Kotler M, Shalev A, Lin R: Delayed onset PTSD among Israeli veterans of the 1982 Lebanon War. Psychiatry 1989; 52:428–436Google Scholar
22. Breslau N, Davis GC, Andreski P, Peterson E: Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry 1991; 48:216–222Google Scholar
23. Breslau N, Davis GC, Peterson EL, Schulz L: Psychiatric sequelae of posttraumatic stress disorder in women. Arch Gen Psychiatry 1997; 54:81–87Google Scholar
24. Helzer JE, Robins LN, McEvoy LM: Post-traumatic stress disorder in the general population: findings of the Epidemiological Catchment Area survey. N Engl J Med 1987; 317:1630–1634Google Scholar
25. Prigerson HG, Maciejewski PK, Rosenheck RA: Combat trauma: trauma with highest risk of delayed onset and unresolved posttraumatic stress disorder symptoms, unemployment, and abuse among men. J Nerv Ment Dis 2001; 189:99–108Google Scholar
26. Yule W, Bolton D, Udwin O, Boyle S, O’Ryan D, Nurrish J: The long-term psychological effects of a disaster experienced in adolescence, I: the incidence and course of PTSD. J Child Psychol Psychiatry 2000; 41:503–511Google Scholar
27. Koren D, Arnon I, Klein E: Long-term course of chronic posttraumatic stress disorder in traffic accident victims: a three-year prospective follow-up study. Behav Res Ther 2001; 39:1449–1458Google Scholar
28. Epstein R: Avoidant symptoms cloaking the diagnosis of PTSD in patients with severe accidental injury. J Trauma Stress 1993; 6:451–458Google Scholar
29. Buckley TC, Blanchard EB, Hickling EJ: A prospective examination of delayed onset PTSD secondary to motor vehicle accidents. J Abnorm Psychol 1996; 105:617–625Google Scholar
30. Sungur M, Kaya B: The onset and longitudinal course of a man-made post-traumatic morbidity: survivors of the Sivas disaster. Int J Psychiatry Clin Pract 2001; 5:195–202Google Scholar
31. Southwick SM, Morgan CA III, Darnell A, Bremner D, Nicolaou AL, Nagy LM, Charney DS: Trauma-related symptoms in veterans of Operation Desert Storm: a 2-year follow-up. Am J Psychiatry 1995; 152:1150–1155Google Scholar
32. Watson CG, Kucala T, Manifold V, Vassar P, Juba M: Differences between posttraumatic stress disorder patients with delayed and undelayed onsets. J Nerv Ment Dis 1988; 176:568–572Google Scholar
33. North CS, McCutcheon V, Spitznagel EL, Smith EM: Three-year follow-up of survivors of a mass shooting episode. J Urban Health 2002; 79:383–391Google Scholar
34. Mayou R, Tyndell S, Bryant B: Long-term outcome of motor vehicle accident injury. Psychosom Med 1997; 59:578–584Google Scholar
35. Solomon Z, Mikulincer M: Trajectories of PTSD: a 20-year longitudinal study. Am J Psychiatry 2006; 163:659–666Google Scholar
36. Bremner JD, Southwick SM, Darnell A, Charney DS: Chronic PTSD in Vietnam combat veterans: course of illness and substance abuse. Am J Psychiatry 1996; 153:369–375Google Scholar
37. Op den Velde W, Falger PRJ, Hovens JE, de Groen JHM, Lasschuit LJ, Van Duijn H, Schouten EGW: Posttraumatic stress disorder in Dutch resistance veterans from World War II, in International Handbook of Traumatic Stress Syndromes. Edited by Wilson JP, Raphael B. New York, Plenum, 1993, pp 219–230Google Scholar
38. Brewin CR, Dalgleish T, Joseph S: A dual representation theory of posttraumatic stress disorder. Psychol Rev 1996; 103:670–686Google Scholar
39. Grieger TA, Cozza SJ, Ursano RJ, Hoge C, Martinez PE, Engel CC, Wain HJ: Posttraumatic stress disorder and depression in battle-injured soldiers. Am J Psychiatry 2006; 163:1777–1783Google Scholar
40. Horowitz MJ, Solomon GF: A prediction of delayed stress response syndromes in Vietnam veterans. J Soc Issues 1975; 31:67–80Google Scholar
41. Shatan CF: The grief of soldiers: Vietnam combat veterans’ self-help movement. Am J Orthopsychiatry 1973; 43:640–653Google Scholar
42. Vasterling JJ, Brailey K: Neuropsychological findings in adults with PTSD, in Neuropsychology of PTSD: Biological, Cognitive, and Clinical Perspectives. Edited by Vasterling JJ, Brewin CR. New York, Guilford, 2005, pp 178–207Google Scholar