Differential Effects of Aripiprazole on D 2 , 5-HT 2 , and 5-HT 1A Receptor Occupancy in Patients With Schizophrenia: A Triple Tracer PET Study
Abstract
Objective: Aripiprazole has a unique pharmacological profile that includes partial agonism at D 2 receptors, antagonism at 5-HT 2 receptors, and partial agonism at 5-HT 1A receptors. The authors conducted a positron emission tomography (PET) study to characterize the simultaneous effects of aripiprazole at the D 2 , 5-HT 2 , and 5-HT 1A receptors in patients with schizophrenia or schizoaffective disorder. Method: Twelve patients who had previously received antipsychotic treatment were randomly assigned to receive 10 mg, 15 mg, 20 mg, or 30 mg of aripiprazole. After at least 14 days of treatment, participants underwent high-resolution PET scans using [ 11 C]raclopride, [ 18 F]setoperone, and [ 11 C]WAY100635. Results: Very high occupancy was observed at striatal D 2 receptors (average putamen, 87%; caudate, 93%; and ventral striatum, 91%), lower occupancy at 5-HT 2 receptors (54%–60%), and even lower occupancy at 5-HT 1A receptors (16%). D 2 occupancy levels were significantly correlated with plasma drug concentrations, and even the lowest dose (10 mg) led to 85% D 2 occupancy. Extrapyramidal side effects were seen only in two of the four participants with occupancies exceeding 90%. Conclusions: Aripiprazole exhibits a unique occupancy profile as compared with other conventional and atypical antipsychotics. The threshold for response appears to be higher than 60%, extrapyramidal side effects appear to be uncommon even at occupancies that exceed the conventional extrapyramidal side effects threshold of 80%, and 5-HT 2 occupancy is lower than D 2 occupancy. Implications for aripiprazole’s mechanism of action are discussed.
Aripiprazole is the first antipsychotic to be introduced that has a mechanism of action that deviates from those of both conventional and atypical antipsychotics. It has a high affinity for the dopamine D 2 receptor (K i =0.34 nmol), a level similar to that of haloperidol (K i =0.7 nmol) but lower than that of other atypical antipsychotics (1) . In vitro, aripiprazole acts as a partial agonist (1 – 4) , a property that distinguishes it from the full-antagonist profile of all other conventional and atypical antipsychotic drugs (5) . In a recent rodent study, the least effective dose to inhibit the conditioned avoidance response was associated with a striatal D 2 receptor occupancy exceeding 80%, in contrast to haloperidol and risperidone, which showed inhibition of the conditioned avoidance response at 60% occupancy (6) . Furthermore, aripiprazole was not associated with any catalepsy, despite an occupancy exceeding 80% (6) . Thus, in preclinical studies, aripiprazole has shown distinction from other antipsychotics at both the cellular and system levels.
In addition to its effects on D 2 receptors, aripiprazole also shows antagonism at 5-HT 2 receptors (K i =8.7 nmol) (4) and partial agonism at 5-HT 1A receptors (K i =1.65 nmol) (7) . Aripiprazole differs from atypical antipsychotics (amisulpride excepted) in that it shows a lower in vitro affinity for 5-HT 2 receptors than for D 2 receptors (8) . The 5-HT 2 occupancy of aripiprazole in human beings in vivo is unknown, although a recent preclinical study showed very low 5-HT 2 receptor occupancy in rats (median effective dose >30 mg/kg) (6) . At 5-HT 1A receptors, aripiprazole shows levels of in vitro potency and intrinsic activity similar to those of ziprasidone (7) , although little is known about the binding to 5-HT 1A receptors in human beings.
At clinically effective antipsychotic doses of 10–30 mg per day, aripiprazole carries a low risk of extrapyramidal side effects or elevation of prolactin levels (9) . While preclinical studies have explored the contribution of aripiprazole’s pharmacological profile to its atypicality in terms of neurological side effects, no positron emission tomography (PET) studies have been conducted of this agent in patients with schizophrenia. In a previous PET study with healthy volunteers (10) , subtherapeutic doses of aripiprazole (0.5 mg, 1 mg, and 2 mg per day) resulted in <80% striatal D 2 receptor occupancy at steady state, while therapeutic doses (10–30 mg per day) resulted in >80% striatal D 2 receptor occupancy without extrapyramidal side effects or prolactin elevation. These observations indicate a profile that contrasts with those of other antipsychotic drugs, which are associated with the emergence of extrapyramidal side effects and hyperprolactinemia at striatal D 2 occupancies >80%, and suggest that aripiprazole may show a higher D 2 occupancy threshold for both response and extrapyramidal side effects.
In light of aripiprazole’s unique in vitro profile, its partial agonist action at the D 2 receptors, claims about its pharmacological effects at 5-HT 2 and 5-HT 1A receptors, and its favorable clinical profile, we conducted a PET study to characterize its simultaneous effects at the D 2 , 5-HT 1A , and 5-HT 2 receptors at therapeutic doses (10–30 mg/day) using three different radiotracers in patients with schizophrenia or schizoaffective disorder.
Method
The study was approved by the Research Ethics Board of the Centre for Addictions and Mental Health, Toronto. After providing informed consent, all participants underwent a physical examination and a battery of laboratory assessments. We used a randomized block design, with three participants per dose level, in which patients with schizophrenia or schizoaffective disorder were assigned to receive 10 mg, 15 mg, 20 mg, or 30 mg of aripiprazole. Diagnoses were confirmed by use of the Mini-International Neuropsychiatric Interview (11) . Previous antipsychotic medications other that olanzapine were discontinued and replaced by the assigned dose of aripiprazole, without taper or titration. Participants who were taking olanzapine were tapered from this drug over 7 days to minimize cholinergic withdrawal symptoms. No concomitant antipsychotic medications or change in other concomitant psychotropic medications were allowed during the study period. Patients with active substance abuse or a positive urine drug screen, as well as patients who had been treated with depot antipsychotic drugs within the previous 6 months, were excluded from the study. The following clinical assessments were conducted at baseline and then weekly thereafter: the Positive and Negative Syndrome Scale (PANSS) (12) , the Clinical Global Impression scale (CGI) (13) , the Global Assessment of Functioning Scale, the Simpson-Angus Rating Scale (14) , the Barnes Rating Scale for Drug-Induced Akathisia (15) , and the Abnormal Involuntary Movement Scale (16) .
After at least 14 days of treatment with aripiprazole, participants underwent PET scanning using [ 11 C]raclopride, [ 18 F]setoperone, and [ 11 C]WAY100635. Scanning was done 3–5 hours after administration of aripiprazole (peak plasma level=3–5 hours). The [ 11 C]raclopride and [ 11 C]WAY100635 scans, separated by an interval of at least 3 hours, were done on one day, and the [ 18 F]setoperone scan on another. Venous blood was collected to assess plasma concentrations of drug and prolactin at the time of scanning. For plasma prolactin concentration, a chemiluminescent immunoassay with a sensitivity of 0.25 mg/liter (Access Immunoassay System, Prolactin 33530) was used. Plasma concentrations of aripiprazole and its principal metabolite, dehydroaripiprazole, were determined using a validated LC-API-MS/MS assay (Alta Analytical Laboratory, Inc., El Dorado Hills, Calif.).
PET scanning was done with a Siemens HRRT high-resolution neuro-PET camera system (Siemens Molecular Imaging, Knoxville, Tenn.) measuring radioactivity in 207 brain sections with a thickness of 1.2 mm each and an in-plane resolution of approximately 2.8 mm full width at half-maximum. Transmission scans were acquired immediately before emission scans using a single photon point source ( 137 Cs; T 50 =30.2 years, Eg=662 keV); these were used to correct the emission scans for the attenuation of 511 keV photons through tissue and head support. A saline solution containing a mean of 9.8 mCi [ 11 C]raclopride (SD=0.7) with a specific activity (at time of injection) of 1,243 mCi/mmol (SD=294) was injected as a bolus into an intravenous line placed in an antecubital vein. Similar procedures were done for [ 11 C]WAY100635 scans (mean dose=9.2 mCi [SD=0.8], specific activity=1,633 mCi/mmol [SD=827]) and [ 18 F]setoperone scans (mean dose=4.8 mCi/mmol [SD=0.2], specific activity=823 mCi/mmol [SD=619]). Emission data were acquired in list mode for the highest possible temporal resolution. Emission data were acquired over 60 minutes for the [ 11 C]raclopride scan and 90 minutes for the [ 11 C]WAY100635 and [ 18 F]setoperone scans. Raw data were reconstructed by filtered-back projection to yield dynamic images. For the [ 11 C]raclopride PET images, data were analyzed in 28 frames (five 1-minute, twenty 2-minute, and three 5-minute frames); for the [ 11 C]WAY100635 images, in 18 frames (three 20-second, three 1-minute, three 2-minute, two 5-minute, and seven 10-minute frames); and for the [ 18 F]setoperone images, in 22 frames (five 1-minute and seventeen 5-minute frames).
Participants underwent standard fast spin echo T1-weighted imaging (fast spoiled gradient echo, time to echo=5.3–15 msec, repetition time=8.9–12 msec, field of view=20 cm [three-dimensional], 256×256 voxel 1.5 isotropic, number of excitations=1) and a proton density image (time to echo=17, repetition time=6,000, field of view=22 cm [two-dimensional], 256×256, slice thickness=2 mm, number of excitations=2) acquired on a 1.5T Sigma-GE scanner. The T1 image was used for the analysis of the [ 11 C]WAY100635 and [ 18 F]setoperone scans, and the proton density image for the [ 11 C]raclopride scans.
The regions of interest were the caudate, putamen, and ventral striatum for the [ 11 C]raclopride scan and the frontal and temporal cortices for the [ 18 F]setoperone and [ 11 C]WAY100635 scans, as these regions are rich in D 2 , 5-HT 1A , and 5-HT 2 receptors, respectively. The cerebellar cortex, excluding the vermix, was used as the reference region for each of the three PET scans (17 – 19) . Time activity curves were obtained from dynamic PET images in native space with reference to regions of interest generated with in-house software for semiautomated generation of regions of interest from the coregistered magnetic resonance images (20) .
To calculate receptor occupancy, data were obtained from age- and sex-matched healthy subjects (N=23, N=13, and N=24, respectively, for the [ 11 C]raclopride, [ 11 C]WAY100635, and [ 18 F]setoperone scans) using the same imaging protocols as described above and used to estimate the participants’ unmedicated binding potential. Previous studies have not shown a major effect of illness on [ 11 C]raclopride, [ 11 C]WAY100635, and [ 18 F]setoperone binding potential (21 – 23) . The outcome measure was the binding potential (BP), defined as the ratio of k3 to k4, where k3 and k4 are the rate constants of radioligand delivery and transfer out of the specifically bound compartment in a three-compartment model (24) . Formally, BP=k3/k4=1/V2×B max /K d , where V2 is the volume of distribution of the radioligand in the nondisplaceable compartments (which is assumed to be constant between individuals), B max is the receptor concentration, and K d is the affinity (25) . In this study, binding potential is taken as a measure of the available receptors in the region of interest. An estimate of the binding potential was obtained by use of the simplified reference tissue model (26 , 27) , using PMOD software, version 2.7 (PMOD Technologies, Ltd., Zurich, Switzerland).
Occupancy was calculated as the percentage reduction in binding potential obtained after treatment with aripiprazole when compared with age-matched healthy comparison subjects [(BP healthy – BP drug )/BP healthy × 100]. In addition, for an alternative index of receptor occupancy as measured by [ 11 C]WAY100635, we measured the change in area under the curve for each region of interest as a function of treatment with aripiprazole (28) .
Bivariate correlation analysis was used to examine the relationship between the primary variables of interest. Nonlinear regression analysis was used to evaluate the relationship between dose and D 2 receptor occupancy. Descriptive statistics were used to summarize clinical rating scale scores at baseline and 4 weeks, and within-group t tests were performed to test whether any of the changes were significantly different from zero.
Results
Sixteen patients completed the informed consent procedure, and 12 patients completed the study imaging procedures. Two patients failed screening (one could not commit to the study schedule because of other commitments, and the other was no longer interested in participating). Two patients (both assigned to receive 30 mg aripiprazole) dropped out of the study (after 1 and 4 weeks, respectively) before completing the brain imaging procedures and were replaced. The reasons for study discontinuation were insomnia and seizure, respectively. The patient who suffered a seizure later acknowledged a lifelong history of seizures, and the one who complained of insomnia had been nonadherent with a previously prescribed valproic acid regimen during the study. Among the 12 patients who completed the imaging procedures, nine were male, and the mean age was 31 years (SD=7). Those who completed the study were diagnosed as having either schizophrenia (10 patients) or schizoaffective disorder (two patients); the self-reported mean age at first episode was 23 years (SD=4). At baseline, participants were either off antipsychotic medications (four patients) or taking risperidone (five patients; 2.5–6.0 mg/day), olanzapine (two patients; 10 mg/day and 30 mg/day), or clozapine (one patient, 100 mg/day).
Table 1 presents clinical rating scale scores at baseline and after 4 weeks of treatment with aripiprazole. Because the study was not designed to detect changes in clinical rating scales, these results are presented for descriptive purposes only. The following adverse events were reported during the study period: difficulty falling asleep or interrupted sleep (N=7), restlessness (N=5), dizziness (N=5), dystonia (N=1), nightmare (N=1), headache (N=1), nausea (N=1), decreased appetite (N=1), and seizure (N=1).
Mean plasma aripiprazole concentrations did not differ at the time of the three respective scans ([ 11 C]raclopride: 221 ng/ml [SD=179]; [ 11 C]WAY100635: 199 ng/ml [SD=173]; [ 18 F]setoperone: 218 ng/ml [SD=176]). Mean plasma concentrations of dehydroaripiprazole were similar at the times of the three scans ([ 11 C]raclopride: 53 ng/ml [SD=26]; [ 11 C]WAY100635: 51 ng/ml [SD=26]; [ 18 F]setoperone: 52 ng/ml [SD=27]). Mean plasma aripiprazole and dehydroaripiprazole levels for each dose group are listed in Table 2 . A modest linear correlation was observed between dose and plasma levels of aripiprazole (r=0.67, p=0.02) and dehydroaripiprazole (r=0.63, p=0.03). Mean prolactin concentration decreased from 21 mg/liter (SD=16) at baseline to 9 mg/liter (SD=13) at the time of the [ 11 C]raclopride scan (mean change, 12 mg/liter [SD=21]). Only one participant, a female patient who had been off antipsychotic medication at the start of the study, showed an increase in prolactin concentration, from 6 mg/liter at baseline to 47 mg/liter at the time of the [ 11 C]raclopride scan (reference range=3–27 mg/liter).
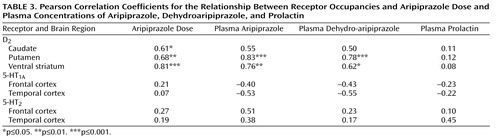
We found high occupancy at striatal dopamine D 2 receptors (putamen, 86.6% [SD=3.7]; caudate, 92.9% [SD=5.7]; and ventral striatum, 91.0% [SD=4.0]). Even the lowest dose (10 mg) resulted in a mean occupancy of 85% (putamen range=81%–88%), and occupancy increased in a dose-related manner to a mean of 91% at the maximum dose of 30 mg (range=90%–94%). The D 2 occupancy in the putamen was lower than that in the caudate (p<0.001) and ventral striatum (p=0.01), while the latter two were not reliably distinguishable. As shown in Table 3 , aripiprazole dose and plasma concentration showed a significant linear correlation with D 2 occupancy in all three regions of interest.
Drug occupancy was lower for 5-HT 2 receptors (temporal cortex: mean=54.0% [SD=15.3, range=30.9–79.2]; frontal cortex: 59.4% [SD=12.9, range=43.4–83.5]), and lowest for 5-HT 1A receptors (temporal cortex: mean=16.2% [SD=14.3, range=0–39]; frontal cortex: 16.5% [SD=13.8, range= –2.0 to 43.5]; F=323.63, df=2, 81, p<0.001 for pairwise comparisons in all cases) ( Figure 1 ). There was no difference between frontal and temporal occupancy for 5-HT 1A receptors and 5-HT 2 receptors. 5-HT 1A and 5-HT 2 receptor occupancies exhibited no relationship with dose, plasma aripiprazole concentration, or plasma dehydroaripiprazole concentration ( Table 3 ).
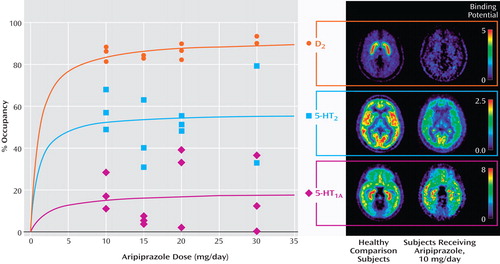
a Patients were treated with aripiprazole for at least 14 days and underwent PET scanning with three radioligands 3–5 hours after oral administration of the drug on two different days. The panel on the right represents averaged binding potential maps for the three participants who received 10 mg of aripiprazole and the age- and sex- matched comparison subjects (N=23, N=13, and N=24, respectively, for the [ 11 C]raclopride, [ 11 C]WAY100635, and [ 18 F]setoperone scans).
Extrapyramidal side effects occurred only in two of the four participants in whom D 2 occupancy exceeded 90%. One of them, in the 30 mg dose group, suffered dystonia and parkinsonism requiring treatment with benztropine; the other, in the 20 mg dose group, suffered increased tone in the upper extremities accompanied by an increase in plasma prolactin concentration. In both participants, the plasma aripiprazole concentration (442 ng/ml and 663 ng/ml, respectively) and dehydroaripiprazole concentration (78 ng/ml and 94 ng/ml, respectively) were substantially higher than the mean concentration within their respective dose group (see Table 2 ).
Discussion
This is the first study to document the very high D 2 receptor occupancy in patients at clinically effective doses of aripiprazole. This finding is consistent with the observation of >80% striatal D 2 occupancy reported earlier in healthy subjects receiving 10 mg or 30 mg of aripiprazole (10) . Plotting the dose-occupancy relationship using pooled data from the present study and the earlier study (subclinical dose-occupancy data from Yokoi et al. [10] ) reveals the expected saturating hyperbolic relationship between dose and D 2 receptor occupancy. In contrast to all other conventional and atypical antipsychotics (with the exception of clozapine), for which the minimum therapeutic dose has been shown to correspond to an expected D 2 receptor occupancy around 60%–65%, the estimated aripiprazole dose associated with 60% D 2 receptor occupancy is closer to a subtherapeutic dose of 1 mg. The minimally effective dose of 10 mg is associated with occupancy closer to 85%, suggesting that the occupancy threshold for clinical response for aripiprazole is above 80%.
Only two participants suffered extrapyramidal side effects; both were among the four participants in whom D 2 occupancy exceeded 90%, which suggests the possibility that slow metabolizers or individuals who have higher drug concentrations for other reasons may be at higher risk of developing extrapyramidal side effects. The emergence of such symptoms only at D 2 occupancy exceeding 90% raises the possibility that the threshold for extrapyramidal side effects is closer to 90% for aripiprazole, compared with 80% for other antipsychotic drugs.
The observation of an occupancy threshold shift for clinical efficacy with aripiprazole compared with other classical dopamine D 2 antagonists is consistent with a recent preclinical study (6) showing dissociation between aripiprazole’s D 2 occupancy and its functional antagonism at D 2 receptors. Natesan et al. (6) showed that in contrast to the observed 60% receptor occupancy threshold for inhibition of the conditioned avoidance response (a preclinical predictor of antipsychotic efficacy) for haloperidol and risperidone, this threshold shifted to 86% for aripiprazole. This apparent shift in threshold for conditioned avoidance response inhibition in rodents and therapeutic response in human subjects is probably a function of the drug’s partial agonist profile at D 2 receptors.
This is also the first study to document aripiprazole’s occupancy of serotonin 5-HT 2 receptors, and our data confirm that aripiprazole binds to this receptor in human subjects in vivo. However, aripiprazole exhibits a higher occupancy at D 2 receptors (87% [SD=4%]) than at 5-HT 2 receptors (52% [SD=18]); in this regard, its profile is more similar to haloperidol’s than to those of atypical antipsychotics. This new finding is consistent with aripiprazole’s higher D 2 affinity in vitro as well as recent occupancy data from an in vivo rodent study (6) , and it confirms that aripiprazole’s atypical profile in vivo is not related to a high 5-HT 2 /D 2 binding profile.
Aripiprazole has been shown to bind with high affinity to recombinant human 5-HT 1A receptors (h5-HT 1A ) (K i =1.65 nmol) and to display a partial agonist pharmacological profile (E max =68% of 5-HT) that is similar to ziprasidone in potency and intrinsic activity (E max =79% of 5-HT) (7) . This is important because partial agonism at the 5-HT 1A receptor has been postulated as a potential therapeutic mechanism in the alleviation of depression, anxiety, negative symptoms, and extrapyramidal side effects (29 – 31) . In rodent studies, 5-HT 1A agonists have been found to diminish the propensity for catalepsy (29) and to attenuate prolactin elevation (32) induced by D 2 antagonists, which suggests a mechanistic role in the atypical profile of ziprasidone and aripiprazole. In this study, we found very low occupancy of aripiprazole at the 5-HT 1A receptor (mean=16%). However, it has been shown that when [ 11 C]WAY100635 is used, other partial agonists also show low occupancies in this range (22 , 33) . Whether the low occupancy we observed reflects the true state of affairs or is an underestimate resulting from the use of an antagonist radiotracer to measure agonist binding is not clear. Underestimation may arise from the fact that agonists bind predominantly to the high-affinity-state sites (G-protein coupled), while antagonists bind equally to both high- and low-affinity-state sites (G-protein uncoupled) (34 , 35) . Thus, even though an agonist may bind to a high proportion of the high-affinity-state sites, this may not necessarily be representative of the total receptor population. Nonetheless, a recent study (36) has questioned aripiprazole’s high efficacy at 5-HT 1A receptors and suggested that the experimental conditions used in previous research (7) may have amplified the detection of aripiprazole’s weak partial agonist activity and even attributed partial agonist activity to risperidone, which is virtually devoid of 5-HT 1A activity. This is consistent with results from recent rodent studies (37 , 38) that failed to find a substantial role for aripiprazole’s 5-HT 1A partial agonism in the attenuation of catalepsy (37) or modulation of extracellular dopamine and serotonin in the prefrontal cortex and hippocampus, respectively (38) , arguing against a major role for this receptor in aripiprazole’s atypical antipsychotic profile.
A number of limitations qualify our conclusions. First, the study was powered to provide reliable occupancy estimates and was not designed to detect major clinical changes. While the data do suggest that the relationship between occupancy and subjective wellness (which is generally negative for other antagonist antipsychotics) may be different for partial agonists, this finding awaits replication from larger clinical studies. Second, the total number of scans was limited by safety considerations and the study participants’ prior medication exposure. The absence of the participants’ own baseline data introduces some error in the estimated occupancy, although this would be expected to be small and would not detract from the conclusions drawn in this study. Third, most participants had been previously maintained on other antipsychotic drugs, although the design ensured that there would be at least a 2-week washout of previous medication, so the spillover effect of these medications would be expected to be negligible.
In summary, therapeutic doses of aripiprazole are associated with D 2 receptor occupancies of >80% in patients with schizophrenia and an increased risk of extrapyramidal side effects at >90% D 2 occupancy, particularly in susceptible individuals, which suggests a shift in occupancy threshold for both clinical effect and extrapyramidal side effects compared with other antipsychotic drugs. Aripiprazole’s high D 2 /5-HT 2 binding profile in vivo contrasts with the profiles of other atypical antipsychotic drugs, which exhibit high 5-HT 2 /D 2 binding, and is consistent with the drug’s in vitro affinity and ex vivo findings in rodents. Finally, we confirm binding at cortical 5-HT 1A receptors in vivo, although occupancy at this receptor is very low and its clinical significance unclear.
1. Burris KD, Molski TF, Xu C, Ryan E, Tottori K, Kikuchi T, Yocca FD, Molinoff PB: Aripiprazole, a novel antipsychotic, is a high-affinity partial agonist at human dopamine D 2 receptors. J Pharmacol Exp Ther 2002; 302:381–389 Google Scholar
2. Tadori Y, Miwa T, Tottori K, Burris KD, Stark A, Mori T, Kikuchi T: Aripiprazole’s low intrinsic activities at human dopamine D 2L and D 2S receptors render it a unique antipsychotic. Eur J Pharmacol 2005; 515:10–19 Google Scholar
3. Inoue T, Domae M, Yamada K, Furukawa T: Effects of the novel antipsychotic agent 7-(4-[4-(2,3-dichlorophenyl)-1-piperazinyl]butyloxy)-3,4-dihydro-2(1H)-quinolinone (OPC-14597) on prolactin release from the rat anterior pituitary gland. J Pharmacol Exp Ther 1996; 277:137–143Google Scholar
4. Lawler CP, Prioleau C, Lewis MM, Mak C, Jiang D, Schetz JA, Gonzalez AM, Sibley DR, Mailman RB: Interactions of the novel antipsychotic aripiprazole (OPC-14597) with dopamine and serotonin receptor subtypes. Neuropsychopharmacology 1999; 20:612–627Google Scholar
5. Arnt J, Skarsfeldt T: Do novel antipsychotics have similar pharmacological characteristics? a review of the evidence. Neuropsychopharmacology 1998; 18:63–101Google Scholar
6. Natesan S, Reckless GE, Nobrega JN, Fletcher PJ, Kapur S: Dissociation between in vivo occupancy and functional antagonism of dopamine D 2 receptors: comparing aripiprazole to other antipsychotics in animal models. Neuropsychopharmacology 2006; 31:1854–1863 Google Scholar
7. Jordan S, Koprivica V, Chen R, Tottori K, Kikuchi T, Altar CA: The antipsychotic aripiprazole is a potent, partial agonist at the human 5-HT 1A receptor. Eur J Pharmacol 2002; 441:137–140 Google Scholar
8. Meltzer HY, Matsubara S, Lee JC: The ratios of serotonin2 and dopamine2 affinities differentiate atypical and typical antipsychotic drugs. Psychopharmacol Bull 1989; 25:390–392Google Scholar
9. Kane JM, Carson WH, Saha AR, McQuade RD, Ingenito GG, Zimbroff DL, Ali MW: Efficacy and safety of aripiprazole and haloperidol versus placebo in patients with schizophrenia and schizoaffective disorder. J Clin Psychiatry 2002; 63:763–771Google Scholar
10. Yokoi F, Grunder G, Biziere K, Stephane M, Dogan AS, Dannals RF, Ravert H, Suri A, Bramer S, Wong DF: Dopamine D 2 and D 3 receptor occupancy in normal humans treated with the antipsychotic drug aripiprazole (OPC 14597): a study using positron emission tomography and [ 11 C]raclopride. Neuropsychopharmacology 2002; 27:248–259 Google Scholar
11. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC: The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998; 59(suppl 20):22–33Google Scholar
12. Kay SR, Fiszbein A, Opler LA: The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull 1987; 13:261–276Google Scholar
13. Guy W (ed): ECDEU Assessment Manual for Psychopharmacology: Publication ADM 76-338. Washington, DC, US Department of Health, Education, and Welfare, 1976, pp 218–222Google Scholar
14. Simpson GM, Angus JWS: A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl 1970; 212:11–19Google Scholar
15. Barnes TRE: A rating scale for drug-induced akathisia. Br J Psychiatry 1989; 154:672–676Google Scholar
16. Guy W (ed): ECDEU Assessment Manual for Psychopharmacology: Publication ADM 76-338. Washington, DC, US Department of Health, Education, and Welfare, 1976, pp 534–537Google Scholar
17. Hall H, Farde L, Halldin C, Lundkvist C, Sedvall G: Autoradiographic localization of 5-HT 2A receptors in the human brain using [ 3 H]M100907 and [ 11 C]M100907. Synapse 2000; 38:421–431 Google Scholar
18. Hall H, Sedvall G, Magnusson O, Kopp J, Halldin C, Farde L: Distribution of D 1 - and D 2 -dopamine receptors, and dopamine and its metabolites in the human brain. Neuropsychopharmacology 1994; 11:245–256 Google Scholar
19. Blin J, Sette G, Fiorelli M, Bletry O, Elghozi JL, Crouzel C, Baron JC: A method for the in vivo investigation of the serotonergic 5-HT 2 receptors in the human cerebral cortex using positron emission tomography and 18 F-labeled setoperone. J Neurochem 1990; 54:1744–1754 Google Scholar
20. Rusjan P, Mamo D, Ginovart N, Hussey D, Vitcu I, Yasuno F, Tetsuya S, Houle S, Kapur S: An automated method for the extraction of regional data from PET images. Psychiatry Res 2006; 147:79–89Google Scholar
21. Farde L, Wiesel FA, Hall H, Halldin C, Stone-Elander S, Sedvall G: No D 2 receptor increase in PET study of schizophrenia. Arch Gen Psychiatry 1987; 44:671–672 Google Scholar
22. Bantick RA, Montgomery AJ, Bench CJ, Choudhry T, Malek N, McKenna PJ, Quested DJ, Deakin JF, Grasby PM: A positron emission tomography study of the 5-HT 1A receptor in schizophrenia and during clozapine treatment. J Psychopharmacol 2004; 18:346–354 Google Scholar
23. Trichard C, Paillere-Martinot ML, Attar-Levy D, Blin J, Feline A, Martinot JL: No serotonin 5-HT 2A receptor density abnormality in the cortex of schizophrenic patients studied with PET. Schizophr Res 1998; 31:13–17 Google Scholar
24. Mintun MA, Raichle ME, Kilbourn MR, Wooten GF, Welch MJ: A quantitative model for the in vivo assessment of drug binding sites with positron emission tomography. Ann Neurol 1984; 15:217–227Google Scholar
25. Ichise M, Meyer JH, Yonekura Y: An introduction to PET and SPECT neuroreceptor quantification models. J Nucl Med 2001; 42:755–763Google Scholar
26. Parsey RV, Slifstein M, Hwang DR, Abi-Dargham A, Simpson N, Mawlawi O, Guo NN, Van Heertum R, Mann JJ, Laruelle M: Validation and reproducibility of measurement of 5-HT 1A receptor parameters with [carbonyl- 11 C]WAY-100635 in humans: comparison of arterial and reference tissue input functions. J Cereb Blood Flow Metab 2000; 20:1111–1133 Google Scholar
27. Lammertsma AA, Hume SP: Simplified reference tissue model for PET receptor studies. Neuroimage 1996; 4:153–158Google Scholar
28. Khan TS, Sundin A, Juhlin C, Langstrom B, Bergstrom M, Eriksson B: 11 C-metomidate PET imaging of adrenocortical cancer. Eur J Nucl Med Mol Imaging 2003; 30:403–410 Google Scholar
29. Millan MJ, Brocco M, Veiga S, Cistarelli L, Melon C, Gobert A: WAY 100,635 enhances both the “antidepressant” actions of duloxetine and its influence on dialysate levels of serotonin in frontal cortex. Eur J Pharmacol 1998; 341:165–167Google Scholar
30. Millan MJ: Improving the treatment of schizophrenia: focus on serotonin 5-HT 1A receptors. J Pharmacol Exp Ther 2000; 295:853–861 Google Scholar
31. Meller E, Goldstein M, Bohmaker K: Receptor reserve for 5-hydroxytryptamine 1A-mediated inhibition of serotonin synthesis: possible relationship to anxiolytic properties of 5-hydroxytryptamine 1A agonists. Mol Pharmacol 1990; 37:231–237Google Scholar
32. Nash JF, Meltzer HY: Effect of gepirone and ipsapirone on the stimulated and unstimulated secretion of prolactin in the rat. J Pharmacol Exp Ther 1989; 249:236–241Google Scholar
33. Rabiner EA, Gunn RN, Wilkins MR, Sedman E, Grasby PM: Evaluation of EMD 128 130 occupancy of the 5-HT 1A and the D 2 receptor: a human PET study with [ 11 C]WAY-100635 and [ 11 C]raclopride. J Psychopharmacol 2002; 16:195–199 Google Scholar
34. Scaramellini C, Leff P: A three-state receptor model: predictions of multiple agonist pharmacology for the same receptor type. Ann N Y Acad Sci 1998; 861:97–103Google Scholar
35. Leff P: The two-state model of receptor activation. Trends Pharmacol Sci 1995; 16:89–97Google Scholar
36. Newman-Tancredi A, Assie MB, Leduc N, Ormiere AM, Danty N, Cosi C: Novel antipsychotics activate recombinant human and native rat serotonin 5-HT 1A receptors: affinity, efficacy, and potential implications for treatment of schizophrenia. Int J Neuropsychopharmacol 2005; 8:341–356 Google Scholar
37. Kleven MS, Barret-Grevoz C, Slot LB, Newman-Tancredi A: Novel antipsychotic agents with 5-HT 1A agonist properties: role of 5-HT 1A receptor activation in attenuation of catalepsy induction in rats. Neuropharmacology 2005; 49:135–143 Google Scholar
38. Assie MB, Ravailhe V, Faucillon V, Newman-Tancredi A: Contrasting contribution of 5-hydroxytryptamine 1A receptor activation to neurochemical profile of novel antipsychotics: frontocortical dopamine and hippocampal serotonin release in rat brain. J Pharmacol Exp Ther 2005; 315:265–272Google Scholar