In This Issue
Next “Step” in Treating Bipolar Depression
Refractory depression in patients with bipolar disorder is a major challenge. Standard treatment is a mood stabilizer plus an antidepressant. If these do not work, what should the clinician try next? Three adjuncts to ongoing treatment with a mood stabilizer plus antidepressant were compared in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Nierenberg et al. (p. 210) report that lamotrigine (mood stabilizer), inositol (sugar derivative affecting intracellular signaling), and risperidone (antipsychotic) did not differ significantly in the rate of recovery over 4 months. However, the patients receiving lamotrigine had fewer depressive symptoms and greater improvement at study exit than the other groups and remained in the study longer (12.2 weeks versus 8.6 for inositol and 5.8 for risperidone); they also had better global functioning than the risperidone group. These findings, combined with lamotrigine’s recovery rate of 23.8%, make this a promising add-on treatment.
Cognitive Problems in Bipolar Children
Adults with bipolar disorder have numerous cognitive impairments. Similar investigation is needed in bipolar children because their brains are still developing, they are more likely to receive multiple drugs, and many have attention deficit hyperactivity disorder (ADHD). In a comparison of children with bipolar I disorder and healthy children 8–17 years old, Pavuluri et al. (p. 286) confirmed that the bipolar children performed significantly worse on tests of attention, verbal memory, working memory, and executive function. It is not surprising that the bipolar children with ADHD had greater impairments than patients without ADHD. What is surprising is that clinically stable children receiving medication performed no better than unmedicated manic patients. This underscores the need of bipolar children for educational interventions and for treatments that address their cognitive deficits.
Disinhibited Children of Bipolar Parents
Children of parents with bipolar disorder have a high risk of developing it themselves. Discovering early predictors of bipolar disorder in these children would help identify the most vulnerable. Hirshfeld-Becker et al. (p. 265) propose behavioral disinhibition—an extreme tendency to seek novelty, approach stimuli, and display uncontrolled speech and actions—as a predisposing factor. The rates of behavioral disinhibition at age 2–6 years differed significantly between children of parents with and without bipolar disorder, 53% versus 34%. The rate was even higher, 67%, in children of parents with full mania. Behavioral disinhibition appeared to be distinct from attention deficit hyperactivity disorder and thus could signal high risk for bipolar disorder in these youngsters.
Optimal Valproate Levels
The effectiveness of valproate sodium for acute manic episodes depends on adequate levels in the blood. How high is high enough? Higher than indicated by current guidelines, conclude Allen et al. (p. 272), after pooling findings from three earlier studies. Stratification of valproate serum levels into six ranges revealed that only levels of 71 mg/ml or above produced significantly greater symptom response than did placebo, and values of 94 mg/ml or above worked better than those of 55 mg/ml or lower. The ranges did not differ in the rate of study discontinuation due to adverse events. Greater efficacy with equivalent tolerability makes a strong case for raising the target serum level for valproate.
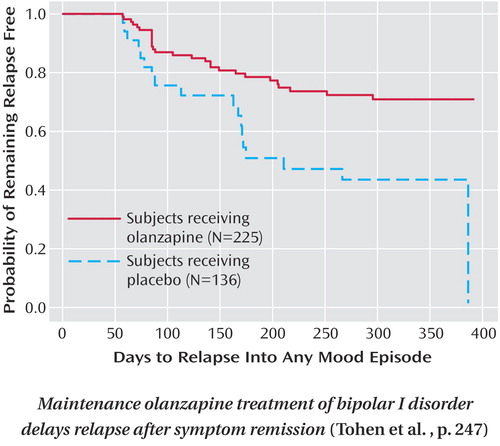
Long-Term Olanzapine for Bipolar Disorder
Bipolar disorder is recurrent and requires maintenance therapy. Lithium is standard for preventing relapse but is ineffective for many patients, and few other drugs are established as maintenance treatments. Several atypical antipsychotic drugs have shown success as short-term interventions for acute mania, and now Tohen et al. (p. 247) report a large 48-week double-blind olanzapine trial for maintenance treatment of bipolar disorder. Among patients in remission after short-term olanzapine use, the median time to relapse was 174 days for patients who continued taking olanzapine and 22 days for those switched to placebo (see figure). The rates of study completion were low, however: 21.3% for olanzapine and 6.6% for placebo. Olanzapine was associated with substantial weight gain, abnormal QTc interval, and increased prolactin level. Despite these drawbacks, olanzapine’s ability to prolong remission increases the long-term therapeutic possibilities for bipolar disorder.