Use of Psychotherapy for Depression in Older Adults
Abstract
OBJECTIVE: The authors examine national patterns in psychotherapy for older adults with a diagnosis of depression and analyze correlates of psychotherapy use that is consistent with Agency for Health Care Policy and Research guidelines for duration of treatment. METHOD: Linked Medicare claims and survey data from the 1992–1999 Medicare Current Beneficiary Survey were used. The data were merged with the Area Resource File to assess the effect of provider-supply influences on psychotherapy treatment. An episode-of-care framework approach was used to analyze psychotherapy use and treatment duration. Multiple logistic regression analysis was used to predict psychotherapy use and its consistency. RESULTS: The authors identified 2,025 episodes of depression treatment between 1992 and 1999. Overall, psychotherapy was used in 25% (N=474) of the episodes, with 68% of episodes with psychotherapy involving services received only from psychiatrists. (Percentages were weighted for the complex design of the Medicare Current Beneficiary Survey.) Use of psychotherapy was correlated with younger patient age, higher patient educational attainment, and availability of local psychotherapy providers. Among episodes in which psychotherapy was used, only a minority (33%, N=141) involved patients who remained in consistent treatment, defined as extending for at least two-thirds of the episode of depression. Availability of local providers was positively correlated with consistent psychotherapy use. In analyses with adjustment for provider-related factors, patients’ socioeconomic and demographic characteristics did not affect the odds of receiving consistent psychotherapy. CONCLUSIONS: Use of psychotherapy remains uncommon among depressed older adults despite its widely acknowledged efficacy. Some of the disparities in psychotherapy utilization suggest supply-side barriers. Increasing the geographic availability of mental health care providers may be one way of increasing access to psychotherapy for depressed older adults.
There is widespread consensus that geriatric depression is highly prevalent (1–3), adversely affects daily function and quality of life, and contributes to increased health care costs (4), physical decline (5), and even death (6).
Several types of psychotherapy are effective for depression in older adults (7, 8). In a meta-analysis of psychosocial treatments for geriatric depression, the overall effect size for treatment versus no treatment or placebo control was 0.78 (9). Although antidepressant medications are a mainstay of medical treatment for depression and have been shown to be safe and efficacious in older adults (10), patients often prefer psychotherapy (11, 12). Specifically, concern over medication side effects may be heightened when geriatric depression occurs in context of diabetes mellitus (13), cardiac disease (14), and other general medical illnesses. Among patients who are treated with antidepressants, high rates of medication nonadherence constrain clinical effectiveness (15). Older adults may face several barriers to psychotherapy treatment. Although nearly all older adults in the United States have basic health coverage through Medicare, Medicare fee-for-service reimbursement currently covers only 50% of mental health care costs. High copayments may put psychotherapy out of the reach of those in greatest need (16, 17). Often, depressed older adults are unwilling to seek treatment for their symptoms when they have to pay out of pocket for services (11). Primary care physicians may also not refer patients to psychotherapy because of a lack of awareness of its clinical efficacy (18).
Little information exists concerning patterns of psychotherapy use for depression in older adults. Most clinical trials involve participants who are highly selected from clinical settings and typically receive care free of charge. Given the results from patient preference studies (12, 19), psychotherapy remains an important but poorly understood option in the community treatment of depression in older adults. Although the Agency for Health Care Policy and Research guidelines (20) recommend treatment for 4–9 months to reduce the risk of recurrence, the frequency with which depressed older adults receive psychotherapy of this duration remains unknown.
In the study reported here, we examined national patterns in psychotherapy treatment of depression among older adults. The study is based on linked Medicare claims and survey data from the 1992–1999 Medicare Current Beneficiary Survey cost and use files.
Method
Data Sources
The Medicare Current Beneficiary Survey is a continuous survey of a nationally representative sample of aged, disabled, and institutionalized Medicare beneficiaries with information on health status, health care use and expenditures, health insurance coverage, and socioeconomic and demographic characteristics. It has a complex sample design in which sampling is conducted first at the level of primary sampling units (geographically based clusters that represent cities or county groups) and then at the person level. Weights are provided to generalize to the total population enrolled in Medicare for a given year; because data for some respondents are weighted more heavily than those for others to achieve national representativeness, weighted percentages differ somewhat from those based on raw cell sizes. Data from interviews and Medicare claims were linked to examine depression diagnosis and use of psychotherapy among adults ages 65 years and older. The data were augmented through merging with the Area Resource File to provide county-level information (21).
Study Sample
The study sample (N=1,542) was restricted to community-dwelling Medicare beneficiaries who were ages 65 and older, were enrolled in fee-for-service Medicare, and had at least one claim with a diagnosis of depression between 1992 and 1999. Sixty-eight percent of the final sample lived in metropolitan areas, and 73% were female.
Episode of Care
We used an episode-of-care framework to analyze psychotherapy treatment for depression. Agency for Health Care Policy and Research guidelines (20) recommend a minimum of 4–9 months of continuous treatment after a diagnosis of depression. Based on depression diagnosis dates, we defined each episode to be at least 6 months from the date of the initial depression diagnosis. To allow for varying length of individual treatment episodes, after the minimum period of 6 months, lack of a subsequent claim with a depression diagnosis for at least 8 weeks indicated the end of an episode. Length of episodes varied from 6 months to 35 months. This approach is consistent with the identification of fixed and varying length episodes in previous research (21–23). Episodes observed for less than 6 months were excluded from the analysis. Excluded episodes consisted of those in which the individuals died (N=20) or had their initial depression diagnosis within 6 months before the end of the study period (N=496).
Measures
Depression diagnosis was identified through ICD-9-CM/DSM-IV diagnosis codes (296.2, 296.3, 300.4, and 311) recorded in the Medicare claim files. On the basis of our episode-of-care approach, the sampling criteria captured 2,025 episodes.
Use of psychotherapy was identified by using physician’s current procedure terminology (Physician’s Current Procedural Terminology, 4th ed. [CPT-4]) and Health Care Financing Administration Common Procedure Coding System codes in the Medicare physician/supply claims. Psychotherapy was defined broadly, by using codes in the range from 90841 to 90857 for 1992 through 1999. In addition, codes ranging from H5010 to H5025 were included for 1992–1997 data; codes 90875, 90876, and 90880 were included for 1993–1999 data; and codes ranging from G0071 to G0094 were included for 1997–1999 data.
Guidelines recommend that treatment for major depression continue for 4–9 months (20). Therefore, we defined consistent psychotherapy use as extending for at least two-thirds of the total months of an episode.
Demographic characteristics included gender, age, race, and living arrangement. Patients were categorized into two groups on the basis of age: 65–74 years, and 75 years and older. Race was classified as white versus nonwhite. Living arrangements were categorized as living alone, living with spouse, and living with others.
Economic characteristics included education, poverty status, pharmacy coverage, and supplemental insurance coverage. On the basis of completed years of schooling, education was categorized as no college or college. “Low income” was defined as the respondent’s personal income, or joint income if married, below 200% of the family-size-adjusted federal poverty level (24). Type of prescription drug insurance coverage was derived from survey responses about monthly drug coverage and included five possible types of private plans, Medicaid, and other public plans. A supplemental insurance variable was created to indicate whether the individual was covered for at least 1 month under any of the following insurance plans: private plans, other public plans, health maintenance organization (HMO) coverage, Medicaid, and Qualified Medicare Beneficiary/Specified Low-Income Medicare Beneficiary coverage.
Environmental variables included characteristics of the health care delivery system, external environment, and community. Person-level area of residence was classified as living in or near “metropolitan” areas versus “nonmetropolitan” areas. Two binary variables were created from Area Resource File data to measure availability of a psychiatrist and a mental health center in the county where the patient lived.
Health care professionals who treated patients during the psychotherapy treatment episodes were categorized by clinical specialty: only psychiatrists, psychiatrists and others, and only others. Other health care professionals included psychologists, social workers, and general practitioners.
Previous studies have suggested that treatment with antidepressant medications increases responsiveness, motivation, and accessibility to psychotherapy (25, 26). We defined medication management visits (CPT-4 code 90862) as those including no more than minimal medical psychotherapy.
Health status variables included self-perceived health and number of comorbid conditions. Both are ordinal variables, and higher values imply lower health status. Health perceptions were classified as 1) excellent or very good, 2) good, and 3) fair or poor. The number of comorbid conditions was measured by respondents’ self-reports about whether they had ever been told by a doctor that they had heart disease, diabetes, cancer, stroke, arthritis, hypertension, emphysema, osteoporosis, or Alzheimer’s disease. The number of comorbid conditions was categorized into three groups: 1) none to one, 2) two to four, and 3) five or more.
Year of diagnosis was included to account for changes in available treatments and practice patterns, with 1992 as the reference year.
Statistical Methods
The chi-square statistic was used to test unadjusted group differences in rates of psychotherapy and their consistency. Multiple logistic regressions were performed to determine the effect of each covariate on the odds of receiving psychotherapy during an episode of depression treatment and, if psychotherapy was used, the odds of receiving consistent psychotherapy.
Given the design of the Medicare Current Beneficiary Survey data and our definition of episode, an individual could be followed for a maximum of 4 years and contribute up to six episodes. Because the Medicare Current Beneficiary Survey assigns weights by calendar year, for episodes that spanned multiple years we used only the baseline weights. In the statistical analysis, we estimated standard errors by using linearization methods that account for intracluster correlation within geographically based primary sampling units in the multilevel sampling design utilized by the Medicare Current Beneficiary Survey. All analyses were conducted with SAS-callable SUDAAN statistical software system to take account of the complex design (27).
Sensitivity Analysis
Because an episode of treatment could begin before the start of the study period or end after the end of the study period, both left-censored and right-censored episodes were possible. To examine censoring, we performed sensitivity analyses by excluding episodes that began during the first available 8 weeks of the first survey year or ended during the last available 8 weeks of the last survey year. The results from the chi-square tests and multiple logistic regressions with these exclusions were consistent with our findings and therefore are not reported here.
Results
Use of Psychotherapy
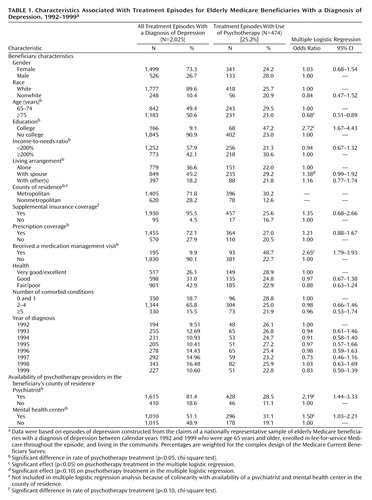
Table 1 displays the composition of the sample of Medicare beneficiaries with a diagnosis of depression during the study period. We identified 2,025 episodes of depression among 1,542 unique beneficiaries with a diagnosis of depression; 1,178 individuals had one episode, 270 had two episodes, and 94 had three or more episodes. A majority of the episodes occurred among female beneficiaries, whites, and individuals with no college. Overall 25% (N=474) of the episodes had any use of psychotherapy for depression. (The percentage was weighted for the complex design of the Medicare Current Beneficiary Survey.) No significant difference in rate of psychotherapy across years was found. This finding held when the year of treatment was entered as a continuous variable (results not shown), indicating the absence of a time trend.
There were significant differences in rates of psychotherapy by age, education, income, living arrangement, availability of local providers, medication management, and prescription coverage. A higher proportion of psychotherapy use was found in the younger elderly group than in the older group, beneficiaries with college than in those with no college, in higher-income than in low-income beneficiaries, in those living with spouse than in those living alone or with others, and in metropolitan than in nonmetropolitan residents. Older adults living in a county where a psychiatrist or a mental health center was available were more likely to use psychotherapy, as were those who ever had medication management visits during the episodes and those who had prescription drug coverage.
Findings from the multiple logistic regression confirmed the results from the chi-square tests (Table 1). County of residence was excluded from the model because of its colinearity with local provider supplies. The income effect became insignificant once education was entered. College-educated older adults were more than twice as likely to receive psychotherapy than those with no college (odds ratio=2.72, 95% confidence interval [CI]=1.67–4.43). Older adults who received medication management during the episode were more than twice as likely to receive psychotherapy as those who did not (odds ratio=2.65, 95% CI=1.79–3.93). Availability of a psychiatrist or a mental health center in the county where the patient lived also increased the odds of receiving psychotherapy about twofold (availability of a psychiatrist: odds ratio=2.19, 95% CI=1.79–3.93; availability of a mental health center: odds ratio=1.50, 95% CI=1.03–2.21). Prescription drug coverage also did not significantly affect the likelihood of using psychotherapy, when other factors were taken into account.
Consistency of Psychotherapy
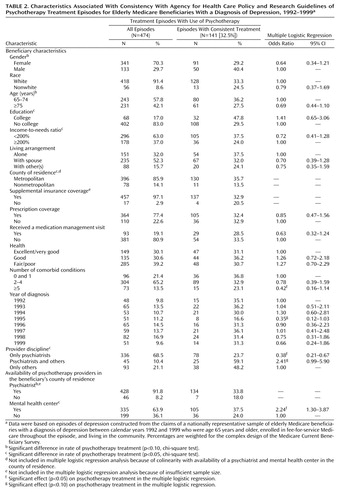
Table 2 shows the results for consistency of psychotherapy. Overall, 33% of the psychotherapy treatment episodes were consistent with guideline recommendations. Chi-square tests showed significant differences in consistency by education attainment, income, county of residence, provider discipline, and local provider supplies. Older adults with no college were less likely to receive consistent psychotherapy, as were nonmetropolitan residents and low-income persons. Psychiatrists alone provided psychotherapy in almost 70% of the total episodes, but the patients they treated were significantly less likely to receive consistent psychotherapy than those who received at least some psychotherapy from other health care professionals. Beneficiaries living in a county with a mental health center were significantly more likely to receive consistent psychotherapy than those who did not.
There were few differences in findings between the chi-square tests and the multiple logistic regressions (Table 2). With adjustment for other factors, users’ socioeconomic and demographic characteristics no longer affected the likelihood of receiving consistent psychotherapy. In contrast, provider-supply effects were persistent. Older patients treated only by psychiatrists were significantly less likely to receive consistent psychotherapy than those treated by other professionals (odds ratio=0.38, 95% CI=0.21–0.67), and a combination of psychiatrists and other professionals increased the likelihood of receiving consistent psychotherapy (odds ratio=2.41, 95% CI=0.99–5.90). Availability of a mental health center in the county where the patient lived increased the odds of receiving consistent psychotherapy about twofold (odds ratio=2.24, 95% CI=1.30–3.87).
Discussion
Despite substantial empirical evidence supporting the efficacy of psychotherapy for depression in older adults, our study showed that only a minority of depressed elderly patients received psychotherapy. This finding is consistent with findings in previous studies (28). Overall, psychotherapy use remained stable at this low level between 1992 and 1999, although antidepressant use in this population increased during this period (29).
Although education and income are indicators of socioeconomic status, in the multiple logistic regression only education was related to psychotherapy use. College-educated older adults were more likely to use psychotherapy than were those with no college. Previous research with groups of nonelderly subjects has found that acceptance of psychotherapy is directly related to level of education (30). Psychiatrists initiating treatment of depression for older patients should bear in mind that their patients who have not attended college may tend to be less accepting of psychotherapy than those with higher educational attainment. The selection of treatment modality should be influenced by the patient’s preferences as well as clinical considerations such as symptom severity, the presence of interpersonal difficulties, or a comorbid axis II disorder (31). With older patients who have less formal education, it may be especially important for psychiatrists to discuss how psychotherapy works and remain responsive to patients’ concerns or misconceptions regarding this treatment.
In our study, environmental factors significantly affected use and consistency of psychotherapy. Our findings suggest that older Americans face significant barriers in access to psychotherapy because of limited local availability of qualified providers (21).
Provider discipline played an important role in affecting the likelihood of receiving consistent psychotherapy. Patients who received psychotherapy only from psychiatrists were less likely to receive psychotherapy for the period of time recommended by Agency for Health Care Policy and Research guidelines. Because a great majority of the medication management visits were provided by psychiatrists, psychotherapy may be used by psychiatrists to supplement pharmacotherapy, rather than as a primary treatment. Costs may also contribute to the observed psychotherapy utilization pattern. Given that a majority of the patients had prescription drug coverage and that Medicare covers 80% of medication management visit payments (32), patients who are treated with antidepressant medications incur lower copayments than those who receive psychotherapy. Psychologists and social workers also have substantially lower fee schedules than psychiatrists (33).
The risk of early termination may be greater for patients under the care of psychiatrists in solo practice than for patients treated by psychiatrists in mental health centers or multidisciplinary groups. Psychiatrists who have institutionalized referral relationships with nonpsychiatrist psychotherapists may have an advantage in maintaining their older patients through the continuation and maintenance phases of psychotherapy for depression. Therefore, higher financial barriers to treatment, differences in rates of antidepressant treatment, and variation in psychotherapy orientations may help to explain the low rates of consistent psychotherapy among patients who received psychotherapy only from psychiatrists.
The study has some important limitations. Coding biases are likely to affect the sensitivity, more than the specificity, of diagnosis (34–36). Therefore, our study may have underestimated the overall number of depressive episodes. The sample includes only non-HMO and non-institution-dwelling Medicare beneficiaries, and so the findings cannot be generalized to HMO and institution-dwelling populations. The Medicare Current Beneficiary Survey data provide only event-level information on prescription drug use, and thus we were unable to determine precise dates of antidepressant use. Most important, Medicare Current Beneficiary Survey data provide no information on the types of psychotherapy being provided (e.g., cognitive behavior, interpersonal, nonspecific supportive) or on their clinical effectiveness.
Despite these limitations, our study provides important information on use of psychotherapy among elderly patients with a diagnosis of depression. The findings confirm that use of psychotherapy is influenced by a host of factors at the patient, provider, and health care system levels.
 |
 |
Received March 19, 2003; revision received Feb. 10, 2004; accepted June 1, 2004. From the Institute for Health, Health Care Policy, and Aging Research, Rutgers University; and the Department of Psychiatry, Columbia University, New York State Psychiatric Institute. Address correspondence and reprint requests to Dr. Wei, Institute for Health, Health Care Policy, and Aging Research, Rutgers University, 30 College Ave., New Brunswick, NJ 08901; [email protected] (e-mail). Supported by NIMH grants MH-60831 and MH-43450, grants HS-11825 and HS-09566 from the Agency for Healthcare Research and Quality, and grant AG-15166 from the National Institute on Aging. The findings and opinions reported here are those of the authors and do not necessarily represent the views of any other individuals or organizations. The authors thank Rizie Kumar, M.A., and Vatsala Karwe, Ph.D., for programming assistance, Michelle Kennedy for research assistance, and the Centers for Medicaid and Medicare Services for making the data available.
1. Lebowitz BD, Pearson JL, Schneider LS, Reynolds CF III, Alexopoulos GS, Bruce ML, Conwell Y, Katz IR, Meyers BS, Morrison MF, Mossey J, Niederehe G, Parmelee P: Diagnosis and treatment of depression in late life: consensus statement update. JAMA 1997; 278:1186–1190Crossref, Medline, Google Scholar
2. NIH consensus conference on diagnosis and treatment of depression in late life. JAMA 1992; 268:1018–1024Crossref, Medline, Google Scholar
3. Diagnosis and Treatment of Depression in Late Life: National Institutes of Health Consensus Development Conference, Nov 4–6, 1991. Consens Statement 1991; 9:1–27Google Scholar
4. Unutzer J, Katon W, Callahan CM, Williams JW Jr, Hunkeler E, Harpole L, Hoffing M, Della Penna RD, Noel PH, Lin EH, Arean PA, Hegel MT, Tang L, Belin TR, Oishi S, Langston C (IMPACT Investigators): Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA 2002; 288:2836–2845Crossref, Medline, Google Scholar
5. Cronin-Stubbs D, Mendes de Leon CF, Beckett LA, Field TS, Glynn RJ, Evans DA: Six-year effect of depressive symptoms on the course of physical disability in community-living older adults. Arch Intern Med 2000; 160:3074–3080Crossref, Medline, Google Scholar
6. Rovner BW, German PS, Brant LJ, Clark R, Burton L, Folstein MF: Depression and mortality in nursing homes. JAMA 1991; 265:993–996; correction, 265:2672Crossref, Medline, Google Scholar
7. Reynolds CF III, Frank E, Perel JM, Imber SD, Cornes C, Miller MD, Mazumdar S, Houck PR, Dew MA, Stack JA, Pollock BG, Kupfer DJ: Nortriptyline and interpersonal psychotherapy as maintenance therapies for recurrent major depression: a randomized controlled trial in patients older than 59 years. JAMA 1999; 281:39–45Crossref, Medline, Google Scholar
8. Keller MB, McCullough JP, Klein DN, Arnow B, Dunner DL, Gelenberg AJ, Markowitz JC, Nemeroff CB, Russell JM, Thase ME, Trivedi MH, Zajecka J: A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. N Engl J Med 2000; 342:1462–1470; correction, 2001; 345:232Google Scholar
9. Scogin F, McElreath L: Efficacy of psychosocial treatments for geriatric depression: a quantitative review. J Consult Clin Psychol 1994; 62:69–74Crossref, Medline, Google Scholar
10. Reynolds CF III: Treatment of major depression in later life: a life cycle perspective. Psychiatr Q 1997; 68:221–246Crossref, Medline, Google Scholar
11. Padgett DK, Burns BJ, Grau LA: Risk factors and resilience: mental health needs and services use of older women, in Women’s Mental Health Services: A Public Health Perspective. Edited by Levin BL, Blanch AK, Jennings A. Thousand Oaks, Calif, Sage Publications, 1998, pp 391–413Google Scholar
12. Arean PA, Cook BL: Psychotherapy and combined psychotherapy/pharmacotherapy for late life depression. Biol Psychiatry 2002; 52:293–303Crossref, Medline, Google Scholar
13. Anderson RJ, Freedland KE, Clouse RE, Lustman PJ: The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care 2001; 24:1069–1078Crossref, Medline, Google Scholar
14. Mendes de Leon CF, Krumholz HM, Seeman TS, Vaccarino V, Williams CS, Kasl SV, Berkman LF: Depression and risk of coronary heart disease in elderly men and women: New Haven Established Populations for the Epidemiologic Studies of the Elderly (EPESE), 1982–1991. Arch Intern Med 1998; 158:2341–2348Crossref, Medline, Google Scholar
15. Lin EH, Von Korff M, Katon W, Bush T, Simon GE, Walker E, Robinson P: The role of the primary care physician in patients’ adherence to antidepressant therapy. Med Care 1995; 33:67–74Crossref, Medline, Google Scholar
16. Landerman LR, Burns BJ, Swartz MS, Wagner HR, George LK: The relationship between insurance coverage and psychiatric disorder in predicting use of mental health services. Am J Psychiatry 1994; 151:1785–1790Link, Google Scholar
17. Simon GE, Grothaus L, Durham ML, VonKorff M, Pabiniak C: Impact of visit copayments on outpatient mental health utilization by members of a health maintenance organization. Am J Psychiatry 1996; 153:331–338Link, Google Scholar
18. Alvidrez J, Arean PA: Physician willingness to refer older depressed patients for psychotherapy. Int J Psychiatry Med 2002; 32:21–35Crossref, Medline, Google Scholar
19. Landreville P, Landry J, Baillargeon L, Guerette A, Matteau E: Older adults’ acceptance of psychological and pharmacological treatments for depression. J Gerontol B Psychol Sci Soc Sci 2001; 56:285–291Crossref, Medline, Google Scholar
20. Agency for Health Care Policy and Research: Depression in Primary Care, vol 2: Treatment of Major Depression: Clinical Practice Guideline 5: Publication 93–0550. Washington, DC, US Department of Health and Human Services, 1993Google Scholar
21. Ettner SL, Hermann RC, Tang H: Differences between generalists and mental health specialists in the psychiatric treatment of Medicare beneficiaries. Health Serv Res 1999; 34:737–760Medline, Google Scholar
22. Keeler EB, Manning WG, Wells KB: The demand for episodes of mental health services. J Health Econ 1988; 7:369–392Crossref, Medline, Google Scholar
23. Kessler LG, Steinwachs DM, Hankin JR: Episodes of psychiatric utilization. Med Care 1980; 18:1219–1227Crossref, Medline, Google Scholar
24. US Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation: Prior HHS Poverty Guidelines and Federal Register References. http://aspe.hhs.gov/poverty/figures-fed-reg.shtmlGoogle Scholar
25. Hirschfeld RM, Dunner DL, Keitner G, Klein DN, Koran LM, Kornstein SG, Markowitz JC, Miller I, Nemeroff CB, Ninan PT, Rush AJ, Schatzberg AF, Thase ME, Trivedi MH, Borian FE, Crits-Christoph P, Keller MB: Does psychosocial functioning improve independent of depressive symptoms? a comparison of nefazodone, psychotherapy, and their combination. Biol Psychiatry 2002; 51:123–133Crossref, Medline, Google Scholar
26. Segal Z, Vincent P, Levitt A: Efficacy of combined, sequential and crossover psychotherapy and pharmacotherapy in improving outcomes in depression. J Psychiatry Neurosci 2002; 27:281–290Medline, Google Scholar
27. Shah BV, Barnwell BG, Bieler GS: SUDAAN User’s Manual, Release 7.5. Research Triangle Park, NC, Research Triangle Institute, 1997Google Scholar
28. Olfson M, Marcus SC, Druss B, Pincus HA: National trends in the use of outpatient psychotherapy. Am J Psychiatry 2002; 159:1914–1920Link, Google Scholar
29. Crystal S, Sambamoorthi U, Walkup JT, Akincigil A: Diagnosis and treatment of depression in the elderly Medicare population: predictors, disparities and trends. J Am Geriatr Soc 2003; 51:1718–1728Crossref, Medline, Google Scholar
30. Furnham A, Wardley Z: Lay theories of psychotherapy, I: attitudes toward, and beliefs about, psychotherapy and therapists. J Clin Psychol 1990; 46:878–890Crossref, Medline, Google Scholar
31. American Psychiatric Association: Practice Guideline for the Treatment of Patients With Major Depressive Disorder (Revision). Am J Psychiatry 2000; 157(April suppl)Google Scholar
32. Sharfstein SS, Goldman H: Financing the medical management of mental disorders. Am J Psychiatry 1989; 146:345–349Link, Google Scholar
33. Dewan M: Are psychiatrists cost-effective? an analysis of integrated versus split treatment. Am J Psychiatry 1999; 156:324–326Abstract, Google Scholar
34. Fowles JB, Lawthers AG, Weiner JP, Garnick DW, Petrie DS, Palmer RH: Agreement between physicians’ office records and Medicare Part B claims data. Health Care Financ Rev 1995; 16:189–199Medline, Google Scholar
35. Robbins JM, Kirmayer LJ, Cathebras P, Yaffe MJ, Dworkind M: Physician characteristics and the recognition of depression and anxiety in primary care. Med Care 1994; 32:795–812Crossref, Medline, Google Scholar
36. Lurie N, Popkin M, Dysken M, Moscovice I, Finch M: Accuracy of diagnoses of schizophrenia in Medicaid claims. Hosp Community Psychiatry 1992; 43:69–71Abstract, Google Scholar



