Specialized Inpatient Trauma Treatment for Adults Abused as Children: A Follow-Up Study
Abstract
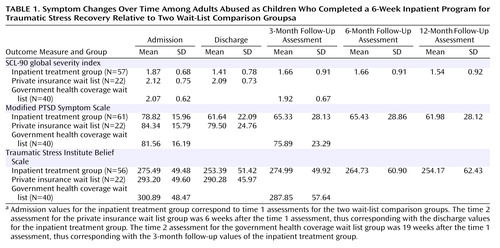
OBJECTIVE: The authors investigated outcome at discharge and at follow-up assessments for adults abused as children who completed a 6-week inpatient program for traumatic stress recovery. METHOD: Participants were assessed at admission, discharge, and 3, 6, and 12 months postdischarge on measures of global symptom severity, posttraumatic stress disorder (PTSD), and disrupted beliefs. Two wait-list comparison groups were also assessed at two points in time for comparison with the discharge and 3-month postdischarge assessments of the treatment group. RESULTS: Relative to admission, the mean scores on all outcome measures for the treatment group were improved at discharge and at 6 and 12 months. Relative to a wait list group, the treatment group was significantly improved at discharge. After 3 months, the scores for the treatment group were not different from those of a wait list group because of deterioration in the treatment group. Age, source of income, and number of axis II disorders were associated with differing patterns of PTSD symptom change over time. Between 32% and 45%, depending on outcome measure, met stringent criteria for clinically significant change at 12 months postdischarge. CONCLUSIONS: At discharge from a specialized inpatient treatment program, adults with a history of abuse during childhood showed improvement relative to a wait list group. Scores tended to deteriorate in the 3 months following discharge but rebounded to discharge levels by 12 months postdischarge. Although many abused adults benefited from specialized inpatient treatment, a substantial proportion did not show clinically significant change 1 year later.
Research into the effectiveness of specialized, trauma-focused inpatient programs for adults abused as children is very limited, and the studies that have been published have had methodological limitations (1). Findings from studies of combat veterans with chronic posttraumatic stress disorder (PTSD) may be seen as relevant, since abused adults are frequently diagnosed with chronic PTSD. Studies of specialized inpatient treatment of veterans with chronic PTSD, especially long-stay programs (>90 days), have suggested that this form of treatment is not an effective form of intervention (2, 3). However, it has been recognized that generalizing from veterans to a population of primarily female abused adults is risky (4).
The few studies that have investigated outcome for abused adults following specialized inpatient treatment suggest that abused adults may respond better than veterans and that, at least for some, it may be the treatment of choice (5). An outcome study of women with histories of child abuse, after varying lengths of specialized inpatient trauma treatment, found substantial improvement at discharge; relapse in some symptom areas was reported at a 12-month follow-up evaluation, but the group tended to maintain treatment gains. A substantial minority, however, continued to show severe impairment at the follow-up assessment (5). Another study reported that patients with dissociative identity disorder were markedly improved 2 years after a stay in a specialized inpatient program (6). An earlier uncontrolled study in the same treatment setting as the study reported here found that abused adults showed reduced PTSD symptoms at discharge from the 6-week inpatient trauma program. Some decay of gains at a 3-month follow-up assessment were noted, but the study group returned to improved levels at 1 year (7).
These previous studies of abused adults have methodological limitations in that none included a control or comparison group, and the study by Allen et al. (5) did not assess PTSD symptoms. The study reported here improves on previous methodologies by including assessment of PTSD symptoms and comparing the outcomes of adults who completed an inpatient program with those on wait lists for the same program.
Treatment Program
The Program for Traumatic Stress Recovery is offered in a psychiatric hospital located in a small city in Ontario, Canada. Approximately 80% of those admitted have private extended health insurance, which covers the cost of the accommodation. Those with only government health insurance coverage are able to access a small number of places in the program. The 6-week program is an adaptation of Bloom’s Sanctuary Model (8). It assumes a relationship between reported childhood trauma and later adult psychological disturbance but is present centered, and the focus is on separating the past from the present and learning to live in the here and now. A multidisciplinary team provides the 6-week inpatient program, which focuses on safety, the first stage of Herman’s trauma treatment model (9); participants are told that further trauma treatment will likely be required. Much of the treatment is offered in a group format within a therapeutic community model (10) and includes education and skills training groups, insight-oriented process groups, and creative arts therapy groups. Planning for life after discharge from the program, and transfer of new skills and understanding to the home environment, are given considerable emphasis.
Method
Participants
The treatment group was recruited from 272 men and women consecutively admitted to the Program for Traumatic Stress Recovery between September 1998 and February 2000 who had reported a history of childhood abuse (physical, sexual, or emotional). After complete description of the study, written informed consent was obtained from 218 patients (80%). Participants were assessed at five points in time (admission, discharge, 3 months postdischarge, 6 months postdischarge, and 12 months postdischarge).
The participants in the wait-list comparison groups were assessed at two points in time. The first comparison group was recruited from the wait list of those with private insurance, for whom the wait was about 2 months. Their two assessments were 6 weeks apart (which corresponded to the length of the inpatient treatment). The second comparison group was recruited from the wait list of those who had only government health coverage, for whom the wait for admission could be up to 2 years. Their two assessments were 19 weeks apart (which corresponded to the time period between admission and the 3-month postdischarge assessment for the treatment group). Although this design is an improvement on previous studies, an ideal design would have included additional testing of a wait-list comparison group at times that corresponded to the 6- and 12-month postdischarge assessments of the treatment group.
From the private insurance wait list, 42 (40% of those receiving letters requesting their participation) gave written informed consent to participate. From the government health coverage wait list, 74 (47% of those receiving letters) consented to participate. Thirty-one (74%) and 58 (78%) participants from the two wait list groups, respectively, returned time 2 data.
Exploration of the data revealed that the treatment group and the wait-list comparison groups were not equivalent in terms of score on the Modified PTSD Symptom Scale: the treatment group included 33 participants (17% of those completing the measure at admission) who scored below 51 on this self-report measure of PTSD symptoms. A score below 51 is within one standard deviation of the mean for a community sample (11) and was lower than any of the scores of participants in the private insurance wait list group. Consequently, participants with scores below 51 were not included in the analysis. Using this criterion, the treatment group comprised 119 participants at discharge, 89 at 3 months postdischarge, 82 at 6 months postdischarge, and 68 at 12 months postdischarge. The government health coverage wait list group was reduced by six subjects to 52. No differences were found in terms of gender, age, marital status, education, main source of family income, annual family income, or type of reported child abuse between participants with admission PTSD scores below 51 and those with PTSD scores above 50.
Measures
Demographic data and history of childhood abuse were collected through self-report questionnaires that were adaptations of those designed for a previous study (12). The Trauma Assessment for Adults–Self-Report (13) assessed lifetime exposure to potentially traumatic events. This questionnaire asks whether participants have experienced any of 14 traumatic event categories in their lifetime. Examples are having been in a serious accident or having been attacked with a weapon.
Outcome measures included the SCL-90 (14), a well-validated instrument of 90 items rated on a 5-point scale. It provides a global severity index, which combines information on the number of symptoms and intensity of perceived distress, and is “the best single indicator of the current level or depth of the disorder” (14, p. 14). The Modified PTSD Symptom Scale was given to assess the frequency and severity of DSM-IV PTSD symptoms, using 17 items with a 4-point scale for frequency and a 5-point scale for severity. An earlier version demonstrated good internal consistency with both treatment and community samples (0.97 and 0.96, respectively) and good concurrent validity with the Structured Clinical Interview for the DSM-III-R PTSD module (15). The Traumatic Stress Institute Belief Scale, Revision L (16) assessed cognitive schemata in psychological need areas that are hypothesized to be sensitive to traumatic experiences. It has 80 items rated on a 6-point scale. Adequate internal consistency has been demonstrated with clinical and student populations, ranging from 0.70 to 0.96. Validity is shown by significant differences in expected directions between nonclinical, outpatient, and chronic patient groups.
Variables Potentially Affecting Treatment
Axis II comorbidity
Within 4 weeks of admission, one of us (D.C.W.) administered the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) (17) to 100 patients randomly selected from the participants recruited for the treatment group. A second psychiatrist assessed the first 10 participants, in order to establish interrater reliability (kappa=0.88, p<0.001) before the remainder were assessed.
Postdischarge professional help
At each follow-up point, participants reported the number of visits to helping professionals in the interval since the previous testing.
Inpatient experience
At 6 months postdischarge, 30 of the participants, selected if they lived within a 2-hour drive of the hospital, were interviewed about their experience of the inpatient treatment. Similar proportions of those who were maintaining gains and not maintaining gains on the standardized measures at 3-month follow-up were included.
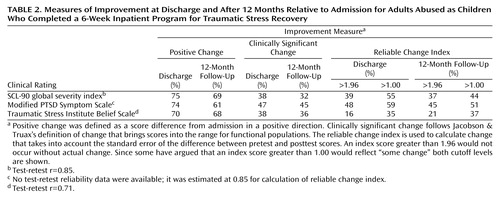
Measures of Improvement
Positive change was deemed to have occurred when the difference between admission scores and those at discharge and 12-month follow-up indicated change in a positive direction. Clinically significant change was calculated by using the definition of Jacobson and Truax (18): change that brings scores into the range for functional populations. It was calculated by using the following functional population norms: for the SCL-90 global severity index, those reported by Derogatis (14) for nonpatient normal subjects (mean=0.31, SD=0.31); for the Traumatic Stress Institute Belief Scale, norms reported by Pearlman (personal communication, 2001) for college students (mean=192.41, SD=43.39); for the Modified PTSD Symptom Scale, those reported by Falsetti (11) for a community sample (mean=30.78, SD=20.33). Reliable change was calculated based on Jacobson and Truax’s formula (18), which takes into account the standard error of the difference between pretest and posttest scores.
Results
Demographic Characteristics
The participants in the treatment group ranged from 18 to 66 years of age with a mean age of 40 years. Eighty-eight percent lived in Ontario, and 87% were born in Canada. Eight percent identified themselves as belonging to a minority group. Women made up 84% of the group, 58% were married or living with a partner, and 25% were separated, divorced, or widowed. Only 23% had secondary school or less education, with 47% being graduates of a college or university and 29% reporting that they had attended a college or university. Thirty-five percent reported that they had been employed prior to admission, but 44% were on sick leave, and the remainder were homemakers, students, or unemployed. Twenty-eight percent reported an annual family income of $30,000 or less, 27% were in the $31,000–$60,000 range, 21% were in the $61,000–$80,000 range, and 26% reported family income above $81,000 (all amounts expressed in Canadian dollars).
Clinical Characteristics
The category of lifetime traumatic events most often endorsed was “coerced sex before age 18 years” (76%). The mean number of event types experienced in which the participant felt at risk of serious injury or death was 4.6 (SD=0.24). Seventy-six percent of the treated group reported having been physically abused as a child (<16 years), 74% reported child sexual abuse, and 61% reported that they had experienced physical, sexual, and emotional abuse.
Seventy percent of the subjects reported that they had been hospitalized previously for psychological reasons, and 40% reported two or more prior hospitalizations. Thirty-eight percent of the participants assessed with the SCID-II did not meet criteria for any axis II disorder. Twenty-eight percent met criteria for one axis II disorder, and the remainder met criteria for two or more.
At 12 months postdischarge, the median number of visits to helping professionals (psychiatrists, psychologists, social workers, clergy, and social agencies) since discharge was 44, the mean was 45.3, and the number of visits ranged from six to 118.
Analysis of Treatment Group Over Time
Because the wait-list comparison groups were tested at fewer time points than the treatment group, a repeated-measures multivariate test including the three groups at all testing points was not possible. Repeated-measures multivariate analysis of variance (MANOVA) was performed on the scores from the treatment group on the three outcome measures at the five points in time. The analysis yielded a significant main effect for time (Pillai’s trace=0.633, F=5.173, df=12, 36, p<0.001), indicating that the within-subject differences on the three outcome measures across the time periods were significant (SCL-90 global severity index: F=5.701, df=4, 188, p<0.001; Modified PTSD Symptom Scale: F=8.665, df=4, 188, p<0.001; Traumatic Stress Institute Belief Scale: F=4.450, df=4, 188, p<0.001).
Repeated-measures univariate tests were conducted for each dependent variable separately to determine where the differences in means existed, given the overall multivariate significance. Univariate tests also reduced the amount of missing data compared with the multivariate test. The means and standard deviations from the univariate analyses are illustrated in Table 1. On the SCL-90 global severity index, relative to admission, the mean was improved at discharge (mean difference=0.46 [p<0.001]) and at all follow-up points (3 months: mean difference=0.21 [p<0.04]; 6 months: mean difference=0.21 [p<0.03]; 12 months: mean difference=0.33 [p=0.001]). Similarly, on the Modified PTSD Symptom Scale, pairwise comparisons revealed that, relative to admission, the mean was improved at discharge (mean difference=17.18 [p<0.001]) and at all follow-up points (3 months: mean difference=13.49 [p<0.001]; 6 months: mean difference=13.39 [p<0.001]; 12 months: mean difference=16.84 [p<0.001]).
On the Traumatic Stress Institute Belief Scale, a different pattern was observed: relative to admission, the mean at discharge was improved (mean difference=22.10 [p=0.001]). However, at 3 months, the mean was not different from admission. At 6 months, it was marginally improved (mean difference=10.76 [p<0.10]), and at 12 months it was significantly better than at admission (mean difference=21.32 [p=0.008]).
Comparison of Treatment and Wait List Groups
The private insurance wait list group and the treatment group were equivalent on all demographic variables except main source of family income: 32% of this wait list group reported their own salary/wages, partner’s income, or investments as the main source of family income compared with 70% of the treatment group. No significant difference was found between the two groups in terms of annual family income. Repeated-measures MANOVA was performed to compare the treatment group (N=103) at admission and discharge with the private insurance wait list group (N=22) at time 1 and time 2 (6 weeks apart) on the three outcome measures. The interaction of group and time was significant (Pillai’s trace=0.074, df=3, 121, p<0.03). Univariate tests indicated that the group-by-time interaction was significant for all three outcome measures. Four covariates (gender, age, marital status, and annual family income) were entered into the same analysis, and the group-by-time interaction remained significant (Pillai’s trace=0.094, df=3, 110, p<0.02).
Univariate tests indicated that the group-by-time interaction was significant for all three outcome measures (SCL-90 global severity index: F=11.401, df=1, 112, p=0.001; Modified PTSD Symptom Scale: F=4.938, df=1, 112, p<0.03; Traumatic Stress Insititute Belief Scale: F=4.663, df=1, 112, p<0.04). These findings indicate that at discharge, the participants in the treatment group were significantly more improved than the private insurance wait list group at time 2.
The government health coverage wait list group and the treatment group were equivalent on all demographic variables except marital status and main source of family income: those in the treatment group were more likely to be married or living with a partner (59% versus 30%), and those in the treatment group were more likely to name salary/wages, partner’s income, or investments as the main source of family income (71% versus 35%). The treatment group was also more likely to have an annual family income over $30,000 than the government health coverage wait list group (71% versus 31%).
A repeated-measures MANOVA was performed to compare the treatment group (N=74) at admission and 3 months postdischarge with the government health coverage wait list group (N=40) at time 1 and time 2 (19 weeks apart) on the three outcome measures. The interaction for group and time was significant (Pillai’s trace=0.08, df=3, 110, p<0.03). Univariate tests indicated that the group-by-time interaction was significant for the Modified PTSD Symptom Scale but not for the other two outcome measures. When gender and age were entered as covariates, the results were similar (Pillai’s trace=0.075, df=3, 107, p<0.04). Marital status and annual family income were not significant covariates. These findings suggest that the treatment group at 3 months postdischarge and the government health coverage wait list group after 19 weeks were not significantly different.
Effects of Demographic and Clinical Variables on Treatment Group Outcome
Age, gender, marital status, source of income, annual family income, axis II comorbidity, and number of visits to helping professionals between discharge and the 12-month follow-up assessment were entered separately into the repeated-measures MANOVA assessing change over time for the treatment group to see if any of these variables interacted with the time factor. Figure 1 shows that age significantly interacted with score on the Modified PTSD Symptom Scale (F=4.03, df=2, 57, p<0.03). Participants 29 years or younger were more likely to report an abrupt increase in PTSD symptoms at 3 months than were older participants. The mean for participants over 50 years did not increase at 3 months at all, suggesting that older participants may experience the return home differently from younger participants.
Figure 2 shows that age also interacted with score on the SCL-90 global severity index (F=3.46, df=2, 53, p<0.04). Although the oldest group had the highest mean global severity index score at admission, the mean at 3 months was as low for the older group as for those 30–50 years of age. However, the mean for the older group returned to admission levels at 6 months postdischarge and was only slightly improved at 12 months postdischarge, whereas the younger age cohorts showed more improvement.
Source of income (personal salary/partner’s income/investments versus government pension/employment insurance/social assistance) significantly interacted with time for score on the Modified PTSD Symptom Scale (F=5.04, df=1, 58, p<0.03). Figure 3 shows that the pattern of change was similar for the two groups between admission and the 3-month follow-up assessment, but at 6 months, those who were supported by government pension, employment insurance, or social assistance had returned to PTSD symptom levels close to those at admission. By 12 months postdischarge this group had improved slightly but still reported considerably more PTSD symptoms than those who received income from nongovernment sources.
Annual family income significantly interacted with time for score on the Traumatic Stress Institute Belief Scale (F=4.01, df=2, 47, p<0.03), but the interaction did not appear to be clinically significant and is not illustrated here. The number of axis II disorders for which the participant met criteria also significantly interacted with time for score on the Modified PTSD Symptom Scale (F=4.325, df=1, 32, p<0.03). Figure 4 shows that those who did not meet criteria for an axis II disorder tended to maintain treatment gains at 3 months, whereas those who met criteria for two or more axis II disorders tended to show an increase in PTSD symptoms at 3 months relative to discharge. Chi-square tests of the association between number of axis II disorders and age, source of income, and annual family income were not significant.
Gender, marital status, and number of visits to helping professionals postdischarge did not interact significantly with time on any of the outcome measures.
Participants’ Perceptions of What Was Helpful
From the interviews, the following themes regarding what participants said was helpful about the program were identified: 1) interaction with staff who were respectful of participants and knowledgeable about PTSD; 2) feeling believed and validated; 3) the opportunity to work through emotional issues in a safe environment; 4) the opportunity to learn self-help skills; and 5) recognizing that others had experienced abuse similar to their own. The most commonly reported negative experience was difficulty in returning to everyday life following discharge. A more complete description of the participants’ views of what was helpful and less helpful about the inpatient treatment can be found elsewhere (19).
Improvement Measures
Table 2 illustrates the proportion of subjects in the treatment group that showed positive change relative to admission on outcome scores at discharge and at 12 months postdischarge. Between 70% and 75%, depending on the outcome measure, demonstrated change in a positive direction at discharge, and between 61% and 69% demonstrated positive change at 12 months. Using Jacobson and Truax’s definition, between 38% and 47% demonstrated clinically significant change at discharge, with similar proportions demonstrating clinically significant change at 12 months. Jacobson and Truax (18) also suggest that for changes in scores to be considered reliable, the reliable change index must be greater than 1.96, because a change larger than 1.96 would be unlikely to occur (p<0.05) without actual change. Others (20) have suggested that a reliable change index greater than 1.00 can be seen as an indication of “some gain.” The proportions of the treatment group that met these two cutoff points at discharge and at 12 months are also shown in Table 2.
Discussion
This study has demonstrated that, as a group, adults abused as children who were admitted to a specialized 6-week inpatient treatment program for traumatic stress were improved relative to admission at discharge and 6 and 12 months postdischarge. At 3 months, mean scores deteriorated somewhat compared with discharge scores, but on two of the three outcome measures, the change in a positive direction between admission and 3 months was statistically significant.
When compared with participants on a wait list, the treatment group was significantly better on all outcome measures at discharge. However, when compared at a 3-month follow-up evaluation with a different wait list group, the treatment group was better only on PTSD symptoms, and further analysis suggested that this difference was not robust.
It appears that some participants find the transition from the hospital milieu to the home environment difficult, and that symptoms and disrupted beliefs tend to increase as the participant experiences the stress of this transition. We believe that if a wait list group had been followed for a longer period, significant differences between the treatment and wait list groups would have been evident at the 6- and 12-month follow-up assessments. The following two findings support this hypothesis: 1) the mean outcome scores for the treatment group at 6 and 12 months were significantly better relative to admission; 2) the government health coverage wait list group did not change significantly over that period. However, a study that followed wait list participants for a minimum of 6 months would be required to strengthen this argument.
Interviews with participants indicated that the treatment approach involving the assumption of a connection between child abuse experiences and PTSD symptoms, interventions that encourage participants to separate the past from the present, and the teaching of self-help skills for coping with PTSD symptoms was experienced as helpful, validating, and respectful.
The relatively large size of the treatment group, assessment of PTSD symptoms, inclusion of wait-list comparison groups, and a 1-year follow-up period represent methodological improvements over prior studies of abused adults following inpatient trauma treatment. The results replicate a previous noncontrolled study (8) by again demonstrating a pattern in which participants lose some treatment gains 3 months postdischarge but regain them at 6 and 12 months postdischarge. They also support the contention of Allen et al. (5) that the clinical course following inpatient treatment may be more encouraging for adults abused as children than has been observed in studies of veterans. For abused adults who are relatively well educated and economically secure, as were the majority of the participants in this study and that of Allen et al. (5), the findings suggest a substantial proportion benefit from a specialized inpatient program.
This study also indicates that the course of recovery, especially as assessed by the Modified PTSD Symptom Scale, may vary with differences in age and income, as well as the number of axis II disorders. These findings need to be replicated with a larger sample. We can speculate that the greater deterioration from discharge of PTSD symptom improvement after 3 months for younger compared with older adults may be related to greater sensitivity to the loss of the inpatient treatment milieu or to other factors in the home environment. The finding that dependence on employment insurance or government assistance is negatively associated with the course of recovery evokes questions about whether current social policies are sufficiently supportive of individuals coping with chronic PTSD.
The finding that 39% of the study group exceeded the cutoff for reliable change on the global severity index at discharge can be compared with the 28% of combat veterans reported in an outcome study by Ford et al. (21) to meet this proportion of reliable change on the same measure following inpatient treatment. Also, in that study, only 22% reported reliable change on a different measure of PTSD symptoms, whereas the current study found that 48% had exceeded the cutoff for reliable change on PTSD symptoms. These findings also support the argument that adults with chronic PTSD associated with child abuse may respond better to specialized inpatient treatment than combat veterans.
The proportion considered improved depends on the criteria used; defining as improved those who demonstrate any amount of change in a positive direction between pre- and posttest is a liberal approach. However, the criteria developed by Jacobson and Truax seem stringent, especially in view of research suggesting that chronic PTSD is associated with structural changes in neuroanatomy (22). Expectations of this magnitude of change, at least in response to a 6-week program, are unrealistic for many individuals with this diagnosis. Whichever criterion for improvement is used, the findings support previous observations that chronic PTSD, at least for some proportion of abused adults, tends to be resistant to treatment and that the norm may be a partial rather than complete response to intervention, at least in the relatively short spans of time studied thus far (4, 23).
The field could benefit from studies of adults abused as children that compare outcomes of specialized inpatient programs with those admitted to general psychiatric units and with specialized outpatient treatment. Outpatient treatment has the possible advantage of avoiding separation from family and friends and the difficult transition to the home environment following discharge. However, such separation may be a treatment component that is necessary for many adults dealing with trauma related to child abuse.
 |
 |
Presented in part at the 16th annual conference of the International Society for Traumatic Stress Studies, San Antonio, Nov. 16–19, 2000. Received May 29, 2002; revisions received March 19, 2003, and Jan. 12, 2004; accepted May 3, 2004. From Homewood Health Centre, Guelph, Ontario, Canada. Address correspondence and reprint requests to Dr. Stalker, Faculty of Social Work, Wilfrid Laurier University, Waterloo, ONT N2L3C5, Canada. The Social Sciences and Humanities Research Council of Canada (grant 410–98-0092) and the Homewood Foundation provided funding for this study.
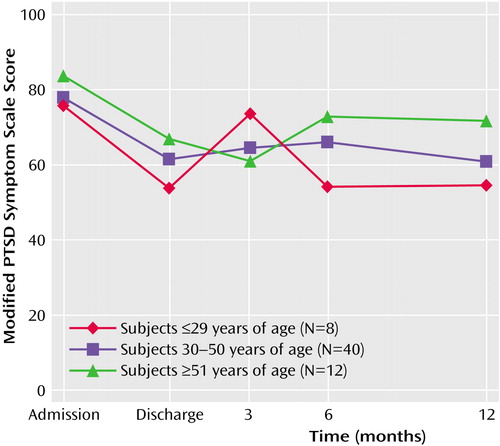
Figure 1. PTSD Symptom Level Over Time Among Adults Abused as Children Who Completed a 6-Week Inpatient Program for Traumatic Stress Recovery, by Age Group
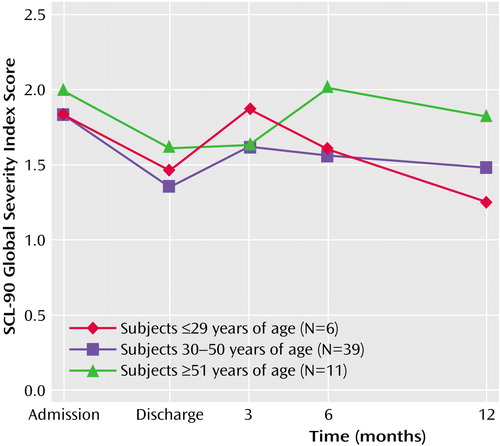
Figure 2. Psychological Symptom Severity Over Time Among Adults Abused as Children Who Completed a 6-Week Inpatient Program for Traumatic Stress Recovery, by Age Group
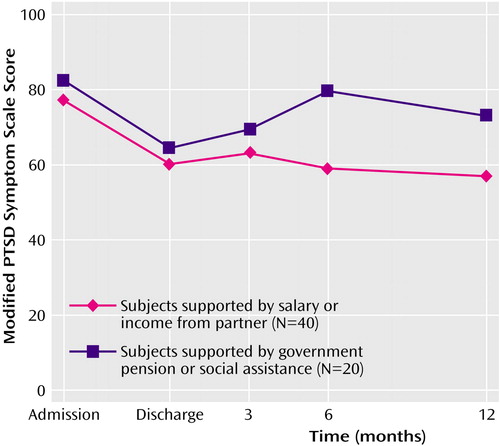
Figure 3. PTSD Symptom Level Over Time Among Adults Abused as Children Who Completed a 6-Week Inpatient Program for Traumatic Stress Recovery, by Source of Income
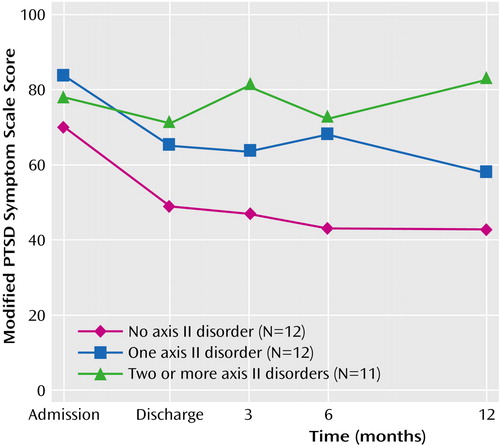
Figure 4. PTSD Symptom Level Over Time Among Adults Abused as Children Who Completed a 6-Week Inpatient Program for Traumatic Stress Recovery, by Axis II Comorbidity
1. Courtois CA, Bloom SL: Inpatient treatment, in Effective Treatments for PTSD: Practice Guidelines From the International Society for Traumatic Stress Studies. Edited by Foa EB, Keane TM, Friedman MJ. New York, Guilford, 2000, pp 199–223Google Scholar
2. Johnson DR, Rosenheck R, Fontana A, Lubin H, Charney D, Southwick S: Outcome of intensive inpatient treatment for combat-related posttraumatic stress disorder. Am J Psychiatry 1996; 153:771–777Link, Google Scholar
3. Johnson DR, Lubin H: Treatment preferences of Vietnam veterans with posttraumatic stress disorder. J Trauma Stress 1997; 10:391–405Medline, Google Scholar
4. Shalev AY: Discussion: treatment of prolonged posttraumatic stress disorder-learning from experience. J Trauma Stress 1997; 10:415–423Medline, Google Scholar
5. Allen JG, Coyne L, Console DA: Course of illness following specialized inpatient treatment for women with trauma-related psychopathology. Bull Menninger Clin 2000; 64:235–256Medline, Google Scholar
6. Ellason JW, Ross CA: Two-year follow-up of inpatients with dissociative identity disorder. Am J Psychiatry 1997; 154:832–839Link, Google Scholar
7. Wright DC, Woo WL, Muller RT, Fernandes CB, Kraftcheck ER: An investigation of trauma-centered inpatient treatment for adult survivors of abuse. Child Abuse Negl 2003; 27:393–406Crossref, Medline, Google Scholar
8. Bloom SL: The sanctuary model: developing generic inpatient programs for the treatment of psychological trauma, in Handbook of Posttraumatic Therapy: A Practical Guide to Intervention, Treatment, and Research. Edited by Williams MB, Sommer JF Jr. New York, Greenwood Publishing, 1994, pp 474–491Google Scholar
9. Herman J: Trauma and Recovery. New York, Basic Books, 1992Google Scholar
10. Wright DC, Woo WL: Treating post-traumatic stress disorder in a therapeutic community: the experience of a Canadian psychiatric hospital. Therapeutic Communities 2000; 21:105–118Google Scholar
11. Falsetti SA: A review of the Modified PTSD Symptom Scale, in Proceedings of the 13th annual meeting of the International Society of Traumatic Stress Studies. Northbrook, Ill, ISTSS, 1997Google Scholar
12. Palmer SE, Brown RA, Rae-Grant NI, Loughlin MJ: Survivors of childhood abuse: their reported experiences with professional help. Soc Work 2001; 46:136–145Crossref, Medline, Google Scholar
13. Resnick HS, Best CL, Kilpatrick DG, Freedy JR, Falsetti SA: Trauma Assessment for Adults—Self-Report. Charleston, Medical University of South Carolina, National Crime Victims Research and Treatment Center, 1993Google Scholar
14. Derogatis LR: SCL-90-R: Administration, Scoring, and Procedures Manual, II. Towson, Md, Clinical Psychometric Research, 1992Google Scholar
15. Falsetti SA, Resnick HS, Resick PA, Kilpatrick DG: The Modified PTSD Symptom Scale: a brief self-report measure of posttraumatic stress disorder. Behavior Therapist 1993; 16:161–162Google Scholar
16. Pearlman LA: The Traumatic Stress Institute Belief Scale—Revision L, in Measurement of Stress, Trauma, and Adaptation. Edited by Stamm BH. Lutherville, Md, Sidran, 1996, pp 415–417Google Scholar
17. First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin L: Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II): User’s Guide. Washington, DC, American Psychiatric Press, 1997Google Scholar
18. Jacobson NS, Truax P: Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol 1991; 59:12–19Crossref, Medline, Google Scholar
19. Palmer S, Stalker C, Gadbois S, Harper K: What works for survivors of childhood abuse: learning from participants in an inpatient treatment program. Am J Orthopsychiatry 2004; 74:112–121Crossref, Medline, Google Scholar
20. Hammarberg M, Silver SM: Outcome of treatment for post-traumatic stress disorder in a primary care unit serving Vietnam veterans. J Trauma Stress 1994; 7:195–216Crossref, Medline, Google Scholar
21. Ford JD, Fisher P, Larson L: Object relations as a predictor of treatment outcome with chronic posttraumatic stress disorder. J Consult Clin Psychol 1997; 65:547–559Crossref, Medline, Google Scholar
22. Stein MB, Hanna C, Koverola C, Torchia M, McClarty B: Structural brain changes in PTSD: does trauma alter neuroanatomy? Ann NY Acad Sci 1997; 821:76–82Crossref, Medline, Google Scholar
23. Fontana A, Rosenheck R: Effectiveness and cost of the inpatient treatment of posttraumatic stress disorder: comparison of three models of treatment. Am J Psychiatry 1997; 154:758–765Link, Google Scholar



