The Role of Peritraumatic Dissociation and Gender in the Association Between Trauma and Mental Health in a Palestinian Community Sample
Abstract
OBJECTIVE: This research focused on gender-specific trauma exposure and mental health symptoms among Palestinians living in conditions of military violence. It also examined the gender-specific role of peritraumatic dissociation in moderating the association between lifetime trauma and mental health. METHOD: A random sample of 311 Palestinian women and 274 men ages 16–60 years from the Gaza Strip participated. The subjects were asked about lifetime trauma and peritraumatic dissociation during their most severe traumatic experience. Mental health was indicated by total scores and diagnostic variables of posttraumatic stress disorder (PTSD), anxiety, mood (depression), and somatization disorders. Symptoms of hostility were assessed as a total score. RESULTS: The women reported a lower level of lifetime trauma than the men, but exposure to trauma was associated with PTSD among both genders. Exposure to lifetime trauma was further associated with anxiety, mood, and somatoform disorders only among women but not among men. No gender differences were found in the level of peritraumatic dissociation. Analyses on moderating effects showed that peritraumatic dissociation made both men and women more vulnerable to symptoms of hostility and men to depressive symptoms when they were exposed to lifetime trauma. CONCLUSIONS: The results are consistent with previous studies in more peaceful conditions: men experience more traumatic events, whereas exposure is associated with more severe psychiatric disorders among women. Peritraumatic dissociation as an acute response to trauma constituted a risk for mental health symptoms in both genders.
The Middle East is the scene of persistent military violence, human rights abuses, and subsequent family tragedies. However, few local epidemiological data are available on the prevalence of traumatic events, mental health symptoms, and acute responses to trauma. This study focuses on gender-specific trauma exposure, mental health, and peritraumatic dissociation among Palestinians living in the Gaza Strip.
Studies of the general population in North America show that both genders are exposed to multiple traumas but of a different nature: men to direct threats and military and civilian violence and women to indirect, sexual, and domestic violence (1–4). Although women are exposed to less severe direct trauma, they show more posttraumatic stress disorder (PTSD) than men do (5–7). For instance, a prospective study of 2,181 participants in the Detroit metropolitan area showed that among 18–45-year-olds, the prevalence of DSM-IV PTSD was 13% among the women and 6.2% among the men (1). Women also suffer more often from chronic PTSD (8). Results on gender differences are not, however, unanimous. Some studies have shown higher PTSD rates among men than women, especially in veteran samples (9, 10). Kulka et al. (9) found a PTSD prevalence of 15% among male and 8.5% among female American Vietnam veterans. The result can be explained by direct exposure to combat experiences, which made men more vulnerable. Also, only few gender differences have been found in the context of natural disasters (11, 12). Gender differences in PTSD may thus be trauma specific, and unique social and biological underlying mechanisms may explain their variation. This study focuses on one potential explanation for the greater female susceptibility to trauma-related symptoms in a community setting: peritraumatic dissociation.
The way people respond during acute exposure to trauma is crucial in explaining whether they recover or develop mental health symptoms. It is generally agreed that showing dissociation, i.e., losing sense of time, behaving mechanically (“like a machine”), or feeling like a bystander watching events occur is a risk for PTSD. Shalev and his team (13–15) in their prospective studies confirmed that peritraumatic dissociation predicts PTSD among accident victims. Positive associations between peritraumatic dissociation and PTSD have also been found in retrospective study settings among war veterans (16–19), disaster and accident survivors (20–22), and emergency workers (23).
It is not yet fully understood why dissociation constitutes a risk for posttraumatic symptoms and what function it serves. One may suggest that, analogously with abnormal startle responses (24–26), dissociative states may serve a survival purpose at some level. Peritraumatic dissociation can be beneficial in the short run because it enables victims to dissociate themselves from overwhelming feelings of fear, horror, and revulsion (27). On the other hand, peritraumatic dissociation may prolong physiological and neurobiological stress reactions and subsequently sensitize victims and increase susceptibility to disorders. However, there is no systematic research available on the risk versus protective functions of peritraumatic dissociation. Only one study could be found suggesting that peritraumatic dissociation may moderate the negative mental health consequences of military combat (28).
Research shows no gender differences in the level of peritraumatic dissociation during traumatic events (17, 19, 23). However, no research is available on the gender-specific mental health role of peritraumatic dissociation. Women and men show unique ways of responding to danger and expressing distress (29), and therefore, we may expect gender differences in peritraumatic dissociation moderating the association between trauma exposure and mental health symptoms.
In this article, we study exposure to trauma, mental health symptoms, and the moderating role of peritraumatic dissociation in a Palestinian community sample. We formulated three gender-specific hypotheses: first, that men report higher frequencies of traumatic events in conditions of military violence; second, that we expect higher levels of psychiatric disorders among traumatized women than among traumatized men; and third, that we expect equal levels of peritraumatic dissociation between both genders. Furthermore, we explored whether peritraumatic dissociation moderates the impact of traumatic events on posttraumatic, depressive, somatic, and hostility symptoms in the same ways in men and women. The moderating effect of peritraumatic dissociation may either protect mental health from the negative impact of trauma or make people more vulnerable to mental health problems.
Method
Sampling and Procedure
The sample consisted of 585 subjects. The mean age was 31.6 years (SD=11.6), and the age ranged between 16 and 60 years. Fifty-three percent of the respondents (N=311) were female, and 47% of them (N=274) were male. A multistage sampling procedure, combining both nonprobability (selecting representative communities) and probability (selecting random households within the selected community), was used. This ensured a representative sample of the heterogeneous population in Gaza. The cities, refugee camps, and resettled areas were randomly chosen. Out of eight refugee camps, three were randomly selected. All three cities were selected. Of the five resettlement areas, two were selected that had heterogeneous populations.
The neighborhoods in each selected area were randomly assigned. The interviewers used random-direction number lists to choose the direction of the movement, starting from mosques and crossroads. Another random-number list was used to select the third house in that direction. The mosques were chosen because they are the most common and obvious landmarks and are equally distributed all over the populated areas. When there was more than one mosque in a neighborhood, they were all taken as starting points, and the number of subjects to be interviewed was divided among them.
The participants were interviewed in their homes by trained interviewers. The interviewers (N=8) used another random-number list to select one subject from the household who fulfilled the sample criteria. One member from each household who fulfilled the age criterion (16–60 years) was interviewed. The criterion for exclusion was severe cognitive impairment or severe psychosis. Verbal consent was obtained because the suspicion caused by the harsh sociopolitical situation in Gaza made signed consent almost impossible. For the same reason, the participants responded anonymously. If the subject was not available at the time of the first visit, a message was left, and two more contact attempts were made. Dropouts were 15 people (2.5%) from the original sample (N=600); five declined to participate, and 10 could not be interviewed because of illness or absence. All of these were young men. The data were collected in July to October 1997.
Measures
Traumatic events were evaluated by an adapted version of the Life Events and Social History Questionnaire (30). The 13-item version consists, first, of family-related traumatic events, such as death or separation in the family, youth domestic events, and general life events, and second, of traumatic events that people typically face in military and political conflicts (e.g., witnessing killing and being the target of injury, shelling, and imprisonment). The participants were asked whether they had been exposed to each event (0=no, 1=yes) either in childhood (<12 years) or later in adulthood (>12 years). The total score of lifetime trauma ranged between 0 and 26 and had an average of 2.79 (SD=3.49). A dichotomous score was also constructed by giving the value 0 to those with no traumatic experiences (N=213) and 1 to those with one or more traumatic experiences (N=372).
Peritraumatic dissociation was assessed with the revised Peritraumatic Dissociative Experiences Questionnaire (31). This is an eight-item questionnaire for assessing retrospective reports of depersonalization, derealization, out-of-body experiences, and altered time perception during a traumatic event. Two items stressed in the literature (32) were added: 1) difficulty in making sense of what was happening and 2) feeling disoriented. The participants were asked to remember the worst, most distressing traumatic event and then to report whether they had (rating=1) or had not (rating=0) experienced described dissociations during that event. Internal consistency has been found to be good among Vietnam veterans (17). Cronbach’s alpha in this sample was 0.94. We used the method described by Tichenor et al. (19) to calculate the total score for peritraumatic dissociation.
PTSD was evaluated in relation to experienced adverse events from the aforementioned life events interview. The PTSD section of the World Health Organization Composite International Diagnostic Interview 2.1 (33) was used to assess lifetime PTSD according to DSM-IV criteria. Although the Composite International Diagnostic Interview/DSM-IV PTSD diagnosis has not been validated in a general population sample, good agreement between the Composite International Diagnostic Interview and independent clinical reinterviews has been found (34). Other Composite International Diagnostic Interview sections were used to assess mood disorder, somatoform disorder, and (“other”) anxiety disorder. In our analyses, mood disorder covers DSM-IV dysthymia and major depressive disorder. Somatoform disorder contains DSM-IV somatization disorder, conversion disorder, hypochondriasis, and pain disorder. (“Other”) anxiety disorder encompasses DSM-IV panic disorder with or without agoraphobia, agoraphobia without history of panic disorder, social phobia, and specific phobia. We used two measures for the disorders: a total score that refers to the number of symptoms of the disorder and a variable that refers to the presence of the DSM-IV lifetime diagnosis of the disorder. A score for symptoms of hostility was derived from the Revised SCL-90-R Symptoms Checklist (35).
Instruments were translated focusing on content, criterion, technical, conceptual, and semantic equivalence. The process of translation and adaptation involved 1) examination of the instruments by bilingual experts (Arabic and Dutch), 2) translation into Arabic, 3) literal back-translation by different translators, 4) examination of the back-translation by monolingual experts, 5) back-translation of all items changed by the monolingual experts, 6) examination of the back-translation by a bilingual group informed by the discussion of the monolingual experts, and 7) pilot testing (36).
Statistical Analysis
We used chi-square analysis and Student’s t test to examine univariate differences in psychiatric disorders and sociodemographic variables between the men and women and chi-square analysis to test the hypothesis on gendered associations between trauma and psychiatric disorders. We report two-tailed test values, and we present Yates-corrected chi-square values for all two-by-two tables. Values for Student’s t tests are reported according to the results of testing the equality of variance assumption.
We assessed the following possible factors associated with different indicators of psychiatric disorders: lifetime traumatic events, peritraumatic dissociation, refugee status, family history of mental illness, and age. Main effects of factors on indicators of psychiatric disorders and moderator effects were identified by the following steps in hierarchical multiple regression analyses. First, we created the interaction term of the factors for lifetime traumatic events and peritraumatic dissociation. Next, we used hierarchical multiple regression analyses to estimate, as the first and second steps, the main effects of the lifetime traumatic events and peritraumatic dissociation on mental health symptoms. In the third step, we estimated the effect of the interaction term. A moderator effect was found when the estimate of the interaction term was significant (37, 38). In the fourth step, we estimated the main effects of the other factors on mental health symptoms. For all analyses, we centered the data to prevent possible multicollinearity between the factors. Standardized variables (z scores) and interaction terms (computed from the z scores of the factors) were entered in the regression analyses.
Results
Demographic Factors
The women and men did not differ in age, marital status, number of children, refugee status, place of residency, and family history of mental illness (all comparisons between women and men on these variables had p>0.05). The men estimated their socioeconomic status to be better than that of the women (χ2=83.89, df=1, p<0.0001). Almost two-thirds (62%) of the men and 24% of the women reported their socioeconomic status to be above average, whereas 37% of the men and 74% of the women reported average socioeconomic status. The number of participants estimating their socioeconomic status as below average was small (1.5% of the men and 2% of the women). More women (8%) had not attended school than men (3%) (χ2=9.87, df=1, p<0.002). However, gender did not affect literacy (90% of the total sample was literate).
Gender, Trauma, and Mental Health
The results show that the lifetime prevalence of traumatic events was higher among the men (mean=4.68, SD=3.92) than the women (mean=1.13, SD=1.85) (t=13.70, df=378.79, p<0.0001; no equal variances were assumed). Eighty-six percent of the men (N=235) and 44% (N=137) of the women had experienced at least one traumatic event during their lifetimes (χ2=29.72, df=1, p<0.0001).
Figure 1 presents the results of gender-specific associations between exposure to lifetime trauma and mental health. They substantiate the hypothesis that when traumatized, women show higher levels of psychiatric distress than men, except for PTSD. Exposure to lifetime trauma was associated with anxiety disorder among women (χ2=9.85, df=1, p<0.002) but not among men (χ2=1.24, df=1, n.s.) and with mood disorder among women (χ2=8.68, df=1, p<0.003) but not among men (χ2=0.66, df=1, n.s.). The significant association was found between trauma and somatoform disorder among the women (χ2=9.65, df=1, p<0.002) but not among men (χ2=0.13, df=1, n.s.).
The association between lifetime trauma and PTSD did not differ between genders. Thirty percent of the women and 25% of the men who had experienced lifetime trauma had also been diagnosed with PTSD (χ2=1.62, df=1, n.s.). This indicates that although the men generally had a higher level of PTSD (24%) than the women (16%), the gender differences diminished when exposure to lifetime trauma was taken into account.
The Moderating Role of Peritraumatic Dissociation
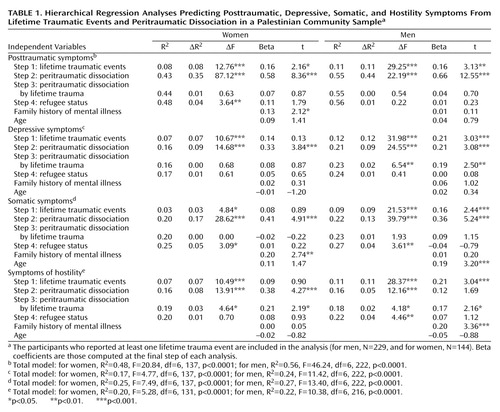
We found no difference between women (mean 2.94, SD=1.21) and men (mean 2.73, SD=1.25) in the total score for peritraumatic dissociation (t=–1.57, df=583, n.s.). Table 1 shows the hierarchical multiple regression analyses, main and interaction effects of lifetime trauma and peritraumatic dissociation and demographic variables on mental health symptoms among women and men. The results revealed significant trauma-by-dissociation interaction effects (step 3) on depressive symptoms among men and on hostility symptoms among both genders. The positive moderating effects indicate that trauma was relatively less associated with these symptoms if the persons reported low levels of peritraumatic dissociation during the most severe trauma.
The hierarchical multiple regression analyses accounted for 48% of the variance in the women’s and 56% in the men’s posttraumatic symptoms. Peritraumatic dissociation did not have any moderating (either protective or risk) effect on posttraumatic symptoms, as the absence of significant interaction effects indicates. In both genders, lifetime trauma and peritraumatic dissociation were associated with high levels of posttraumatic symptoms (main effects). Among the women, having a history of mental illness in the family was further associated with posttraumatic symptoms.
The hierarchical multiple regression analyses accounted for 17% of the variance in the women’s and 24% in the men’s depressive symptoms. The models for depressive symptoms differed among the men and the women. Among women, only peritraumatic dissociation accounted for depressive symptoms: high dissociation was associated with a high level of depressive symptoms. Among men, there were significant main and interaction effects of both lifetime trauma and peritraumatic dissociation. These results indicated that exposure to lifetime trauma was relatively more associated with depressive symptoms, especially if the men had shown peritraumatic dissociation.
The hierarchical multiple regression analyses accounted for 25% of the variance of the women’s and 27% of the variance of the men’s somatic symptoms. Peritraumatic dissociation did not have any moderating (risk or protective) effect on somatic symptoms, as the absence of interaction effects indicated. Among the women, those who had shown peritraumatic dissociation and had mental illness in their family reported the highest level of somatic symptoms. Among the men, lifetime trauma, peritraumatic dissociation, and age predicted the level of somatic symptoms, i.e., the older men with high levels of lifetime trauma and peritraumatic dissociation reported the highest level of somatic symptoms.
Finally, the regression models of hostility accounted for 20% of the variance in the women’s and 22% in the men’s hostility symptoms. In both genders, the significant positive lifetime trauma-by-peritraumatic dissociation interaction effects indicated that lifetime trauma was relatively more associated with symptoms of hostility if the participants had shown peritraumatic dissociation. Among the women, peritraumatic dissociation had also a main effect on symptoms of hostility, and among the men, lifetime traumatic events and family mental illness were associated with a high level of hostility symptoms.
Discussion
Contemporary trauma research has focused on the complex moderating factors between exposure and psychopathology. Our study contributes to this by examining gender-specific trauma exposure and mental health consequences and the moderating role of peritraumatic responses in a Palestinian community sample.
Our results confirmed a higher lifetime prevalence of exposure to trauma in men than in women living in conditions of military violence. However, women were more vulnerable than men, as indicated by only women suffering from anxiety, mood, and somatoform disorders when traumatized. No gender differences were found in the association between lifetime trauma and PTSD diagnosis. Thus, our results show more similarities than differences between the conflict-ridden Middle East and more peaceful societies regarding the gender-specificity of exposure to trauma and female vulnerability to psychiatric disorders.
As hypothesized, we found no gender differences in peritraumatic dissociation during the most severe trauma. Peritraumatic dissociation was positively associated with posttraumatic symptoms, which concurs with earlier research (15, 19, 20). We additionally showed that peritraumatic dissociation was also associated with depressive and somatic symptoms among both men and women and with symptoms of hostility among women. Shalev and Yehuda (28) reminded us that PTSD is no longer considered a unique consequence of trauma. Research confirms that depression and somatic disorders are common among female rape (39) and male torture (40) victims. Likewise, we suggest that PTSD may not be the unique consequence of peritraumatic dissociation, and future studies should conceptualize a wide range of peritrauma-related symptoms.
We examined whether peritraumatic dissociation functions as a moderating factor (risk or protective) among trauma victims. The results revealed only a negative function of peritraumatic dissociation among both men and women. Lifetime trauma was associated with a relatively higher level of hostility if persons reported a high level of peritraumatic dissociation during the most severe trauma. The findings do not explain the greater female vulnerability to trauma-related symptoms because peritraumatic dissociation amplified the negative effect of trauma exposure in both genders. In fact, dissociation made men even more vulnerable because they also showed relatively more depressive symptoms when exposed to a high level of lifetime trauma.
Middle Eastern culture and politics constitute a special context for female and male vulnerability. Male heroism and sacrifice were highly appreciated during the Palestinian Intifada, as in any struggle for independence (41). This may explain that the peritraumatic dissociation formed a risk for depressive symptoms among traumatized men. Dissociative responses apparently connoted loss of control, shame, weakness, and subsequent low self-esteem, all promoting depressiveness. Women’s dissociative and uncontrollable responses in a trauma scene are more easily accepted, especially in a culture that encourages strong and visual female emotional expression, for example, at funerals and other good-byes. The gender-specific roles of peritraumatic symptoms compel us to consider the symbolic, cultural, and social meanings of trauma and the ideological norms shaping people’s responses (29, 41).
We applied a geographical random-sampling method, which is not without problems. The sample excluded individuals who were residing in institutions such as hospitals and prisons. The population density in Gaza is one of the highest in the world, and the population is evenly distributed in refugee camps and towns but not in resettled areas (42). The choice of the mosque as a locator point for sample collecting was based on the consideration that neither population density nor social status differs according to mosque location in Gaza.
There is ample evidence that trauma victims tend to distort, narrow, and repress their memories of painful and often shameful scenes (26). Subsequently, our research deserves criticism for using single-source information and relying on retrospective reporting. The research setting could be strengthened by applying observation methods for peritraumatic dissociation during traumatic events and archiving material regarding exposure to lifetime trauma.
 |
Received May 2, 2001; revisions received Sept. 26, 2002, June 20, 2003, and Jan. 12, 2004; accepted May 10, 2004. From the Department of Psychology, University of Tampere, and the Department of Psychology, University of Helsinki, Helsinki, Finland; the Gaza Community Mental Health Programme, Gaza, Palestine (via Israel); and the Transcultural Psychosocial Organization, Vrije Universiteit, Amsterdam, the Netherlands. Address correspondence and reprint requests to Dr. Punamäki, Department of Psychology, 33014 University of Tampere, Tampere, Finland; [email protected] (e-mail).
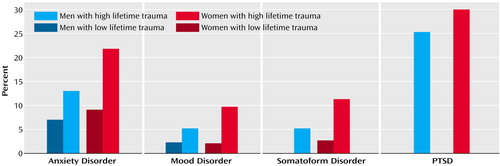
Figure 1. Interaction Effects of Trauma and Gender on Anxiety, Mood, Somatoform Disorder, and Posttraumatic Stress Disorder (PTSD) in a Palestinian Community Sample
1. Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P: Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry 1998; 55:626–632Crossref, Medline, Google Scholar
2. Norris FH: Epidemiology of trauma: frequency and impact of different potentially traumatic events on different demographic groups. J Consult Clin Psychol 1992; 60:409–418Crossref, Medline, Google Scholar
3. Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL: Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J Consult Clin Psychol 1993; 61:984–991Crossref, Medline, Google Scholar
4. Stein MB, Walker JR, Hazen AL, Forde DR: Full and partial posttraumatic stress disorder: findings from a community survey. Am J Psychiatry 1997; 154:1114–1119Link, Google Scholar
5. Breslau N, Davis GC, Andreski P, Peterson EL, Schultz LR: Sex differences in posttraumatic stress disorder. Arch Gen Psychiatry 1997; 54:1044–1048Crossref, Medline, Google Scholar
6. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB: Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995; 52:1048–1060Crossref, Medline, Google Scholar
7. Stein MB, Walker JR, Forde DR: Gender differences in susceptibility to posttraumatic stress disorder. Behav Res Ther 2000; 38:619–628Crossref, Medline, Google Scholar
8. Breslau N, Davis GC: Posttraumatic stress disorder: the stressor criterion. J Nerv Ment Dis 1987; 175:255–264Crossref, Medline, Google Scholar
9. Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS: Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. New York, Brunner/Mazel, 1990Google Scholar
10. Willer JK, Grossman LS: Mental health care needs of female veterans. Psychiatr Serv 1995; 46:938–940Link, Google Scholar
11. Kaniasty K, Norris FH: A test of the social support deterioration model in the context of natural disaster. J Pers Soc Psychol 1993; 64:395–408Crossref, Medline, Google Scholar
12. Norris FH, Kaniasty K: Received and perceived social support in times of stress: a test of the social support deterioration deterrence model. J Pers Soc Psychol 1996; 71:498–511Crossref, Medline, Google Scholar
13. Freedman SA, Brandes D, Peri T, Shalev AY: Predictors of chronic post-traumatic stress disorder: a prospective study. Br J Psychiatry 1999; 174:353–359Crossref, Medline, Google Scholar
14. Shalev AY, Freedman S, Peri T, Brandes D, Sahar T: Predicting PTSD in trauma survivors: prospective evaluation of self-report and clinician-administered instruments. Br J Psychiatry 1997; 170:558–564Crossref, Medline, Google Scholar
15. Shalev AY, Freedman S, Peri T, Brandes D, Sahar T, Orr SP, Pitman RK: Prospective study of posttraumatic stress disorder and depression following trauma. Am J Psychiatry 1998; 155:630–637Link, Google Scholar
16. Bremner JD, Southwick SM, Johnson DR, Yehuda R, Charney DS: Childhood physical abuse and combat-related posttraumatic stress disorder in Vietnam veterans. Am J Psychiatry 1993; 150:235–239Link, Google Scholar
17. Marmar CR, Weiss DS, Schlenger WE, Fairbank JA, Jordan BK, Kulka RA, Hough RL: Peritraumatic dissociation and posttraumatic stress in male Vietnam theater veterans. Am J Psychiatry 1994; 151:902–907Link, Google Scholar
18. O’Toole BI, Marshall RP, Schureck RJ, Dobson M: Combat, dissociation, and posttraumatic stress disorder in Australian Vietnam veterans. J Trauma Stress 1999; 12:625–640Crossref, Medline, Google Scholar
19. Tichenor V, Marmar CR, Weiss DS, Metzler TJ, Ronfeldt HM: The relationship of peritraumatic dissociation and posttraumatic stress: findings in female Vietnam theater veterans. J Consult Clin Psychol 1996; 64:1054–1059Crossref, Medline, Google Scholar
20. Koopman C, Classen C, Spiegel D: Predictors of posttraumatic stress symptoms among survivors of the Oakland/Berkeley, Calif, firestorm. Am J Psychiatry 1994; 151:888–894Link, Google Scholar
21. Holen A: The North Sea oil rig disaster, in International Handbook of Traumatic Stress Syndromes. Edited by Wilson JP, Raphael B. New York, Plenum, 1993, pp 471–478Google Scholar
22. Ursano RJ, Fullerton CS, Epstein RS, Crowley B, Vance K, Kao T-C, Baum A: Peritraumatic dissociation and posttraumatic stress disorder following motor vehicle accidents. Am J Psychiatry 1999; 156:1808–1810Abstract, Google Scholar
23. Weiss DS, Marmar CR, Metzler TJ, Ronfeldt HM: Predicting symptomatic distress in emergency services personnel. J Consult Clin Psychol 1995; 63:361–368Crossref, Medline, Google Scholar
24. Griffin MG, Resick PA, Mechanic MB: Objective assessment of peritraumatic dissociation: psychophysiological indicators. Am J Psychiatry 1997; 154:1081–1088Link, Google Scholar
25. Shalev AY, Peri T, Brandes D, Freedman S, Orr SP, Pitman RK: Auditory startle response in trauma survivors with posttraumatic stress disorder: a prospective study. Am J Psychiatry 2000; 157:255–261Link, Google Scholar
26. van der Kolk BA, Burbridge JA, Suzuki J: The psychobiology of traumatic memory: clinical implications of neuroimaging studies. Ann NY Acad Sci 1997; 821:99–113Crossref, Medline, Google Scholar
27. Horowitz MJ: Introduction, in Essential Papers on Posttraumatic Stress Disorder. Edited by Horowitz MJ. New York, New York University Press, 1999, pp 1–17Google Scholar
28. Shalev AY, Yehuda R: Longitudinal development of traumatic stress disorders, in Psychological Trauma. Edited by Yehuda R. Washington, DC, American Psychiatric Press, 1998, pp 31–66Google Scholar
29. Taylor SE, Klein LC, Lewis BP, Gruenewald TL, Gurung RA, Updegraff JA: Biobehavioral responses to stress in females: tend-and-befriend, not fight-or-flight. Psychol Rev 2000; 107:411–429Crossref, Medline, Google Scholar
30. Mollica RF, Caspi-Yavin Y, Bollini P, Truong T, Tor S, Lavelle J: The Harvard Trauma Questionnaire: validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. J Nerv Ment Dis 1992; 180:111–116Crossref, Medline, Google Scholar
31. Marmar CR, Weiss DS, Metzler TJ, Delucchi K: Characteristics of emergency services personnel related to peritraumatic dissociation during critical incidence exposure. Am J Psychiatry 1996; 153(July Festschrift suppl):94–102Google Scholar
32. Breslau N: Epidemiology of trauma and posttraumatic stress disorder, in Psychological Trauma. Edited by Yehuda R. Washington, DC, American Psychiatric Press, 1998, pp 1–29Google Scholar
33. World Health Organization: Composite International Diagnostic Interview (CIDI), version 2.1. Geneva, WHO, 1997Google Scholar
34. Peters L, Andrews G, Cottler LB, Chatterji S, Janca A, Smeets R: The Composite International Diagnostic Interview post-traumatic stress disorder module: preliminary data. Int J Methods Psychiatr Res 1996; 6:167–174Crossref, Google Scholar
35. Derogatis LR, Cleary PA: Confirmation of the dimensional structure of the SCL-90: a study in construct validation. J Clin Psychol 1977; 33:981–989Crossref, Google Scholar
36. Flaherty JA, Gaviria FM, Pathak D, Mitchell T, Wintrob R, Richman JA, Birz S: Developing instruments for cross-cultural psychiatric research. J Nerv Ment Dis 1988; 176:257–263Medline, Google Scholar
37. Holmbeck GN: Toward terminological, conceptual, and statistical clarity in the study of mediators and moderators: examples from the child-clinical and pediatric psychology literatures. J Consult Clin Psychol 1997; 65:599–610Crossref, Medline, Google Scholar
38. Aiken LS, West SG: Multiple Regression: Testing and Interpreting Interactions. Newbury Park, Calif, Sage Publications, 1991Google Scholar
39. Girelli SA, Resick PA, Marhoefer-Dvorak S, Hutter CK: Subjective distress and violence during rape: their effects on long-term fear. Violence Vict 1986; 1:35–46Crossref, Medline, Google Scholar
40. Allodi F: Physical and psychiatric effects of torture: Canadian study, in The Breaking of Bodies and Minds: Torture, Psychiatric Abuse, and the Health Professions. Edited by Stover E, Nightingale EO. New York, WH Freeman, 1985, pp 66–78Google Scholar
41. King LA, King DW, Fairbank JA, Keane TM, Adams GA: Resilience-recovery factors in post-traumatic stress disorder among female and male Vietnam veterans: hardiness, postwar social support, and additional stressful life events. J Pers Soc Psychol 1998; 74:420–434Crossref, Medline, Google Scholar
42. Benvenisti M, Khayat S: The West Bank and Gaza Atlas. Jerusalem, Jerusalem Post, 1988Google Scholar



