Placebo-Controlled Study of Pimozide Augmentation of Fluoxetine in Body Dysmorphic Disorder
Abstract
OBJECTIVE: Although body dysmorphic disorder often responds to serotonin reuptake inhibitors (SRIs), most patients do not respond or respond only partially. However, placebo-controlled studies of augmentation of SRIs have not been done. Furthermore, although 40%–50% of patients are delusional, studies of antipsychotic medications have not been done. METHOD: Twenty-eight patients with body dysmorphic disorder or its delusional variant participated in an 8-week, placebo-controlled, double-blind, parallel-group study of pimozide augmentation of fluoxetine. RESULTS: Pimozide was not more effective than placebo: two (18.2%) of 11 subjects responded to pimozide and three (17.6%) of 17 subjects responded to placebo. There was no significant effect of baseline delusionality on endpoint severity of body dysmorphic disorder. Delusionality did not decrease significantly more with pimozide than placebo. CONCLUSIONS: Pimozide augmentation of fluoxetine treatment for body dysmorphic disorder was not more effective than placebo, even in more delusional patients. Further studies of augmentation for SRIs are needed.
Body dysmorphic disorder is distressing, impairing, and relatively common (1, 2). Many patients require hospitalization, become housebound, or attempt suicide (1, 2). Although serotonin-reuptake inhibitors (SRIs) are often efficacious (2–4), most patients do not respond or respond only partially. However, no placebo-controlled studies of augmentation of SRIs for the treatment of body dysmorphic disorder have been done. Furthermore, although 40%–50% of patients are delusional (1, 2), thereby qualifying for a diagnosis of delusional disorder in addition to body dysmorphic disorder, no studies of antipsychotic medications have been done for these patients.
Pimozide was selected as an SRI augmentor because antipsychotics have been widely recommended and used for body dysmorphic disorder (5, 6), despite a lack of research examining their efficacy. Pimozide has been proposed to be uniquely effective for disorders characterized by somatic delusions (monosymptomatic hypochondriacal psychoses), including body dysmorphic disorder (5, 6). Also, pimozide effectively augments SRIs in obsessive-compulsive disorder (OCD) (7), which has similarities to body dysmorphic disorder.
Method
Twenty-eight patients were included in the study. These subjects had received fluoxetine for ≥12 weeks, reaching 80 mg/day if tolerated (mean=62.5 mg/day, SD=20.1). Nineteen of these patients received fluoxetine in a separate placebo-controlled study (4); 16 did not respond to fluoxetine, and the three responders still had severe enough body dysmorphic disorder to participate in this pimozide study. Nine of the patients received the fluoxetine in my practice. An additional 16 patients in the separate placebo-controlled fluoxetine study (13 nonresponders and three responders), plus two nonresponders from my clinical practice, did not enter the pimozide study for different reasons (e.g., lack of interest).
The 28 patients were randomly assigned to 8 weeks of double-blind pimozide (N=11) or placebo (N=17) augmentation while remaining on a fixed fluoxetine dose. Pimozide and placebo were furnished in identical-appearing tablets (2 mg for pimozide). Subjects were started on 1 mg/day, with an attempt made to raise the dose to 2 mg/day after 1 week and then by 2 mg per week to a maximum of 10 mg/day if tolerated. After a complete description of the study, written informed consent was obtained from all participants.
Inclusion/exclusion criteria were standard for efficacy studies (e.g., reference 4). Following fluoxetine treatment, subjects had a body dysmorphic disorder score of ≥20 on the Yale-Brown Obsessive Compulsive Scale Modified for Body Dysmorphic Disorder (8) with fair, poor, or absent insight and were at least moderately ill according to the Clinical Global Impression (CGI) scale. Subjects took no other psychotropics. They could not begin psychotherapy during the study or have begun it within the past 4 months. The Yale-Brown Obsessive Compulsive Scale Modified for Body Dysmorphic Disorder score was the primary outcome measure; a decrease in score of ≥30% determined treatment response (8). The Brown Assessment of Beliefs Scale (9) assessed delusionality of appearance beliefs and categorized subjects at baseline as delusional (N=12) or nondelusional (N=16) according to an empirically derived cutoff point. Other measures were the CGI, Hamilton Rating Scale for Depression, Brief Psychiatric Rating Scale, and Structured Clinical Interview for DSM-III-R.
Excluding the augmented fluoxetine trial, 18 (64.3%) of the 28 subjects had previously received a total of 58 psychotropic medications. Fifteen subjects received a total of 26 SRIs, and three received a neuroleptic (one trial each). Only two SRI trials improved body dysmorphic disorder, but only five trials were considered minimally adequate for body dysmorphic disorder (2), one of which led to improvement. Three non-SRI medications (a non-SRI tricyclic, lithium, and a neuroleptic) improved body dysmorphic disorder.
Analyses were based on the intent-to-treat study group and used analysis of covariance (ANCOVA) with baseline measures as the covariate. The effect size (d) was based on ANCOVA. Continuous variables were analyzed with independent-sample t tests, and dichotomous variables were analyzed with chi-square test and Fisher’s exact test. All tests were two-tailed; the alpha level was 0.05.
Results
Baseline age, gender, and body dysmorphic disorder severity did not significantly differ between groups, although the pimozide group were younger at the onset of body dysmorphic disorder (mean=13.7 years, SD=3.1, versus mean=20.4, SD=8.6) (t=2.5, df=26, p=0.02) and had had body dysmorphic disorder for a longer time (mean=21.2 years, SD=10.8, versus mean=12.4, SD=10.1) (t=–2.1, df=25, p=0.04). Thirteen (76.5%) of the 17 patients given placebo and six (54.5%) of the 11 given pimozide completed the study (eight [72.7%] of the pimozide subjects completed ≥4 weeks). The mean endpoint pimozide dose was 1.7 mg/day (SD=1.0); the equivalent dose in the placebo group was 5.0 mg/day (SD=3.4).
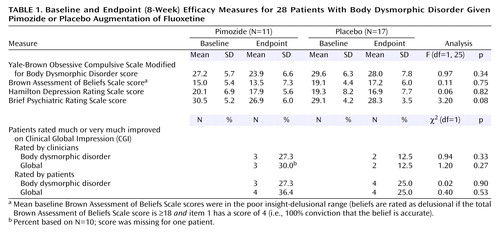
Pimozide was not more efficacious than placebo for body dysmorphic disorder severity or on any other measure (Table 1). Mean scores on the 48-point Yale-Brown Obsessive Compulsive Scale Modified for Body Dysmorphic Disorder decreased only 1.7 points more with pimozide than placebo. The effect size (d) was 0.23. Two (18.2%) of 11 subjects responded to pimozide and three (17.6%) of 17 responded to placebo (χ2=0.001, df=1, p=0.97). There was no significant effect of baseline delusionality on endpoint body dysmorphic disorder severity (F=2.9, df=1, 25, p=0.10). One (8.3%) of the 12 delusional patients responded (this patient responded to placebo), and four (25.0%) of the 16 nondelusional patients responded (two to pimozide and two to placebo). Delusionality did not decrease more with pimozide than placebo (F=0.11, df=1, 25, p=0.75). The only adverse event more frequent with pimozide was difficulty sitting still (54.6% [N=6] versus 0%) (p=0.001, Fisher’s exact test). No serious adverse events occurred.
Discussion
Although pimozide has been proposed to be effective for body dysmorphic disorder (5, 6), it was not more efficacious in augmenting fluoxetine and did not improve delusionality more than placebo. Because power was limited, these results are preliminary. Power to detect a medium effect size (d=0.50) was 25%, and power to detect a large effect size (d=0.80) was 53%. Nonetheless, the pimozide response rate was very low and similar to that of placebo. The mean group difference in improvement score on the Yale-Brown Obsessive Compulsive Scale Modified for Body Dysmorphic Disorder was not clinically meaningful. A sample of more than 600 subjects would be needed to yield a statistically significant result with the effect size obtained.
Studies (1–4) have found similarities between body dysmorphic disorder’s delusional and nondelusional forms, suggesting they may be the same disorder. This study offers some support for this, given the similar pimozide response rate in both groups. It is unclear why pimozide augmentation is efficacious for OCD (7) but not for body dysmorphic disorder in this study, especially because body dysmorphic disorder patients are more delusional (2). Possible explanations include this study’s low power, the fairly modest mean pimozide dose attained (1.7 mg/day versus 6.5 mg/day, SD=5.4, in OCD [7]), and possible treatment refractoriness of the body dysmorphic disorder patients. Furthermore, studies of augmentation of SRIs with pimozide and haloperidol in patients with OCD found higher response rates in those with a tic disorder (100% versus 33%) (10) or a tic disorder or schizotypal personality disorder (88% versus 22%) (7). No body dysmorphic disorder subject had either diagnosis. In addition, body dysmorphic disorder and OCD have other differences and are probably not identical disorders (2). Additional studies of augmentation of SRIs, including studies with atypical antipsychotics, are greatly needed in body dysmorphic disorder, given the paucity of empirically based treatments for this often-disabling disorder.
 |
Presented at the American College of Neuropsychopharmacology Annual Meeting, San Juan, Puerto Rico, December 8–12, 2002. Received April 1, 2003; revisions received Dec. 22, 2003, and April 23, 2004; accepted May 19, 2004. From Brown Medical School and Butler Hospital. Address correspondence and reprint requests to Dr. Phillips, Brown Medical School and Butler Hospital, 345 Blackstone Blvd., Providence, RI 02906; [email protected] (e-mail). Supported in part by the National Alliance for Research on Schizophrenia and Depression. Study medication and matching placebo were supplied by Gate Pharmaceuticals.
1. Phillips KA, McElroy SL, Keck PE Jr, Pope HG Jr, Hudson JI: Body dysmorphic disorder: 30 cases of imagined ugliness. Am J Psychiatry 1993; 150:302–308Link, Google Scholar
2. Phillips KA: Body dysmorphic disorder, in Somatoform and Factitious Disorders. Edited by Phillips KA. Washington, DC, American Psychiatric Press, 2001, pp 67–94Google Scholar
3. Hollander E, Allen A, Kwon J, Aronowitz B, Schmeidler J, Wong C, Simeon D: Clomipramine vs desipramine crossover trial in body dysmorphic disorder: selective efficacy of a serotonin reuptake inhibitor in imagined ugliness. Arch Gen Psychiatry 1999; 56:1033–1039Crossref, Medline, Google Scholar
4. Phillips KA, Albertini RS, Rasmussen SA: A randomized placebo-controlled trial of fluoxetine in body dysmorphic disorder. Arch Gen Psychiatry 2002; 59:381–388Crossref, Medline, Google Scholar
5. Riding J, Munro A: Pimozide in the treatment of monosymptomatic hypochondriacal psychosis. Acta Psychiatr Scand 1975; 52:23–30Crossref, Medline, Google Scholar
6. Munro A, Chmara J: Monosymptomatic hypochondriacal psychosis: a diagnostic checklist based on 50 cases of the disorder. Can J Psychiatry 1982; 27:374–376Crossref, Medline, Google Scholar
7. McDougle CJ, Goodman WK, Price LH, Delgado PL, Krystal JH, Charney DS, Heninger GR: Neuroleptic addition in fluvoxamine-refractory obsessive-compulsive disorder. Am J Psychiatry 1990; 147:652–654Link, Google Scholar
8. Phillips KA, Hollander E, Rasmussen SA, Aronowitz BR, DeCaria C, Goodman WK: A severity rating scale for body dysmorphic disorder: development, reliability, and validity of a modified version of the Yale-Brown Obsessive Compulsive Scale. Psychopharmacol Bull 1997; 33:17–22Medline, Google Scholar
9. Eisen JL, Phillips KA, Baer L, Beer DA, Atala KD, Rasmussen SA: The Brown Assessment of Beliefs Scale: reliability and validity. Am J Psychiatry 1998; 155:102–108Link, Google Scholar
10. McDougle CJ, Goodman WK, Leckman JF, Lee NC, Heninger GR, Price LH: Haloperidol addition in fluvoxamine-refractory obsessive-compulsive disorder. Arch Gen Psychiatry 1994; 51:302–308Crossref, Medline, Google Scholar



