Racial Disparity in the Use of ECT for Affective Disorders
Abstract
OBJECTIVE: Published reports indicate that African Americans are underrepresented among patients treated with ECT. The reason for this disparity in practice has not been determined. This study addressed this question by using existing data on a large series of patients treated with ECT at a single academic medical center. METHOD: The hospital’s administrative databases were used to select Caucasian and African American patients with a diagnosis of major affective disorder treated over the period from November 1993 to March 2002. Independent variables were age, sex, treatment unit, readmission within 30 days, type of insurance, and geographic zone of residence. The dependent variable was likelihood of being treated with ECT, computed for each race group. RESULTS: Caucasians were more likely than African Americans to be treated with ECT (odds ratio=4.71; 95% confidence interval [CI]=3.77–5.90). None of the variables examined provided an explanation for this disparity. When all of the variables were controlled simultaneously, the likelihood of being treated with ECT remained significantly higher for Caucasians than for African Americans (odds ratio=2.48; 95% CI=1.89–3.25). CONCLUSIONS: The racial disparity in the use of ECT cannot be explained on the basis of the variables studied. It is not an artifact of the age of the patient population, nor can it be explained on the basis of insurance coverage, the social class of the patients, or their illnesses’ being more treatment resistant. The authors propose several other hypotheses, including explanations relating to clinical presentation, differential response to other treatments, differences in patients’ willingness to consent, and physicians’ behavior, that could be explored by using other methods.
There has been heightened concern in recent years about the disparities in health care experiences of racial and ethnic minorities in the United States (1, 2). For example, compared with Caucasians, African Americans and members of other minority groups are less likely to have a regular source of health care, more likely to receive poorer- quality hospital care and fewer pediatric prescriptions, and less likely to receive smoking prevention counseling and preventive care (3).
Racial disparities in psychiatric practice—including diagnosis, treatment, and access to services—have also been reported (4). It has been shown repeatedly that, compared with Caucasians, African Americans are more likely to receive a diagnosis of schizophrenia and less likely to receive a diagnosis of an affective disorder (5–8), that African Americans are overrepresented among patients involuntarily admitted to psychiatric hospitals (9), and that, in New York State public hospitals, African Americans are more likely than Caucasians to be treated with depot injections of neuroleptics (10). In a study of a large national sample of people with depression, Young and colleagues (11) found that African Americans were less likely than Caucasians to be treated in accord with official treatment guidelines. The Schizophrenia Patient Outcomes Research Team (PORT) Study has shown that among patients with schizophrenia, African Americans are less likely than Caucasians to receive a diagnosis of comorbid depression and to be treated accordingly, although objective measures show no difference in the frequency of depressive symptoms in the two groups (12).
Disparities have also been reported in the use of ECT. Thompson et al. (13) examined patterns of admissions and treatment from hospitals throughout the United States and found that white patients were more likely to be treated with ECT than patients of other races. Their data were biased in favor of private hospitals, but after the effects of this variable were controlled, the difference persisted. Other regional surveys have produced similar findings. Babigian and Guttmacher (14), in an analysis of case register data, found that in the years 1961–1975, among patients admitted for the first time for psychiatric inpatient treatment, white patients were more likely than black patients to be treated with ECT. The authors conjectured that the disparity is likely to be attributable to diagnostic differences. In a survey of the use of ECT in California between 1977 and 1983, a total of 18,627 patients received the treatment (15). The likelihood of receiving ECT, measured as the rate per 10,000 population, was three times greater for whites than for blacks. ECT was more likely to be prescribed in private hospitals, which may have contributed to the racial difference. In Texas, 5,971 patients were treated with ECT between 1993 and 1997 (16). Again, white patients were more likely than patients from other ethnic groups to be treated with ECT. In a 1993 nationwide study that analyzed treatment of recurrent major depression in 913 community hospitals in 17 states, black patients were less likely than white patients to be treated with ECT (odds ratio=0.7) (17).
This racial disparity is troubling because it suggests that psychiatrists may consciously or unconsciously make treatment decisions that are influenced by social or racial considerations rather than solely on the basis of the clinical needs of the patient. Of course there are several other possible explanations: the disparity may arise for clinical reasons, because of insurance coverage, or because of cultural differences in acceptance of this treatment. However, while previous research had repeatedly demonstrated the existence of a disparity, to our knowledge, no data have been published that provide a satisfactory explanation for the finding. Thus, we designed a study to examine data on ECT utilization in patients with affective disorders in the department of psychiatry of a large academic medical center. In this study, we use data from existing administrative databases for a large series of admissions of patients with affective disorder diagnoses. Seven hypotheses were considered:
| 1. | The apparent racial disparity arises because of confounding variables of age and sex. | ||||
| 2. | The disparity arises because certain treatment teams, which have an excess of Caucasian patients, are more likely to prescribe ECT. | ||||
| 3. | The disparity occurs because ECT is more likely to be offered to more affluent patients for reasons of insurance coverage or ability to pay for services. | ||||
| 4. | ECT is in most cases employed when other treatments have failed; there are more Caucasian patients admitted with treatment-resistant illnesses, accounting for the higher utilization of ECT in Caucasian patients. | ||||
| 5. | Tertiary referrals of “very-difficult-to-treat” patients from other hospitals or psychiatrists are more likely to involve Caucasian patients, and these patients are more likely to require ECT. | ||||
| 6. | The ICD-9 affective disorders category (296.x) is a “mixed bag,” and African American patients are clinically different from the Caucasian patients, although they carry the same diagnoses. | ||||
| 7. | African American patients with psychotic depression, who might be candidates for ECT, are misdiagnosed as having schizophrenia and thus are not included in the group of subjects selected for this study. | ||||
Method
In the period between November 1993 and March 2002, there were 17,914 admissions to the adult inpatient service of the department of psychiatry at an academic medical center. Of these, 1,086 (6.1%) were treated with ECT. From the total pool of admissions, subjects were selected for the study group as follows: All episodes of care for patients discharged with an ICD 296.x primary diagnosis were identified (N=7,118). Data for these admissions were extracted from the hospital’s administrative databases. Those patients whose race was documented as Caucasian or African American were selected for study. This group was further refined to exclude patients admitted to two short-stay admission units, because a high proportion of these patients had mood disorders associated with substance dependence and because the short length of stay on these units precluded the use of ECT. The remaining 5,243 admissions were used for analysis. Of these episodes of care, 878 (16.7%) involved treatment with ECT. This is not an unduplicated group of patients. It is a consecutive series of admissions, and certain patients were admitted more than once during the period.
To control for confounding variables, the data were stratified to examine the effects of age, race, sex, treatment unit, payer category, readmission status, and geographic area of the patient’s residence by using chi-square tests and odds ratio risk estimates. Multiple logistic regression analysis was employed to control for all of the potentially confounding variables simultaneously.
To permit comparisons of ECT utilization in patients with a diagnosis of schizophrenia, we selected a subgroup of patients (N=1,776) that included all patients discharged during the study period with a diagnosis in the schizophrenia spectrum (ICD 295.x).
Results
The age, sex, and race characteristics of the patients are shown in Table 1. A total of 61.3% of the patients were female, and 38.7% were male; 68.4% were Caucasian, and 31.6% were African American. The proportion of African Americans was greater in the younger age groups and declined progressively among patients age 45 years and older.
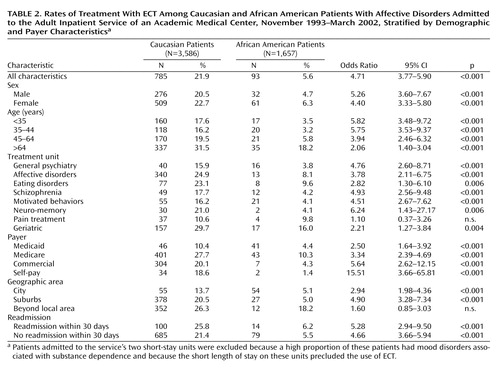
Caucasians had a significantly greater likelihood of being treated with ECT than African Americans (21.9% versus 5.6%) (odds ratio=4.71, 95% confidence interval [CI]=3.77–5.90, p<0.001).
Men were slightly, but significantly, less likely than women to be treated with ECT (15.2% versus 17.7%) (odds ratio=0.83, 95% CI=0.72–0.97, p<0.02).
A significant relationship was observed between age and ECT: the probability of being treated with ECT during the admission was fairly constant until age 45 years, at which time it increased steadily into old age (Figure 1). Of patients age 15–34 years, 12.7% had ECT; of those older than age 64 years, 29.5% had ECT. However, ECT rates for specific age groups showed that in every age group, the likelihood that Caucasian patients received ECT was significantly higher than that for African Americans. The odds ratios were greatest in the lower age groups (Table 2).
The rates of ECT on the different treatment units within the department were examined to ascertain whether the observed racial differences might result from different standards of practice in the different staff teams. Although there was considerable variation between units, on all but one unit, significantly higher ECT rates for Caucasian patients persisted (Table 2).
The patients were grouped according to the type of payer. This variable provides both an indirect measure of socioeconomic class and also may reveal any difference in practice that could be related to differences in coverage provided by various insurers. In each category, the racial disparity persisted (Table 2).
There were 757 patients who had been readmitted to the hospital within 30 days of a prior discharge. This measure of early readmission was used as an indicator of illness severity or failure of previous treatment attempts. Among patients with and without an early readmission, Caucasian patients were approximately four times more likely than African Americans to receive ECT.
Each patient was assigned to one of three geographic zones depending on where the patient resided: the city, the surrounding suburbs, or beyond. The composition of the city group was 49.5% African American, the group from the surrounding suburbs was 6.7% African American, and the group from beyond the local area was 3.3% African American. Patients in each group showed a racial disparity in use of ECT, although the difference in the group of patients from outside the local area was not statistically significant (Table 2).
To control for all the variables simultaneously, a multiple logistic regression analysis was performed. With all of the variables entered, the odds ratio for ECT for Caucasians relative to African Americans was 2.48 (95% CI=1.89–3.25, p<0.001).
Analysis of data for subjects with schizophrenia showed that African Americans were more likely than Caucasians to receive a diagnosis of schizophrenia (14% of all admissions versus 5%), but among patients with schizophrenia, Caucasians were more likely than African Americans to be treated with ECT (2.2% versus 0.5%) (odds ratio=4.27, 95% CI=1.58–11.55, p<0.005).
Discussion
These data confirm in the psychiatric department of a single academic medical center what has been shown elsewhere in national data sets—that African Americans with affective disorders are less likely than Caucasians to be treated with ECT.
We hoped that the data available to us would provide insights into the reasons for this disparity. The following hypotheses were examined:
1. This apparent racial disparity arises because of confounding variables of age and sex. The effect of age on utilization of ECT has been widely reported: older patients are more likely to be treated by this method than are younger patients, and it has been found that older patients respond better to ECT than younger patients (18). It has also usually been the case that samples of ECT patients have contained more women than men, although these findings appear to reflect different admission patterns rather than different ECT practice patterns (12, 14). Our data confirm both of these earlier findings: our study group included 570 women and 308 men who were treated with ECT. Nevertheless, the stratified treatment rates and odds ratios in excess of 4.4 for women and 5.3 for men demonstrate that the racial disparity exists for both sexes. The difference persists in every age group, although for patients older than age 64 years, the odds ratio was lowest—2.06, compared with 5.82 for the age group younger than 35 years. Thus, while age has an effect on use of ECT, the large observed racial disparity cannot be explained by the age composition of the study group.
The finding that the proportion of African American patients declined sharply in the older age groups is of interest. Data from a study of depression in African Americans in Norfolk, Virginia, suggested that the prevalence of major depression in the oldest age groups was less than anticipated, and the authors concluded that older African Americans may be less willing to acknowledge depression and less likely therefore to seek help (19). However, this explanation does not account for the lower rates of ECT in African American patients who are admitted for treatment.
2. The disparity arises because certain treatment teams, which have an excess of white patients, are more likely to prescribe ECT. Different treatment teams have different sources of referrals. If one team, with a predominantly white, middle-class, privately insured patient population, prescribed most of the ECT, this pattern could bias the overall finding. However, when data from the eight units in the adult inpatient service were analyzed separately, significant racial disparities were found in every case except one, the pain treatment program, where most of the patients were Caucasian and ECT was used less frequently. The racial disparity in the use of ECT existed on all other units, irrespective of the composition of their patient populations.
3. The disparity occurs because ECT is more likely to be offered to more affluent patients for reasons of insurance coverage or ability to pay for services. Thus, if the data are stratified by type of insurance, the racial discrepancy should disappear. In fact, the disparity persisted in each payer category. The “self-pay” group had the greatest disparity, but this group was very small, accounting for only 6% of the patients. Its influence in the overall pattern of disparity was small.
4. ECT is in most cases employed when other treatments have failed; there are more Caucasian patients admitted with treatment-resistant illnesses, accounting for the higher utilization of ECT in Caucasian patients. Thus, in the subgroup of patients from both racial groups for whom previous treatment efforts had been unsuccessful, the racial disparity should disappear. There would be no disparity among the remaining patients either. Patients for whom the current admission occurred within 30 days from a previous discharge were selected as “treatment failures.” In both this group and in the group of patients for whom the current admission was the only admission within the month, the odds of receiving ECT were five to six times higher for Caucasian patients, so that the disparity can not be explained on this basis.
5. Tertiary referrals of “very-difficult-to-treat” patients from other hospitals or psychiatrists are more likely to involve Caucasian patients, and these patients are more likely to require ECT. The hospital, in addition to the services it provides to local people, attracts referrals of patients from a wide geographic area who need or desire specialized services when treatment does not appear to be succeeding in their local treatment setting. These patients are more likely to be affluent, or well insured, and less likely to be members of minority groups. Consistent with this hypothesis, if patients who came from outside the local area are excluded from the analysis, there should be no racial discrepancy in ECT rates for the remaining patients, who are drawn from the local area. In fact, when the nonlocal patients were excluded, robust racial differences in ECT rates persisted for the patents from the local areas. A racial disparity existed also in the patients referred from outside the local area, but this difference did not reach statistical significance owing to the small number of African American patients in this group.
6. The ICD-9 affective disorders category (296.x) is a “mixed bag,” and African American patients are clinically different from the Caucasian patients, although they carry the same diagnoses. Our data set does not contain clinical information that permits us to address this question directly or to rule out this possibility definitively. However, for this analysis, we selected patients on the basis of primary diagnoses only and excluded patients with depressive disorders that were deemed to be of secondary importance in a particular case.
7. African American patients with psychotic depression, who might be candidates for ECT, are misdiagnosed as having schizophrenia and thus are not included in the group of subjects selected for this study. A diagnostic issue raised by the literature concerns the possible misdiagnosis of African Americans with affective disorders. Several studies have demonstrated that African Americans are more likely than Caucasians to receive a diagnosis of schizophrenia (4, 5, 7, 8). Discharge data from the hospital where the study was conducted also indicate that African American patients are more likely than Caucasians to receive a diagnosis of schizophrenia. Although there are many possible explanations for this disparity, including the demographic characteristics of the hospital’s patients and the social class distribution of schizophrenia, the possibility exists that African American patients with severe affective disorders are being placed in the wrong diagnostic category and are being treated for the wrong disorders. ECT is sometimes used in the treatment of schizophrenia spectrum disorders, often in the case of patients with a catatonic or affective component. If patients with affective disorders were being assigned a schizophrenia diagnosis, it would be predicted that they among all schizophrenic patients would be most likely to receive ECT. However, African Americans in the schizophrenia group were significantly less likely to be treated with ECT: the same fourfold disparity persisted, making it unlikely that the disparity observed in the patients with affective disorders can be explained by loss of severely ill patients into the schizophrenia group.
A multiple logistic regression analysis was performed to ascertain whether there might be interaction effects among the several variables that could account for the disparity. When all of the variables were entered, the odds ratio fell to 2.48. This result indicates that several variables contribute to the racial disparity, but they do not fully explain it. When the effects of all of these factors were controlled, Caucasian patients with affective disorders were still two and one-half times more likely than African Americans to be treated with ECT.
There are several possible explanations for this finding that would require further research with different methods. Hypothesis 6 was not adequately tested by this study—the hypothesis that mood disorders in people of different ethnic and cultural backgrounds may present with different symptom patterns and that these different presentations may affect physicians’ decisions to recommend particular treatments. African American patients may present patterns of symptoms that conform less often to the syndrome pattern believed to be most responsive to ECT. There is some evidence to support this possibility. One small study of patients with major depression found that African American and Caucasian patients exhibited different patterns of symptoms, even though, as judged by ratings on the Hamilton Depression Rating Scale, the overall severity of the depression was the same in both groups (20). Another study, of a series of patients with manic symptoms, demonstrated that African Americans and Caucasians exhibited different patterns of delusions and hallucinations (8).
Anecdotal reports from psychiatrists suggest another possibility—that patients from minority groups are less likely than Caucasian patients to consent to ECT. This possibility should be amenable to empirical testing. Some support for this hypothesis may come from a study that examined the coping resources of a group of patients with bipolar disorder (21). It was found that the African American patients scored significantly higher on several measures of coping. If this is so, African Americans may be more likely to believe they can get well without resorting to what is perceived as a dangerous treatment.
It is also possible that African Americans respond better to antidepressants, so that ECT, which is usually employed when other treatments fail, may be required less frequently. There is little information available on this question. More than three decades ago, Overall and colleagues (22) reported a finding that African Americans responded significantly better to a variety of psychotropic drugs, including tricyclic antidepressants. However, the relevance of this finding in today’s practice environment with newer classes of antidepressants is unclear. More recently, Bosworth et al. (23) found that in elderly patients treated with a variety of psychotropic medicines, psychosocial factors such as social support affected outcome, but race did not. Recent developments in ethnopharmacology are providing information about ethnic differences in the genetics of enzymes governing the metabolism of antidepressants and other drugs (24), which at least suggest that differential responses could occur (25).
Finally, there could be a conscious or unconscious bias in psychiatrists’ treatment decisions. Racial biases in psychiatric diagnoses have been studied extensively (4–8, 26, 27), but biases in treatment have not. Treatment decisions involve much individual judgment that can be affected by group or individual perceptions of particular classes of patients and their needs. Racial bias can lead to underdiagnosing certain conditions or, on the other hand, to pathologizing culturally normal behaviors or ideas (4). Most of the psychiatrists involved in the decision to prescribe ECT were Caucasian and may have been less sensitive to cultural expressions of depression in African American patients than in Caucasian patients, leading them to underestimate the severity of the illness. It could also be hypothesized that physicians felt less obligation or were subjected to less pressure to “leave no stone unturned” in seeking the best outcome for more disadvantaged patients, although there is no evidence to suggest that these processes occurred. Further research on physicians’ attitudes will be needed to address these questions.
The limitations of this study must be acknowledged. The patients were selected by convenience; however, the large number of patients and the fact that the study group included 100% of all admissions of Caucasian and African American patients with affective disorders to this hospital during the study period would suggest that the data are reflective of actual practice. Because this study was a retrospective review of data collected by the hospital for administrative purposes, the investigators could analyze only those variables that were included in the hospital’s administrative databases. More clinical data would have been desirable, for example, to provide some confirmation of the diagnoses assigned or to permit comparisons of clinical syndromes. The data were not collected for research, and the diagnoses were made by treating psychiatrists. This information and all other data were entered into the database by administrative personnel. Systematic errors may have been introduced by the process of collecting and storing the data, but these errors are unlikely to have been biased by race.
In summary, this study confirms that African American patients with affective disorders diagnoses are less likely than Caucasian patients to be treated with ECT. This disparity cannot be explained by the demographic or socioeconomic variables considered here. Other possible explanations relating to clinical presentation, differential response to other treatments, differences in patients’ willingness to consent, or physicians’ behavior will require further research.
 |
 |
Received June 5, 2003; revision received Oct. 20, 2003; accepted Nov. 12, 2003. From the Department of Psychiatry and Behavioral Sciences, Johns Hopkins Hospital. Address reprint requests to Dr. Breakey, Department of Psychiatry and Behavioral Sciences, Meyer 4-181, Johns Hopkins Hospital, 600 N. Wolfe St., Baltimore MD 21287-7481; [email protected] (e-mail). Supported in part by the Center for Research on Services for the Severely Mentally Ill, funded by NIMH grant MH-43703. The authors thank Mark Teitelbaum, M.D., Jack Samuels, Ph.D., and Peter Rabins, M.D., for their comments.
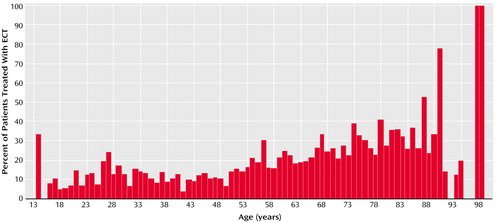
Figure 1. Percentages of Patients With Affective Disorders Admitted to the Adult Inpatient Service of an Academic Medical Center, November 1993–March 2002, Who Were Treated With ECT, by Agea
aPatients admitted to the service’s two short-stay units were excluded because a high proportion of these patients had mood disorders associated with substance dependence and because the short length of stay on these units precluded the use of ECT.
1. Mental Health: Culture, Race and Ethnicity—a Supplement to Mental Health: A Report of the Surgeon General. Rockville, Md, US Department of Health and Human Services, 2001Google Scholar
2. Institute of Medicine: Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Washington, DC, National Academies Press, 2003Google Scholar
3. Fiscella K, Franks P, Doescher MP, Saver BG: Disparities in health care by race, ethnicity, and language among the insured: findings from a national sample. Med Care 2002; 40:52–59Crossref, Medline, Google Scholar
4. Snowden LR: Bias in mental health assessment and intervention: theory and evidence. Am J Public Health 2003; 93:239–243Crossref, Medline, Google Scholar
5. Neighbors HW, Trierweiler SJ, Munday C, Thompson EE, Jackson JS, Binion VJ, Gomez J: Psychiatric diagnosis of African Americans: diagnostic divergence in clinician-structured and semistructured interviewing conditions. J Natl Med Assoc 1999; 91:601–612Medline, Google Scholar
6. Minsky S, Vega W, Miskimen T, Gara M, Escobar J: Diagnostic patterns in Latino, African American, and European American psychiatric patients. Arch Gen Psychiatry 2003; 60:637–644Crossref, Medline, Google Scholar
7. Strakowski SM, Flaum M, Amador X, Bracha HS, Pandurangi AK, Robinson D, Tohen M: Racial differences in the diagnosis of psychosis. Schizophr Res 1996; 21:117–124Crossref, Medline, Google Scholar
8. Strakowski SM, McElroy SL, Keck PE Jr, West SA: Racial influence on diagnosis in psychotic mania. J Affect Disord 1996; 39:157–162Crossref, Medline, Google Scholar
9. Lindsey KP, Paul GL: Involuntary commitments to public mental institutions: issues involving the overrepresentation of blacks and assessment of relevant functioning. Psychol Bull 1989; 106:171–183Crossref, Medline, Google Scholar
10. Citrome L, Levine J, Allingham B: Utilization of depot neuroleptic medication in psychiatric inpatients. Psychopharmacol Bull 1996; 32:321–326Medline, Google Scholar
11. Young AS, Klap R, Sherbourne CD, Wells KB: The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry 2001; 58:55–61Crossref, Medline, Google Scholar
12. Dixon L, Green-Paden L, Delahanty J, Lucksted A, Postrado L, Hall J: Variables associated with disparities in treatment of patients with schizophrenia and comorbid mood and anxiety disorders. Psychiatr Serv 2001; 52:1216–1222Link, Google Scholar
13. Thompson JW, Weiner RD, Myers CP: Use of ECT in the United States in 1975, 1980, and 1986. Am J Psychiatry 1994; 151:1657–1661Link, Google Scholar
14. Babigian HM, Guttmacher LB: Epidemiological considerations in electroconvulsive therapy. Arch Gen Psychiatry 1984; 41:246–253Crossref, Medline, Google Scholar
15. Kramer BA: Use of ECT in California, 1977–1983. Am J Psychiatry 1985; 142:1190–1192Link, Google Scholar
16. Scarano VR, Felthous AR, Early TS: The State of electroconvulsive therapy in Texas, part I: reported data on 41,660 ECT treatments in 5,971 patients. J Forensic Sci 2000; 45:1197–1202Medline, Google Scholar
17. Olfson M, Marcus S, Sackeim HA, Thompson J, Pincus HA: Use of ECT for the inpatient treatment of recurrent major depression. Am J Psychiatry 1998; 155:22–29Link, Google Scholar
18. O’Connor MK, Knapp R, Husain M, Rummans TA, Petrides G, Smith G, Mueller M, Snyder K, Bernstein H, Rush AJ, Fink M, Kellner C: The influence of age on the response of major depression to electroconvulsive therapy: a CORE Report. Am J Geriatr Psychiatry 2001; 9:382–390Crossref, Medline, Google Scholar
19. Brown DR, Ahmed F, Gary LE, Milburn NG: Major depression in a community sample of African Americans. Am J Psychiatry 1995; 152:373–378Link, Google Scholar
20. Wohi M, Lesser I, Smith M: Clinical presentations of depression in African American and white outpatients. Cult Divers Ment Health 1997; 3:279–284Crossref, Medline, Google Scholar
21. Pollack LE, Harvin S, Cramer RD: Coping resources of African American and white patients hospitalized for bipolar disorder. Psychiatr Serv 2000; 51:1310–1312Link, Google Scholar
22. Overall JE, Hollister LE, Kimbell I, Shelton J: Extrinsic factors influencing responses to psychotherapeutic drugs. Arch Gen Psychiatry 1969; 21:89–94Crossref, Medline, Google Scholar
23. Bosworth HB, Hays JC, George LK, Steffans DC: Psychosocial and clinical predictors of unipolar depression outcome in older adults. Int J Geriatr Psychiatry 2002; 17:238–246Crossref, Medline, Google Scholar
24. Lin KM, Smith MW, Ortiz V: Culture and psychopharmacology. Psychiatr Clin North Am 2001; 24:523–538Crossref, Medline, Google Scholar
25. Sramek JJ, Pi EH: Ethnicity and antidepressant response. Mt Sinai J Med 1996; 63:320–325Medline, Google Scholar
26. Adebimpe VR: Overview: white norms and psychiatric diagnosis of black patients. Am J Psychiatry 1981; 138:279–285Link, Google Scholar
27. Bell C, Mehta H: The misdiagnosis of black patients with manic-depressive illness. J Natl Med Assoc 1981; 73:101–107Medline, Google Scholar



