Suicide Attempts Associated With Externalizing Psychopathology in an Epidemiological Sample
Abstract
OBJECTIVE: Borrowing from recent dimensional models of psychopathology, the authors conducted analyses that optimized the common variance shared by internalizing (depression, anxiety) and externalizing (antisocial personality, substance dependence) disorders in statistically predicting suicidal behaviors. These relationships were analyzed in a large epidemiological sample, thus allowing for the examination of gender differences in risk for suicide attempts associated with psychopathology. METHOD: The data were obtained from the Colorado Social Health Survey. Participants (N=4,745) were a community sample recruited by household address. Structured clinical interviews were used to obtain lifetime diagnostic and symptom count information. Symptom counts were included in a factor analysis that yielded two main dimensions of psychopathology: internalizing and externalizing. These factors were used in hierarchical logistic regression analyses to predict history of suicide attempts associated with the presence of internalizing symptoms, externalizing symptoms, and comorbid internalizing and externalizing symptoms. RESULTS: After the investigators controlled for the presence of internalizing symptoms and the comorbidity of internalizing and externalizing symptoms, externalizing symptoms were related to suicidal behavior in both men and women, although comorbidity was most predictive of suicide attempts among women, compared to men. CONCLUSIONS: Suicidal behavior among individuals with externalizing symptoms is not necessarily a result of comorbid depressive or other internalizing disorder. Thus, persons exhibiting antisocial behaviors should receive rigorous assessment for suicidal ideation and behavior.
The growing incidence of suicidal acts among prisoners (1) and jail detainees (2) has heightened awareness of the risk for suicide among persons characterized by criminal, aggressive, and substance abuse behaviors. The importance of these “externalizing” syndromes, as well as of “internalizing” forms of psychopathology such as depressive disorders, in predicting suicide is well established (3–5). Most research examining suicide risk among individuals who exhibit externalizing syndromes has been conducted with forensic or psychiatric patients (6, 7). Although these subjects are often ideal for studies that examine extreme behaviors, their inclusion impedes disentangling the effects of incarceration or acute institutionalization from more stable underlying processes that place these persons at risk for suicide (8). Even in community samples, the risk for suicide among persons exhibiting acting-out behaviors may simply reflect risk associated with the comorbidity of such behaviors with an internalizing axis I disorder, such as depression (9, 10).
Mounting evidence supports the supposition that externalizing psychopathology represents a key risk factor for suicide. In this regard, Apter and colleagues (7, 11) identified at least two subtypes of individuals with suicidal behaviors: depressed/withdrawn and irritable/aggressive. They found that among violent male patients and adolescents with conduct disorder, sadness did not correlate with suicidal behavior. On the other hand, the correlation between depression and suicidal acts was significant for nonviolent hospital patients and adolescents with internalizing syndromes (7, 12). Although major depression is an important precipitant, suicide risk among individuals with externalizing disorders may instead be related to impulsive and anger-related behaviors. Despite this evidence, a few issues prevent firm conclusions about the roles of internalizing and externalizing psychopathology in suicidal behavior. First, in the studies just discussed, the study groups were composed of psychiatric patients, and we wanted to examine whether these relationships could be found in the general population. Second, prior research has not statistically controlled for depressive symptoms, or comorbidity between internalizing and externalizing disorders, in analyzing the relationship between externalizing disorders and suicidal behavior. Finally, few authors have examined gender differences in the effect of internalizing and externalizing disorders and their co-occurrence on suicidal behaviors in a large group of men and women from the community.
The high rate of comorbidity among mental disorders is relevant to the understanding of risk for suicide in different diagnostic groups. Epidemiological data support the high rate of comorbidity among depressive and anxiety disorders (13, 14), as well as the co-occurrence of externalizing symptoms (including antisocial and criminal behaviors, excessive alcohol use, and aggressive acting out) within individuals (15–18). Krueger (19) suggested that these patterns of comorbidity represent meaningful covariance. Specifically, he validated a two-factor model of common mental disorders (i.e., not including schizophrenia and bipolar disorder): an internalizing factor representing mood and anxiety disorders and an externalizing factor that included antisocial personality disorder and alcohol and other substance dependence. This dimensional model suggests that each factor (or cluster of related disorders) represents a common underlying process of psychopathology (20, 21).
Although some controversy exists in the interpretation of Krueger’s analyses (22), his conceptualization provides a parsimonious approach to examining the influence of a collection of correlated syndromes on outcomes. Following this framework, we attempted to validate this two-factor structure of mental disorders in an epidemiological sample and extended Krueger’s work by including both schizophrenia and bipolar disorder in these analyses to determine if these inclusions would change the factor structure. Then, factor scores were used in regression analyses to determine whether externalizing psychopathology predicts risk for suicide attempts above the variance accounted for by the presence of internalizing symptoms and comorbid internalizing and externalizing symptoms.
In addition, we were interested in whether these effects would be similar for both genders. Typically, women are more likely to experience depressive and internalizing symptoms and engage in suicide attempts (23–25), but externalizing behaviors are more strongly associated with men (26). Thus, we explored whether the effect of externalizing disorders on suicide was equally robust for both genders.
Method
Participants
The data for this study were obtained as part of the Colorado Social Health Survey (27), which included an epidemiological sample of the Colorado general adult population (N=4,745). The survey method was patterned after that of the Epidemiological Catchment Area program (see reference 28). During 1985–1986, participants were randomly sampled by household address, and potential respondents were then interviewed in their homes by trained lay interviewers. Participants were first provided with a description of the study, and they signed an informed consent form. Ciarlo and colleagues (27) have provided a full description of the Colorado Social Health Survey procedures. The mean age of the participants was 43.0 years (SD=17.5); 48% (N=2,265) of the sample were men, and 52% (N=2,479) were women. The ethnic composition of the sample was as follows: 2% (N=99) were Native American, Asian, or Pacific Islander; 4% (N=178) were African American; 84% (N=3,986) were Caucasian; and 10% (N=472) were Hispanic.
Diagnostic Assessment
Participants’ psychiatric disorders were assessed by means of the highly structured interview protocol of the National Institute of Mental Health Diagnostic Interview Schedule (DIS) (29). The DIS was used to obtain present and past DSM-III axis I diagnoses through a patterned series of specified questions. Questions pertaining to one axis II disorder, antisocial personality disorder, were also included in the interview. Robins and colleagues (29) have demonstrated that the DIS has adequate reliability (kappa coefficients ranging from 0.60 to 0.86), and sensitivity and specificity indices (true positive and true negative rates, respectively) that are in the adequate to excellent range (80%–94%).
The following diagnoses were assessed: bipolar disorder (manic), major depression, dysthymic disorder, schizophrenia, obsessive-compulsive disorder (OCD), phobic disorder, panic disorder, generalized anxiety disorder, alcohol abuse/dependence, other substance abuse/dependence, and antisocial personality disorder. The criteria for receiving a diagnosis followed directly from the criteria set forth in DSM-III. While there have been some modifications in diagnostic criteria from DSM-III to DSM-IV, for the most part changes have been minimal and there is considerable overlap. The fact that we conducted primary analyses by using symptom count variables (see later discussion) and not diagnoses largely resolves concerns about discrepancies in criteria across different versions of DSM. For the purposes of this study, lifetime diagnostic and symptom information were used as independent variables. Our hypothesis was that the vulnerability to externalizing disorders (evidenced by the participant’s having experienced a series of externalizing symptoms at some point in his or her lifetime), and not just the current presence of the syndrome, represents the underlying risk for suicidal acts.
The lifetime prevalence of generalized anxiety disorder (17%) in the Colorado Social Health Survey was higher than that reported in other samples (30), but the discrepancy was due mostly to the difference in duration criteria from DSM-III (1 month) to DSM-III-R and DSM-IV (6 months). A reanalysis of the data for this diagnosis by using more stringent duration criteria (i.e., symptoms that lingered or recurred for longer than 1 month) resulted in a lifetime prevalence (6.3%) similar to that found in other epidemiological studies (30). In addition, to avoid confounding diagnostic (major depression) and outcome (suicide) variables, major depression diagnoses and symptom counts were calculated with the omission of data from the survey questions about suicidal ideation or suicide attempts. This change affected 62 persons who would have met the criteria for a lifetime diagnosis of major depression but subsequently, with this revision, did not. It is interesting to note that the prevalence of suicide attempts among persons with a lifetime major depression diagnosis was very similar when we used the original criteria (24.6%) and when we used the revised criteria (24.3%). Dysthymic disorder, alcohol abuse, and other substance abuse were not included in the analyses because of symptom overlap with their more severe versions (major depression, alcohol dependence, and other substance dependence). A diagnosis of childhood conduct disorder was not used in the analyses of the dichotomous diagnostic variables because only adult diagnoses were included. However, a symptom count for childhood antisocial behavior was calculated for use in the factor analysis.
Symptom Count Variables
For the factor analysis and logistic regression analyses, we used symptom count variables (number of symptoms endorsed for each disorder), instead of the dichotomous diagnosis variables (present versus absent) (20, 21). Psychopathology researchers have argued that symptoms of mental disorders are distributed continuously in the population, with increasing symptom levels indicative of greater dysfunction (31). In addition, symptom count variables yield greater statistical power in studies of general population samples with lower base rates of psychopathology, compared with clinical samples (21). Moreover, Krueger (32) has confirmed that analyses of symptom counts result in distinct lifetime patterns of comorbidity that are not solely attributable to criterion overlap.
For each disorder, the symptom count variables corresponded to the following DSM-III criteria: for major depression, criteria A and B; for alcohol and other substance dependence, criteria A, B and C; for panic disorder, criteria A and B; for generalized anxiety disorder, criteria A and B; for phobic disorder, all symptom criteria; for OCD, criterion A; for schizophrenia, criteria A, B, and C; and for bipolar disorder (manic), criteria A and B. Antisocial personality disorder symptoms were divided into adult antisocial behavior and child antisocial behavior symptoms (i.e., DSM-III criterion C for antisocial personality disorder). The symptom count variables were positively skewed in distribution; thus, we used a rank-normalizing transformation previously used in these types of analyses (33).
History of Suicidal Behavior
As part of the assessment procedure, participants were asked about history of suicidal behavior. For purposes of this study, we chose to focus on suicide attempts, because a suicide attempt represents a more severe manifestation of suicidal behavior than does suicidal ideation. Although some data suggest that suicide attempters differ from persons who die by suicide (34), research indicates that self-harm not resulting in death is related to a high risk for eventual suicide (6, 35). A dichotomous variable representing lifetime history of suicide attempts was used as the dependent variable to ensure that we obtained a large enough group of suicide attempters for the analyses.
Statistical Analyses
First, chi-square analyses were conducted to determine whether lifetime diagnoses (present or absent) statistically predicted suicide attempt history. Then, we employed the common extraction method of principal axis factor analysis (20) to examine the relationships between the common mental disorders (i.e., the 11 transformed symptom count variables representing lifetime symptoms) previously described. Hierarchical logistic regression analyses were then performed, wherein dichotomous lifetime suicide attempt history was the criterion variable. Gender, the internalizing and externalizing factors that resulted from the factor analysis, and their interactions were included as independent variables in these regression analyses. A significant reduction in the (–2)log likelihood estimate from the restricted model (with the internalizing factor and gender as predictors) to the full model (which included the externalizing factor in a second step, the internalizing factor-by-externalizing factor interaction term in a third step, and the internalizing factor-by-externalizing factor-by-gender interaction in a final step) would represent an improvement in statistical prediction of suicide history, which was calculated as a chi-square statistic with a corresponding p value (36).
Results
History of Suicide Attempts Across Diagnostic Groups
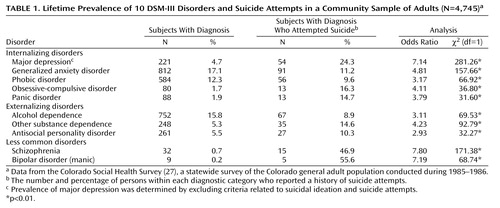
Across the overall sample, 173 persons (3.7% of the sample) reported that they had attempted suicide in their lifetime. Women were significantly more likely to report suicide attempts (N=128; 5.2% of women) than men (N=44; 1.9% of men) (χ2=35.14, df=1, N=4,744, p<0.001). Information on gender was not available for one person who reported a suicide attempt. As reported in Table 1, all lifetime diagnostic conditions (present versus absent, without regard to comorbidity) were significantly related to a history of suicide attempts. Since the large sample size may have influenced the p value estimates, we also calculated odds ratios and reported them in Table 1. It is typical to report odds ratios in such cases to best evaluate the contribution of each diagnostic syndrome in the prediction of suicide attempts (9). An examination of Table 1 reveals that, of the internalizing disorders, major depression confers the most risk for suicidal acts (37). The other internalizing disorders (anxiety disorders) and the externalizing disorders (antisocial personality disorder, alcohol dependence, and other substance dependence) were similarly predictive of suicide attempts.
As has been found in other work, schizophrenia and bipolar disorder (manic) were strongly associated with suicidal behaviors, with risk just slightly higher than that for major depression. Consistent with other epidemiological investigations, the base rates of schizophrenia (N=32) and bipolar disorder (manic) (N=9) were low (below 1%) in this sample, making conclusive statements about these relationships quite tenuous. In addition, all of the persons meeting the criteria for schizophrenia or bipolar disorder (manic), except one, met the criteria for another disorder. For both of these diagnoses, comorbidity was mostly with an internalizing disorder or with comorbid internalizing and externalizing disorders. Only four participants with a schizophrenia diagnosis had only an externalizing comorbid disorder.
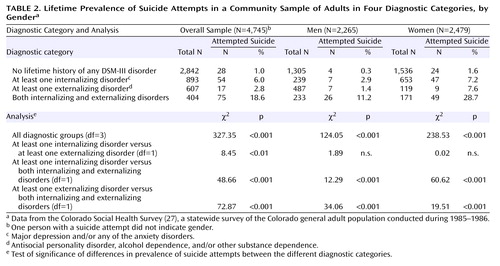
Among participants with a “pure” externalizing or internalizing disorder, women were more likely than men to have a history of an internalizing disorder (χ2=193.27, df=1, N=4,744, p<0.001). Men were more likely than women to have a history of an externalizing disorder (χ2=294.43, df=1, N=4,744, p<0.001) and of both internalizing and externalizing disorders (χ2=17.91, df=1, N=4,744, p<0.001). In Table 2, we present the prevalence of suicide attempts by diagnostic categories. Chi-square analyses revealed that participants in each of the psychopathology groups were more likely to have attempted suicide than participants with no prior psychopathology (Table 2). Those with only an internalizing diagnosis were slightly more likely to have attempted suicide than participants with only an externalizing diagnosis, although this result was not significant when analyses were conducted separately for men and women. Participants who met the criteria for both internalizing and externalizing diagnoses were more likely to attempt suicide than those with only an internalizing diagnosis or only an externalizing diagnosis (Table 2).
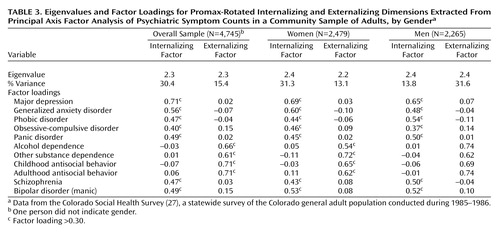
Latent Structure of Mental Disorders
Borrowing from the literature on dimensional models of psychopathology (19, 38), we conducted a principal axis factor analysis, with promax rotation, using the 11 symptom count variables described earlier. The scree plot and eigenvalues (>1) revealed a clear two-factor solution; factors other than the two major factors had trivial eigenvalues (Table 3 provides eigenvalues and factor loadings for the full sample and for each gender). The major depression, panic disorder, generalized anxiety disorder, and phobia symptom count variables loaded highly on the first factor (the internalizing factor), and OCD loaded moderately on this factor. The internalizing factor variables loaded negligibly on the second factor. Symptom counts for adulthood antisocial behavior, childhood antisocial behavior, alcohol dependence, and other substance dependence loaded highly on the second factor (the externalizing factor) and negligibly on the first factor. Separate analyses performed on the symptom count data for men and women revealed very similar two-factor solutions, indicative of internalizing and externalizing factors, for both genders (Table 3).
Schizophrenia and bipolar disorder symptoms loaded highly on the internalizing factor and negligibly on the externalizing factor (Table 3); this pattern may have occurred because persons with these symptoms were more likely to also have internalizing symptoms, as was discussed earlier. The result may also be an artifact of the low base rates of schizophrenia and bipolar disorder (manic) symptoms; thus, a separate factor could not be detected in the analyses. We excluded the schizophrenia and bipolar disorder symptom counts from the calculation of the two internalizing and externalizing factor scores because their inclusion may have confounded the interpretation of the two factors (since schizophrenia and bipolar disorder [manic] symptoms loaded on the internalizing factor and not on the externalizing factor). With this exclusion, scores on the internalizing and externalizing factors, extracted from the overall analyses, were used as independent variables in the regression analyses predicting suicide attempt history.
Risk for Suicide Associated With Internalizing and Externalizing Factors
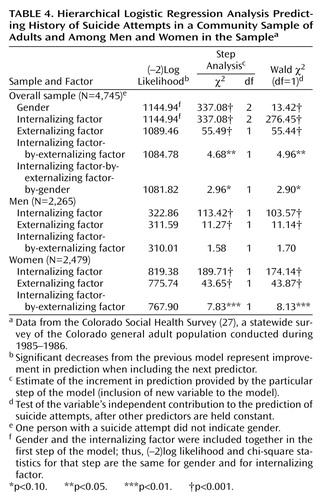
We conducted a hierarchical logistic regression analysis with four steps (Table 4 provides [–2]log likelihood, chi-square, and Wald statistics for all steps of the analysis). Gender and internalizing factor scores were included as predictors in the first step, which significantly improved prediction of suicide attempts above a constant. When externalizing factor scores were entered in a second block, the model fit was significantly improved. Then, the internalizing factor-by-externalizing factor interaction term was included in a third step, which also improved model fit. It is important to note that the contribution of the externalizing factor remained highly significant in this third step (Wald χ2=53.21, df=1, p<0.001). Finally, the internalizing factor-by-externalizing factor-by-gender interaction included in a final step was not significant in predicting suicide attempts (p=0.09) (Table 4). Also, in this step, the two-way internalizing factor-by-externalizing factor interaction became nonsignificant in this final step (p=0.74), whereas the externalizing factor main effect remained highly significant (Wald χ2=54.80, df=1, p<0.001).
Due to the significant gender differences on all the variables of interest (history of suicide attempts, internalizing factor, and externalizing factor), we also conducted hierarchical regression analyses separately by gender (independent variables included the internalizing factor, externalizing factor, and internalizing factor-by-externalizing factor) (Table 4). For women, the internalizing factor was a significant predictor in the first step and improved model fit above a constant, as did the externalizing factor in the second step of the model. In addition, the interaction between internalizing and externalizing factors was a significant predictor of suicide attempts in the final step; the interaction improved model fit further for women. For men, the internalizing factor in the first step and the externalizing factor in a second step both made independent significant contributions to prediction; however, for men, the internalizing factor-by-externalizing factor interaction term included in the third step of the analyses did not improve model fit significantly. These results suggest that when internalizing and externalizing factor effects are held constant, their co-occurrence plays a more influential role in suicidal behaviors among women than among men.
Discussion
An innovative aspect of this study was the application of dimensional models of psychopathology (19, 38) to the examination of relations between internalizing or externalizing symptoms and suicidal behavior. Although a large literature has confirmed relationships between suicidal behaviors and externalizing syndromes (5, 39–41), a number of these studies have been conducted with incarcerated or psychiatric subjects. Our results support the validity of the link between externalizing syndromes and suicidal behavior in a large community sample, confirming that this relationship is robust across psychopathological and “normal” populations.
In addition, our data provide support for the thesis that the relationship between a history of suicidal behavior and a history of impulsive, deviant (externalizing) behaviors is independent of internalizing symptoms and independent of comorbidity between internalizing and externalizing symptoms. Indeed, the results of the chi-square analyses of diagnostic categories showed that persons who had internalizing disorders did not differ in rate of suicide attempts from those with externalizing disorders. A more important finding was that the results of the regression analyses of symptom count data suggested that the common variance associated with these disorders (i.e., the externalizing factor dimension) is predictive of a history of suicide attempts. As suggested by Krueger and colleagues (19, 21), a common vulnerability factor may underlie the co-occurrence of externalizing behaviors; our data indicate that suicide risk among persons with externalizing syndromes may also be related to this common diathesis (5). The underlying mechanism in this relationship (e.g., impulsivity) would theoretically be different from the mechanism that links suicide to depressive and other internalizing disorders (e.g., hopelessness) (7, 11, 12).
Results from the current study point to other areas for future study. Research on normal personality links to psychopathology can help in identifying the common risk factor for externalizing and suicidal behaviors. For example, in a study by Verona et al. (42), analyses revealed that extremes in personality traits reflective of negative emotionality and (low) constraint accounted for the relationship between antisocial behavior history and suicide attempt history among male offenders. Moreover, Krueger and colleagues (20, 21) have confirmed that the externalizing spectrum of disorders is related to the genetically linked personality trait of low constraint. Although trait negative emotionality may represent vulnerability to both internalizing and externalizing psychopathology (and thus explain their comorbidity), low constraint seems to be related to engagement in externalizing versus internalizing behaviors (20). Application of this hypothesis to the relationship between suicidal behavior and externalizing symptoms should be examined directly in future work.
Another important contribution of this study is the analysis of relationships between psychopathology and suicidal behavior in men and women separately. As in earlier studies, women were more likely to engage in suicidal behaviors than men, probably because they had a higher prevalence of depression, which was a strong predictor of suicide attempts. However, externalizing psychopathology uniquely predicted suicidal behaviors in both genders, even though women showed fewer externalizing symptoms. On the other hand, women, more than men, showed strong relationships between comorbid externalizing and internalizing psychopathology and suicide attempt history. These results are only preliminary and require replication; however, they suggest that suicidal behaviors in women with externalizing symptoms may relate to the combination of emotional instability (such as depression or anxiety) and behavioral disconstraint (represented by acting-out behaviors) (43). This latter description is reminiscent of borderline personality traits, which are strongly linked to self-harm in women. Unfortunately, the Colorado Social Health Survey did not obtain information on borderline personality disorder, which is a limitation of this study. Thus, we could not investigate this hypothesis directly, although such an endeavor would be an important contribution in future work.
Some have suggested that substance dependence and antisocial personality disorder in men may be the equivalents of depression or anxiety in women and, thus, that externalizing syndromes may represent unrecognized depression in men (see reference 44). However, in our study, men were more likely than women to endorse both internalizing and externalizing symptoms; thus, the differential results for men and women are too preliminary to interpret fully. Nonetheless, these results suggest that gender differences in the link between psychopathology and suicide should be explored further in other samples in which rates of suicide attempt are higher, especially among male participants (see reference 45).
Certain limitations of the current study should be considered in interpreting the findings. The diagnosticians were lay interviewers; thus, our results need to be replicated in studies utilizing experienced clinical interviewers. Also, diagnosis and symptom assessment relied on DSM-III criteria, and future research should confirm these results using the most recent version of DSM. We also relied on participants’ retrospective reports, which is a limitation of using lifetime diagnosis and symptom counts. However, this strategy allowed us to obtain data from a large number of persons who endorsed psychopathological symptoms, increasing the reliability of our statistics. In addition, when analyses were performed by using more current (within the last year) information on diagnostic and suicidal behavior variables, we found similar results. Nonetheless, future research can examine, in a prospective or longitudinal fashion, whether initial symptoms of externalizing disorders predict later suicidal behaviors. An additional weakness of the current study is the binary index (yes/no) of suicidal behavior that was utilized. However, there was clear evidence for the validity of the index, in that it was correlated in predicted ways with diagnostic variables (particularly the high concordance of suicidal behavior with depression). Nonetheless, this limitation should be remedied in future research to help uncover differences in the nature of suicidal acts performed by antisocial individuals, compared with clinically depressed individuals (16).
Another weakness of this study is that we could not fully examine the important relationship between suicide and symptoms of schizophrenia and bipolar disorder, because of the low base rates of these syndromes in the studied population. In extending Krueger’s work, we did find that these two symptom clusters tended to load on the internalizing factor of psychopathology. However, our factor analytic results need to be replicated in future research, which should examine further the relationship of schizophrenia and bipolar disorder symptoms with externalizing disorders and suicidal behaviors.
Our results also have clinical implications. In general, this work informs the development of interventions to prevent individuals from engaging in behaviors that are destructive to the self and to others. Our results suggest that clinicians and treatment providers would benefit from paying closer attention to the assessment of suicidal impulses in persons exhibiting externalizing behaviors, even if they do not (but especially when they do) present with comorbid depression.
 |
 |
 |
 |
Received Jan. 7, 2003; revision received July 29, 2003; accepted Aug. 11, 2003. From the Department of Psychology, Kent State University; and the Department of Psychology, Florida State University, Tallahassee. Address reprint requests to Dr. Verona, Department of Psychology, Kent State University, Kent, OH 44242; [email protected] (e-mail). Supported by NIMH grant MH-377698.
1. Haycock J: Crimes and misdemeanors: a review of recent research on suicides in prisons. Omega: J Death and Dying 1991; 23:81–94Crossref, Google Scholar
2. McKee GR: Lethal vs nonlethal suicide attempts in jail. Psychol Rep 1998; 82:611–614Crossref, Medline, Google Scholar
3. Shafii M, Carrigan S, Whittinghill JR, Derrick A: Psychological autopsy of completed suicide in children and adolescents. Am J Psychiatry 1985; 142:1061–1064Link, Google Scholar
4. Brent DA, Johnson BA, Perper JA, Connolly J, Bridge J, Bartle S, Rather C: Personality disorder, personality traits, impulsive violence, and completed suicide in adolescents. J Am Acad Child Adolesc Psychiatry 1994; 33:1080–1086Crossref, Medline, Google Scholar
5. Verona E, Patrick CJ: Suicide risk in externalizing syndromes: temperamental and neurobiological underpinnings, in Suicide Science: Expanding the Boundaries. Edited by Joiner TE, Rudd D. Boston, Kluwer Academic, 2000, pp 137–173Google Scholar
6. Ivanoff A: Background risk factors associated with parasuicide among male prison inmates. Crim Justice Behav 1992; 19:426–436Crossref, Google Scholar
7. Apter A, Kotler M, Sevy S, Plutchik R, Brown SL, Foster H, Hillbrand M, Korn ML, van Praag HM: Correlates of risk of suicide in violent and nonviolent psychiatric patients. Am J Psychiatry 1991; 148:883–887Link, Google Scholar
8. Kupers TA: Trauma and its sequelae in male prisoners: effects of confinement, overcrowding, and diminished services. Am J Orthopsychiatry 1996; 66:189–196Crossref, Medline, Google Scholar
9. Aharonovich E, Liu X, Nunes E, Hasin DS: Suicide attempts in substance abusers: effects of major depression in relation to substance use disorders. Am J Psychiatry 2002; 159:1600–1602Link, Google Scholar
10. Mann JJ, Waternaux C, Haas GL, Malone KM: Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry 1999; 156:181–189Abstract, Google Scholar
11. Apter A, Gothelf D, Orbach I, Weizman R, Ratzoni G, Har-Even D, Tyano S: Correlation of suicidal and violent behavior in different diagnostic categories in hospitalized adolescent patients. J Am Acad Child Adolesc Psychiatry 1995; 34:912–918Crossref, Medline, Google Scholar
12. Apter A, Bleich A, Plutchik R, Mendelsohn S: Suicidal behavior, depression, and conduct disorder in hospitalized adolescents. J Am Acad Child Adolesc Psychiatry 1988; 27:696–699Crossref, Medline, Google Scholar
13. Kessler RC, Stang PE, Wittchen HU, Ustun TB, Roy-Byrne PP, Walters EE: Lifetime panic-depression comorbidity in the National Comorbidity Survey. Arch Gen Psychiatry 1998; 55:801–808Crossref, Medline, Google Scholar
14. Brown TA, Barlow DH: Comorbidity among anxiety disorders: implications for treatment and DSM-IV. J Consult Clin Psychol 1992; 60:835–844Crossref, Medline, Google Scholar
15. Virkkunen M: Alcoholism and antisocial personality. Acta Psychiatr Scand 1979; 59:493–501Crossref, Medline, Google Scholar
16. Moeller FG, Dougherty DM, Lane SD, Steinberg JL, Cherek DR: Antisocial personality disorder and alcohol-induced aggression. Alcohol Clin Exp Res 1998; 22:1898–1902Crossref, Medline, Google Scholar
17. Jaffe JH, Babor TF, Fishbein DH: Alcoholics, aggression and antisocial personality. J Stud Alcohol 1988; 49:211–218Crossref, Medline, Google Scholar
18. Ohannessian CM, Stabenau JR, Hesselbrock VM: Childhood and adulthood temperament and problem behaviors and adulthood substance use. Addict Behav 1995; 20:77–86Crossref, Medline, Google Scholar
19. Krueger R: The structure of common mental disorders. Arch Gen Psychiatry 1999; 56:921–926Crossref, Medline, Google Scholar
20. Krueger RF, McGue M, Iacono WG: The higher-order structure of common DSM mental disorders: internalization, externalization, and their connections to personality. Pers Individ Dif 2001; 30:1245–1259Crossref, Google Scholar
21. Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M: Etiologic connections among substance dependence, antisocial behavior, and personality: modeling the externalizing spectrum. J Abnorm Psychol 2002; 111:411–424Crossref, Medline, Google Scholar
22. Borsboom D: The structure of the DSM. Arch Gen Psychiatry 2002; 59:569–570Crossref, Medline, Google Scholar
23. Runeson B: Psychoactive substance use disorder in youth suicide. Alcohol Alcohol 1990; 25:561–568Medline, Google Scholar
24. Cairns RB, Peterson G, Neckerman HJ: Suicidal behavior in aggressive adolescents. J Clin Child Psychol 1988; 17:298–309Crossref, Google Scholar
25. Marttunen MJ, Aro HM, Henriksson MM, Lonnqvist JK: Antisocial behavior in adolescent suicide. Acta Psychiatr Scand 1994; 89:167–173Crossref, Medline, Google Scholar
26. Cowen B: Women and crime, in Violence and the Prevention of Violence. Edited by Adler L, Denmark F. Westport, Conn, Praeger, 1995, pp 157–168Google Scholar
27. Ciarlo J, Shern D, Tweed D, Kilpatrick L, Sachs Ericsson N II: The Colorado Social Health Survey of Mental Health Needs: sampling, instrumentation, and major findings. Eval Program Plann 1992; 15:133–148Crossref, Google Scholar
28. Regier DA, Myers JK, Kramer M, Robins LN, Blazer DG, Hough RL, Eaton WW, Locke BZ: The NIMH Epidemiologic Catchment Area Program: historical context, major objectives, and study population characteristics. Arch Gen Psychiatry 1984; 41:934–941Crossref, Medline, Google Scholar
29. Robins LN, Helzer JE, Croughan J, Ratcliff KS: The National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Arch Gen Psychiatry 1981; 38:381–389Crossref, Medline, Google Scholar
30. Blazer DG, Hughes D, George LK, Swartz M, Boyer J: Generalized anxiety disorder, in Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. Edited by Robins L, Regier D. New York, Free Press, 1991, pp 180–203Google Scholar
31. Robins LN, Price R: Adult disorders predicted by childhood conduct problems: results from the NIMH Epidemiologic Catchment Area project. Psychiatry 1991; 54:116–132Crossref, Medline, Google Scholar
32. Krueger R: Reply to D Borsboom: The structure of the DSM (letter). Arch Gen Psychiatry 2002; 59:570–571Google Scholar
33. van den Oord EJCG, Simonoff E, Eaves LJ, Pickles A, Silberg J, Maes H: An evaluation of different approaches for behavior genetic analyses with psychiatric symptom scores. Behav Genet 2000; 30:1–18Crossref, Medline, Google Scholar
34. Brent DA, Perper JA, Goldstein CE, Kolko DJ, Allan MJ, Allman CJ, Zelenak JP: Risk factors for adolescent suicide: a comparison of adolescent suicide victims with suicidal inpatients. Arch Gen Psychiatry 1988; 45:581–588Crossref, Medline, Google Scholar
35. Cross CK, Hirschfeld RMA: Psychosocial factors and suicidal behavior: life events, early loss, and personality. Ann NY Acad Sci 1986; 487:47–62Crossref, Medline, Google Scholar
36. Cohen J, Cohen P: Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. Hillsdale, NJ, Lawrence Erlbaum Associates, 1983Google Scholar
37. LeCubrier Y: The influence of comorbidity on the prevalence of suicidal behavior. Eur Psychiatry 2001; 16:395–399Crossref, Medline, Google Scholar
38. Clark LA, Watson D: Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. J Abnorm Psychol 1991; 100:316–336Crossref, Medline, Google Scholar
39. Plutchik R, van Praag HM: Psychosocial correlates of suicide and violence risk, in Violence and Suicidality: Perspectives in Clinical and Psychobiological Research. Edited by van Praag HM, Plutchik R, Apter A. New York, Brunner/Mazel, 1990, pp 37–65Google Scholar
40. Murphy GE, Wetzel RD: The lifetime risk of suicide in alcoholism. Arch Gen Psychiatry 1990; 47:383–392Crossref, Medline, Google Scholar
41. Virkkunen M, DeJong J, Bartko J, Linnoila M: Psychobiological concomitants of history of suicide attempts among violent offenders and impulsive fire setters. Arch Gen Psychiatry 1989; 46:604–606Crossref, Medline, Google Scholar
42. Verona E, Patrick CJ, Joiner TJ: Psychopathy, antisocial personality, and suicide risk. J Abnorm Psychol 2001; 110:462–470Crossref, Medline, Google Scholar
43. Wichstrom L, Rossow I: Explaining the gender difference in self-reported suicide attempts: a nationally representative study of Norwegian adolescents. Suicide Life Threat Behav 2002; 32:101–116Crossref, Medline, Google Scholar
44. Sachs-Ericsson N: Gender, social roles and suicidal ideation and attempts in a general population sample, in Suicide Science: Expanding the Boundaries. Edited by Joiner TE, Rudd D. Boston, Kluwer Academic, 2000, pp 201–220Google Scholar
45. Gunnell D, Rasul F, Stansfeld SA, Hart CL, Davey Smith G: Gender differences in self-reported minor mental disorder and its association with suicide. Soc Psychiatry Psychiatr Epidemiol 2002; 37:457–459Crossref, Medline, Google Scholar



