Cholesterol Metabolism and Suicidality in Smith-Lemli-Opitz Syndrome Carriers
Abstract
OBJECTIVE: The authors examined the relationship between cholesterol metabolism and suicidality in carriers of Smith-Lemli-Opitz syndrome and their families. This population has a partial deficiency in 7-dehydrocholesterol reductase (DHCR7), the enzyme that catalyzes the last step in cholesterol biosynthesis. METHOD: Suicidal behavior, depression, misuse of alcohol and drugs, and family history of psychopathology, including attempted or completed suicide, were assessed by structured interview in 51 carriers of Smith-Lemli-Opitz syndrome and 54 matched comparison subjects. RESULTS: There were significantly more suicide attempters and completers among the biological relatives of Smith-Lemli-Opitz syndrome carriers than comparison subjects, but family history of psychopathology did not significantly differ between the groups. More suicide attempts were reported among Smith-Lemli-Opitz syndrome carriers than among the comparison subjects. CONCLUSIONS: These results, based on a unique study design, provide additional evidence supporting the relationship between cholesterol metabolism and suicidal behavior.
It is well established that individuals with a family history of suicide are at greater risk of attempted and completed suicide (1). This fact, combined with consistent evidence from twin and adoption studies, suggests that there is a genetic component to suicidal behavior (2). Interest in cholesterol as a biological marker of suicide risk has emerged following consistent evidence from studies that used different designs suggesting the existence of an association between low serum cholesterol and suicidal behavior (3). Investigating suicidal behavior in a population having natively low cholesterol because of a particular genetic variation is an interesting and novel approach to the further exploration and validation of this association.
Smith-Lemli-Opitz syndrome is an autosomal recessive multiple malformation and mental retardation syndrome characterized by abnormally low cholesterol levels resulting from mutations in the gene coding for the enzyme 7-dehydrocholesterol reductase (DHCR7), which is involved in cholesterol biosynthesis (4). Smith-Lemli-Opitz syndrome has an estimated incidence of between one in 10,000 and one in 60,000 births (5) and a carrier frequency estimated as high as one in 30 (6). Many patients with Smith-Lemli-Opitz syndrome exhibit behavioral difficulties (aggressive and self-injurious behaviors), and dietary cholesterol supplementation has been shown to reduce aggression in these patients and improve their behavioral problems (7). Parents of Smith-Lemli-Opitz syndrome children are obligate heterozygotes and are clinically normal but are carriers of a partial enzyme deficiency, displaying reduced DHCR7 activity in the biosynthesis of cholesterol (8).
We explored the putative relationship between low cholesterol and suicide by investigating whether suicidal behavior would be more frequent in Smith-Lemli-Opitz syndrome carriers than comparison subjects, given the influence of the genetic variant on cholesterol metabolism in this population.
Method
The subjects were individuals who were heterozygous for Smith-Lemli-Opitz syndrome. They were recruited through health care centers across the United States and Canada where Smith-Lemli-Opitz syndrome patients and their families are followed. In all instances, Smith-Lemli-Opitz syndrome carriers were identified as the biological parents of a child diagnosed with Smith-Lemli-Opitz syndrome. We took into account the important influence of caregiver stress by selecting a comparison group consisting of individuals who were parents of a child with a chronic debilitating disorder (excluding autism and disorders resulting from inborn errors of cholesterol metabolism) requiring a level of care similar to that needed by a child with Smith-Lemli-Opitz syndrome.
Parents or primary caregivers of children being assessed or followed up at the genetics clinics of collaborating pediatric health care centers in the United States and Canada were invited to participate in the research study. Individuals with hypocholesterolemia, taking lipid-lowering medications, or suffering from acute or chronic psychosis, neurological disorders, or disorders of lipid metabolism were excluded from the study. Additionally, since Smith-Lemli-Opitz syndrome is most common among Caucasians of European origin, only individuals of European ancestry were included as comparison subjects.
All subjects were contacted for a comprehensive interview. Information on sociodemographic characteristics was collected, and medical and psychiatric histories, suicidality, and detailed family history were systematically assessed through self-administrated and structured interviews. History of major depression and misuse of alcohol or other substances was ascertained by using a modified version of the Structured Clinical Interview for DSM-IV. Suicidality was examined in terms of suicidal thoughts and suicide attempts. A detailed history of attempted suicide, including intent and lethality rating, was taken for each subject reporting a past suicide attempt. A suicide attempt was defined as a voluntary self-destructive act with lethal intent. Current depressive mood state was controlled for and measured by using the 21-item Beck Depression Inventory (9). After complete description of the study to the subjects, written informed consent was obtained from all who participated. This multicenter study was approved by local institutional review boards.
Pearson’s chi-square or Fisher’s exact test was used to compare dichotomous variables between carriers and comparison subjects. Student’s t test was used to compare continuous variables. All tests were two-tailed, and significance was accepted at the level of p<0.05. Statistical analyses were performed with SPSS Version 10 (SPSS, Inc., Chicago).
Results
The subjects were 51 carriers of Smith-Lemli-Opitz syndrome and 54 comparison subjects who were not carriers. All subjects were Caucasian, and carriers and comparison subjects were comparable with respect to all major demographic variables examined, including age (mean=33.7 years, SD=8.4, for carriers and mean=39.2 years, SD=6.4, for comparison subjects) (t=–0.89, df=103, p=0.37), sex (62.7% of the carriers and 61.1% of the comparison subjects were female) (χ2=0.03, df=1, p=0.86), and socioeconomic status.
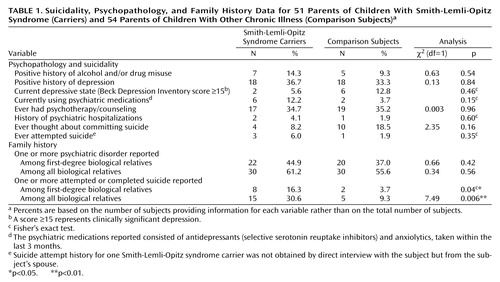
A striking difference was observed in family history of suicidal behavior between Smith-Lemli-Opitz syndrome carriers and comparison subjects, even though the two groups did not differ significantly on family history of psychiatric disorders (Table 1). Over 30% of Smith-Lemli-Opitz syndrome carriers but only 9% of comparison subjects reported having at least one biological relative who attempted or committed suicide (odds ratio=4.32, 95% confidence interval [CI]=1.31–16.45). Moreover, there were nine suicide attempters or completers among the 284 first-degree relatives of Smith-Lemli-Opitz syndrome carriers but only two among 360 first-degree relatives of comparison subjects (not shown in Table 1) (odds ratio=5.86. 95% CI=1.20–56.01).
Smith-Lemli-Opitz syndrome carriers and comparison subjects did not significantly differ overall for the major features of psychiatric history assessed (Table 1). A large proportion of both carriers and comparison subjects had a positive history of major depression and reported having seen a psychologist or a psychiatrist for counseling or psychotherapy. In most cases, this was related to the stresses associated with the child’s illness, marital problems, and/or alcohol or drug problems. A small proportion of subjects had a history of psychiatric hospitalization for reasons including attempted suicide (one female Smith-Lemli-Opitz syndrome carrier) and alcohol and drug treatment (one male Smith-Lemli-Opitz syndrome carrier and one female comparison subject).
None of the subjects reported having any current suicidal thoughts, and the two groups did not differ significantly with respect to reporting ever having thoughts about committing suicide in the past. Among comparison subjects, only a single suicide attempt was reported, involving a low-lethality overdose of over-the-counter diet pills. In contrast, five suicide attempts were reported by three Smith-Lemli-Opitz syndrome carriers; methods used included overdose of over-the-counter pills, deliberate attempt to crash car, interrupted attempt with a gun, and interrupted inhalation of car exhaust fumes.
Discussion
Family history of suicidal behavior was significantly different between Smith-Lemli-Opitz syndrome carriers and comparison subjects irrespective of family history of psychopathology: there were significantly more reports of suicide attempters and completers among the biological relatives of Smith-Lemli-Opitz syndrome carriers. The direct assessment of carriers indicated that more Smith-Lemli-Opitz syndrome carriers than comparison subjects had a history of attempted suicide, although this finding did not reach statistical significance, probably reflecting power sample size limitations, which in turn were consequent to the fact that Smith-Lemli-Opitz is a rare syndrome. Nevertheless, overall, more Smith-Lemli-Opitz syndrome carriers had attempted suicide, with repeated attempts and more violent and impulsive methods than comparison subjects.
The high proportion of both Smith-Lemli-Opitz syndrome carriers and comparison subjects who had a positive history of major depression in most cases reflected the stresses associated with caring for a child with a chronic debilitating disorder. Although it is important that the comparison subjects were matched with Smith-Lemli-Opitz syndrome carriers in terms of caregiver stress, it is also important to consider that this group is not representative of the general population because of the high rate of depression.
The finding that family history of suicidality but not psychopathology differed significantly between the groups is consistent with the finding from other studies suggesting that the familial transmission of suicide risk is discrete from that of psychiatric illness (1). The possibility emerges of investigating DHCR7 and similar genes as possible genetic factors mediating predisposition to suicidal behavior.
Our results suggest that Smith-Lemli-Opitz syndrome carriers may be at greater risk for suicidal behavior. Although possible mechanisms that may explain this observation remain unclear, it is reasonable to postulate that, given the reduced DHCR7 activity in Smith-Lemli-Opitz syndrome carriers, they may have a disturbance in brain sterol composition—either altered cholesterol and/or presence of 7-dehydrocholesterol or 7-dehydrodesmosterol—that could affect CNS function and behavior. This theory is in agreement with recent evidence that because cholesterol plays an important role in CNS synaptogenesis (10), CNS cholesterol alterations may impair development or plasticity of the synaptic circuitry involved in mediating behavior. Serum cholesterol may be a marker of CNS cholesterol metabolism, although the relationship between brain and serum cholesterol is not understood.
The results of this study provide additional support for the relationship between cholesterol metabolism and suicidality by means of a novel approach. It would be interesting to replicate these findings in other conditions that, like Smith-Lemli-Opitz syndrome, lead to low levels of cholesterol.
 |
Received Oct. 9, 2003; revision received Jan. 25, 2004; accepted March 10, 2004. From the McGill Group for Suicide Studies, Douglas Hospital Research Centre, McGill University, Montreal, Quebec, Canada. Address reprint requests to Dr. Turecki, McGill Group for Suicide Studies, Douglas Hospital Research Centre, 6875 LaSalle Blvd., Verdun, Quebec H4H 1R3, Canada; [email protected] (e-mail). Supported in part by the Réseau de Santé Mentale et Neuroscience du Québec, Suicide Axis. Dr. Turecki is a Canadian Institutes of Health Research scholar. Dr. Steiner is a Clinical Associate Physician Investigator of the General Clinical Research Centers, funded by U.S. Public Health Service grant 5 M01 RR-00334-33S3.
1. Brent DA, Bridge J, Johnson BA, Connolly J: Suicidal behavior runs in families: a controlled family study of adolescent suicide victims. Arch Gen Psychiatry 1996; 53:1145–1152Crossref, Medline, Google Scholar
2. Turecki G: Suicidal behavior: is there a genetic predisposition? Bipolar Disord 2001; 3:335–349Crossref, Medline, Google Scholar
3. Golomb BA: Cholesterol and violence: is there a connection? Ann Intern Med 1998; 128:478–487Crossref, Medline, Google Scholar
4. Wassif CA, Maslen C, Kachilele-Linjewile S, Lin D, Linck LM, Connor WE, Steiner RD, Porter FD: Mutations in the human sterol delta7-reductase gene at 11q12–13 cause Smith-Lemli-Opitz syndrome. Am J Hum Genet 1998; 63:55–62Crossref, Medline, Google Scholar
5. Nowaczyk MJ, Waye JS: The Smith-Lemli-Opitz syndrome: a novel metabolic way of understanding developmental biology, embryogenesis, and dysmorphology. Clin Genet 2001; 59:375–386Crossref, Medline, Google Scholar
6. Battaile KP, Battaile BC, Merkens LS, Maslen CL, Steiner RD: Carrier frequency of the common mutation IVS8–1G>C in DHCR7 and estimate of the expected incidence of Smith-Lemli-Opitz syndrome. Mol Genet Metab 2001; 72:67–71Crossref, Medline, Google Scholar
7. Elias ER, Irons MB, Hurley AD, Tint GS, Salen G: Clinical effects of cholesterol supplementation in six patients with the Smith-Lemli-Opitz syndrome (SLOS). Am J Med Genet 1997; 68:305–310Crossref, Medline, Google Scholar
8. Shefer S, Salen G, Honda A, Batta A, Hauser S, Tint GS, Honda M, Chen T, Holick MF, Nguyen LB: Rapid identification of Smith-Lemli-Opitz syndrome homozygotes and heterozygotes (carriers) by measurement of deficient 7-dehydrocholesterol-delta 7-reductase activity in fibroblasts. Metabolism 1997; 46:844–850Crossref, Medline, Google Scholar
9. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J: An inventory for measuring depression. Arch Gen Psychiatry 1961; 4:561–571Crossref, Medline, Google Scholar
10. Mauch DH, Nagler K, Schumacher S, Goritz C, Muller EC, Otto A, Pfrieger FW: CNS synaptogenesis promoted by glia-derived cholesterol. Science 2001; 294:1354–1357Crossref, Medline, Google Scholar



