Long-Term Course of Schizophrenic Illness: Bleuler’s Study Reconsidered
Abstract
OBJECTIVE: The influential 1972 study by Manfred Bleuler on the long-term course of schizophrenic illness has been reconsidered. The authors tested the diagnosis of schizophrenia in all patients and investigated how the distribution of the types of illness course and outcome would change after exclusion of patients whose diagnosis of schizophrenia could not be confirmed by modern diagnostic standards. METHOD: Clinical charts and Bleuler’s research notes on the original sample were assessed, and all patients were rediagnosed with the help of DSM-IV, DSM-III-R, ICD-10, the Research Diagnostic Criteria (RDC), Schneider’s criteria, and an operationalized version of the criteria of Eugen Bleuler. RESULTS: The diagnosis of schizophrenia was not confirmed in about 30% of the sample; the majority of these patients were rediagnosed with schizoaffective disorder. High diagnostic agreement was found between DSM-IV, DSM-III-R, ICD-10, and RDC; there was much less agreement with Bleuler’s and Schneider’s criteria. After exclusion of patients whose schizophrenia diagnosis was not confirmed, the proportion of patients with undulating course and recovery slightly decreased, and the proportion of patients with severe end state slightly increased. Nevertheless, the distribution of the types of long-term course did not significantly change, and even among patients with strictly defined schizophrenia, half had an undulating course with remissions and 12%–15% recovered. CONCLUSIONS: Schizophrenic illness remains heterogeneous with regard to illness course and outcome even when narrowly diagnosed with the help of modern operationalized diagnostic criteria. Contemporary differentiation between schizophrenic and schizoaffective disorders is prognostically valid.
The schizophrenia study by Manfred Bleuler (1) still belongs—with some other studies (2–5)—among the most important long-term follow-up investigations of the disorder. In that study the majority of 208 patients, all of them diagnosed with schizophrenia and personally known to Bleuler, were followed up over 20 years. The course of their illness was meticulously reconstructed, and eight types of course of schizophrenic illness were identified. The diagnosis was based on the schizophrenia concept set forth by Eugen Bleuler (6), and as Manfred Bleuler put it, the diagnosis was more oriented toward the entire syndrome than toward the sum of individual symptoms. The duration of the psychosis (that is, the time criterion) was not considered in the diagnostic process, and on the whole, no operationalized diagnoses were given.
We decided to rediagnose the patients of Bleuler’s original sample with the help of several sets of modern diagnostic criteria and to test whether we could confirm the types of long-term course of schizophrenia delineated by Bleuler after the exclusion of patients who would not fulfill the diagnostic criteria for schizophrenic disorder according to the contemporary standards. Viewed from another perspective, our retrospective study covering an exceptionally long observation period represents a contribution to the exploration of the course of schizophrenic illness diagnosed by modern criteria. As these criteria have only relatively recently been developed, corresponding prospective data are not available at present.
Method
Original Patient Sample
The original sample in Bleuler’s study encompassed 100 male and 108 female patients, all of them hospitalized at the Psychiatric Hospital Burghölzli during the recruitment phase of the study, from April 1942 to December 1943. Sixty-eight of them had been admitted for the first time, and 140 had been readmitted. The mean age of the patients at the time of study inclusion was 40 years (range=16–67 years). Out of 208 patients, 119 (57%) were single, 58 (28%) were married, five (2%) were widowed, and 26 (13%) were divorced. There were no statistical differences between the sexes with regard to marital status. According to Bleuler, the patients were representative of all schizophrenia patients hospitalized in the canton of Zurich during that period except for their slightly lower social class and higher age.
A number of the older patients were diagnosed with schizophrenia by Eugen Bleuler; the younger ones were diagnosed by Manfred Bleuler. Symptoms of particular diagnostic significance were schizophrenic distractedness of thinking (loosening of associations), loss of customary capability for affective contact, severe ego disturbances (such as transitivism, obedience automatism, identity loss, thought hearing, feeling of complete personality change), and severe catatonic muscular symptoms.
Assessment of Illness Course
Manfred Bleuler took an active part in the patients’ examination and treatment. The development of the patients’ psychoses had been studied in retrospect from their beginnings to 1942–1943. A portion of the patients had been continuously hospitalized; a larger portion had been repeatedly or intermittently hospitalized. All patients were followed up until 1963–1965 or until their death. The course of their illness was usually described in the clinical charts with utmost accuracy, and corroborating data were gathered continuously during the whole study from a number of different sources. Inquiries concerning the patients’ illness course and development were made at least three times for every patient in the course of the 23 years of the study duration. For all patients, relatives or other informants were interviewed. The course of the illness could not be established for three of the 208 patients, as they died shortly after their illness had begun. Of the remaining 205, four had follow-up periods of less than 5 years and 201 had follow-ups of over 5 years. For 193 it was over 10 years, and for 175 it was over 20 years.
Regarding the typology of the long-term course of schizophrenia (Table 1), Bleuler differentiated between 1) a simple course without remissions—with acute onset (within a few days, a few weeks, or at the outside, a few months) or with chronic onset (almost unnoticed over many months or years) and 2) an undulating (episodic) course with identifiable separate illness periods of at least 1 week’s duration and times of remission. Also, he categorized outcome—defined as a constant condition maintained for over 5 years—into 1) recovery (with full employment, reassumed social roles, and no psychotic symptoms on examination except for some eccentricity or symptom residues) and 2) “end state,” which could be severe (with indifference to surroundings, practical incapability to communicate verbally, and requirement of constant care) or moderately severe/mild (less impaired but not recovered). All types of illness course (simple course with acute onset, simple course with chronic onset, and undulating course) could lead to a severe or moderately severe/mild end state; undulating course could also lead to recovery. The course could also be atypical, not conforming to the preceding types.
Diagnostic Reassessment
Both the clinical charts of the patients, containing detailed descriptions of psychopathological findings and their change during treatment, and the original research notes by Bleuler were available. The data on psychopathology were gathered from the clinical charts; the data on age at onset, duration of illness, and long-term course type were taken from the original research notes. For three of Bleuler’s original 208 patients (one man, two women) the clinical charts could not be located. The remaining 205 clinical charts were scrutinized independently by two psychiatrists (A.H. and E.S.) with regard to the psychopathology of the patients and fulfillment of the diagnostic criteria of the individual diagnostic systems. Before the study, both psychiatrists underwent diagnostic training for the various diagnostic systems. Bleuler’s original determination of the type of long-term course was respected; thus, the assessments of course and diagnosis occurred independently from each other.
Diagnostic Instruments
All patients were rediagnosed according to the sets of diagnostic criteria for schizophrenic disorder delineated by DSM-IV, DSM-III-R, ICD-10, and the Research Diagnostic Criteria (RDC) (7). Furthermore, the diagnostic criteria of Eugen Bleuler (6) and Schneider (8) were considered. Schneider offered the first operationalized schizophrenia definition; at least one of his eight schizophrenia-specific first-rank symptoms must be present to diagnose the disorder. Bleuler’s definition relies on the presence of his five basic symptoms (loosening of associations, autism, ambivalence, affective flattening, ego disturbances); we operationalized his definition by requiring the presence of at least two of them. ICD-10 relies heavily on Schneider’s criteria (three of four main diagnostic items refer to first-rank symptoms), whereas DSM-IV—even more than DSM-III-R—makes less effort to define a specific schizophrenia syndrome and enumerates nonspecific psychotic symptoms (bizarre delusions and commenting or conversing voices are mentioned only in a note). Furthermore, different systems require different minimum illness durations; the RDC ask for 2 weeks, ICD-10 for 4 weeks, and DSM-III-R and DSM-IV for 6 months (with or without prodrome). To the patients for whom the diagnosis of schizophrenia could not be confirmed by DSM-IV, DSM-III-R, or ICD-10, alternative diagnoses according to these individual diagnostic systems were given.
Reliability Control
In the course of the study, each clinical chart was evaluated and each patient was rediagnosed independently by both investigators. Afterward they compared their findings. Interrater agreement was achieved in 77% to 91% of the comparisons, depending on the diagnostic system. The kappa coefficients were between 0.41 and 0.63. Specifically, they were 0.63 for DSM-IV, 0.61 for DSM-III-R, ICD-10, and RDC, 0.41 for Bleuler’s criteria, and 0.46 for Schneider’s criteria. The low kappas for Bleuler’s diagnostic criteria were due to the small amount of variance in expected outcome (for 92% of the entire sample, Bleuler’s criteria were fulfilled). In case of diagnostic disagreement, a “best-estimate” consensus diagnosis was given. In all results the consensus diagnoses are included.
Statistical Evaluation
Chi-square analysis and Fisher’s exact test were used for categorical variables, and the Kruskal-Wallis test and t test were used for continuous variables. For reliability, Cohen’s kappa coefficients were calculated to test the agreement between raters and between diagnostic systems. Relative risks along with 95% confidence intervals (95% CIs) were computed for the individual types of course/onset and outcome separately for each diagnostic system.
Results
Rediagnosis
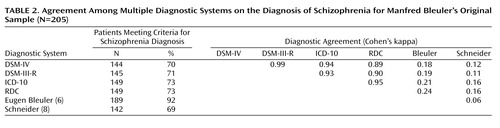
For 205 of 208 Bleuler’s original patients the diagnosis of schizophrenia could be tested. As Table 2 indicates, it was confirmed in 69% to 92% of the patients, depending on the diagnostic system. The proportion of male patients among those with confirmed schizophrenia was 46% to 48% for the different diagnostic systems, corresponding to the 48% in the original sample. The mean age at illness onset of the patients with a confirmed diagnosis of schizophrenia was 32 years (SD=11) in all diagnostic systems except for Bleuler’s, in which it was 31 years (SD=11). The 16 patients who did not fulfill Bleuler’s schizophrenia definition were significantly older at onset (mean=37 years, SD=12) (t=2.18, df=203, p=0.02), and the 63 patients not fulfilling Schneider’s diagnostic criteria were significantly younger (mean=29 years, SD=10) (t=1.83, df=203, p=0.04). Among patients with a confirmed diagnosis there was a significantly higher proportion of single patients (49% to 56%, depending on diagnostic system) than among patients without a confirmed diagnosis of schizophrenia (12% to 38%, depending on diagnostic system). The difference was statistically significant (p<0.01, chi-square analysis) for all diagnostic systems except Schneider’s criteria. For the latter, 49% of the patients were single among both the patients fulfilling and not fulfilling the schizophrenia definition.
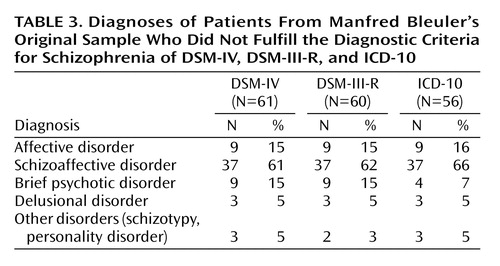
Table 3 shows the diagnostic distribution of patients who did not fulfill the diagnostic criteria for schizophrenia of DSM-IV, DSM-III-R, and ICD-10.
Illness Course
The course of illness could be assessed for 202 of the original 205 patients. Table 4 presents, for each diagnostic system, the distribution of patients with a confirmed schizophrenia diagnosis among the different types of illness course. In comparisons with the corresponding distribution in Bleuler’s original sample, no significant differences were found.
In Table 5 the distributions of patients are presented separately with regard to illness course/onset and end state of illness, after exclusion of the eight patients from the original sample who had shown atypical illness courses. Patients with a schizophrenia diagnosis confirmed by DSM-IV, DSM-III-R, ICD-10, and RDC had significantly higher risks for simple course with chronic onset and for severe end state and significantly lower probabilities of undulating course and of recovery than patients for whom the diagnosis of schizophrenic disorder was not confirmed. Also, there was a highly significant difference between patients with simple and undulating courses with regard to outcome: in Bleuler’s original sample, severe end state was identified in 26 (34%) of the patients with a simple course and 19 (16%) of those with an undulating course, moderate/mild end state in 50 (66%) and 55 (47%), respectively, and recovery in 0 (0%) versus 44 (37%) of the patients (χ2=38.02, df=2, p<0.0001).
There were no differences between the sexes in the distribution of the patients in the original sample by course/onset or end state. Patients with a simple course and chronic onset fell ill later, at a mean age of 35 years (SD=11), than patients with a simple course and acute onset, for whom the mean age was 31 years (SD=8), and patients with an undulating course, for whom the mean was 30 years (SD=11) (χ2=9.27, df=2, p=0.01). In contrast, there was no significant relationship between age at illness onset and outcome in terms of severe end state, moderate/mild end state, and recovery. The proportion of single patients was significantly higher among patients with simple course and acute onset (seven of eight, 88%) than among patients with chronic onset (28 of 68, 41%) or those with an undulating course (60 of 118, 51%) (χ2=6.57, df=2, p=0.04). Also, the proportion of single patients was significantly higher among those with a severe end state (27 of 45, 60%) than among the group with a moderate/mild end state (53 of 105, 50%) or the recovered group (15 of 44, 34%) (χ2=6.18, df=2, p=0.05).
The course of illness could be determined for all but two of the patients for whom the diagnosis of schizophrenia was not confirmed (one with affective disorder, one with schizoaffective disorder). All patients with brief psychotic disorder had an undulating course with recovery. Undulating course was also identified in seven of eight patients with affective disorder, about half of whom showed a recovery. In the large group of patients with schizoaffective disorder for whom course and outcome were known (N=35), the findings were identical with DSM-IV, DSM-III-R, and ICD-10: no patient had a simple course with acute onset, two patients had a simple course with chronic onset, and 33 had an undulating course; five had a severe end state, 16 had a moderate/mild end state, and 14 recovered. For DSM-IV, DSM-III-R, and ICD-10, there were significant differences between patients diagnosed with schizoaffective disorder and schizophrenia with regard to illness course (DSM-IV: χ2=22.97, df=2, p<0.0001; DSM-III-R: χ2=22.67, df=2, p<0.0001; ICD-10: χ2=21.53, df=2, p<0.0001) and outcome (DSM-IV: χ2=14.95, df=2, p=0.0006; DSM-III-R: χ2=15.10, df=2, p=0.0005; ICD-10: χ2=11.00, df=2, p=0.004).
Discussion
In this study we examined the course of illness in the patients in the schizophrenia study by Manfred Bleuler after we had rediagnosed the patients’ disorders by using both modern diagnostic criteria and those of Eugen Bleuler (the latter operationalized by us). Both the symptoms and the illness course—85% of all patients were followed up for more than 20 years—were well documented. Two investigators scrutinized the written material for each patient independently from each other, and they reached fair to good diagnostic agreement, with kappa coefficients between 0.41 and 0.63. Kappas over 0.60 were obtained for DSM-IV, DSM-III-R, ICD-10, and the RDC, confirming greater reliability of the modern diagnostic systems. Nevertheless, the highest kappa did not exceed 0.63; this was due to the format of our study, which was based on the retrospective evaluation of old clinical records (many of which were initiated in 1910–1920) and other written material and not on the live interviews. Besides, the descriptions were based on partially different psychopathological concepts. All this, however, had no bearing on the determination of course and outcome. In case of diagnostic disagreement, a best-estimate diagnosis was reached and agreed on by both investigators after a thorough discussion.
Depending on the diagnostic system, the diagnosis of schizophrenia was confirmed in 69% to 92% of all patients; the best result (92%) was reached by applying Eugen Bleuler’s criteria used by Manfred Bleuler to define this study sample. Manfred Bleuler was a highly experienced diagnostician, but the concepts of psychiatric disorders and the interpretation of similar symptoms change over time (9). Incidentally, the record information was rich, and it did not favor Bleuler’s criteria, so that we do not think there would be an information bias across the different diagnostic groupings. There was high diagnostic agreement, with kappas between 0.90 and 0.99 for agreement between the four main diagnostic systems (Table 2); these are in correspondence with levels of agreement in similar reports (10). In contrast, Bleuler’s and Schneider’s criteria had poor agreement with all other systems and with each other, reflecting the profound difference in the diagnostic approaches of those two systems. The lack of diagnostic agreement between ICD-10 and Schneider’s criteria is somewhat surprising, as some important ICD-10 schizophrenia items include these criteria.
Altogether, the diagnosis was not confirmed in approximately 30% of the original sample. Compared with study groups in older American studies (5, 11), this is a remarkably low figure, indicating Manfred Bleuler’s reserved attitude toward diagnosing schizophrenia. The majority of patients for whom the diagnosis of schizophrenia could not be confirmed received a diagnosis of schizoaffective disorder (Table 3)—a diagnosis hardly used by Bleuler, even though he admitted that in the course of typical schizophrenic illness, manic and depressive episodes can occur (12).
A minority of these patients received the diagnosis of affective disorder or brief psychotic reaction. Thus, on the whole, there was a certain shift from the schizophrenic to the affective spectrum, reflecting a contemporary diagnostic trend. For a long time cyclothymia was diagnosed only in cases where no schizophrenic symptoms could be verified, and this procedure resulted in widespread overdiagnosis of schizophrenia and underdiagnosis of affective disorders (13). Since the 1970s, diagnostic practice has taken an opposite course, in that schizophrenia is to be diagnosed only when an affective disorder can be excluded without doubt (14). In our study on clinical diagnoses, carried out in another Swiss psychiatric hospital, the same tendency to overdiagnose schizophrenia, to the disadvantage of affective disorders, and to value schizophrenic symptoms over affective symptoms was found (15). The greater appreciation of the importance of affective symptoms and the subsequent shift in diagnostic practice seem to be well justified by the evidence that has emerged from phenomenologic, prognostic, genetic, and possibly treatment-response studies (13). Along with other findings (16), the results of this study demonstrate a less malignant course and a better long-term outcome in schizoaffective than in schizophrenic disorder. Thus, they support the prognostic validity of the distinction of these two disorders. Another finding of the study is in agreement with this conclusion: the group of patients whose schizophrenia diagnosis was not confirmed contained a higher proportion of married or previously married patients, perhaps indicating a better capacity for intimate relationships. It is interesting that all three main contemporary diagnostic systems used in this study (DSM-IV, DSM-III-R, ICD-10) yielded practically identical results, with the exception of the smaller number of brief psychotic disorders diagnosed with ICD-10, reflecting the different requirements for duration of schizophrenic illness.
The course and the outcome of illness could be reviewed for 202 of the 205 patients in the original sample (Table 4). The majority of Bleuler’s original patients, 58%, presented an undulating illness course; 22% of the patients had a severe end state, and 22% recovered. Similar results have been reported elsewhere: continuous hospitalization for 19% and recovery for 19% were found in one study (17), and recovery and a functionally adequate outcome were reported for one-third of the patients in another study (18). The results indicate that in patients diagnosed with schizophrenia according to the criteria of DSM-IV, DSM-III-R, ICD-10, and RDC there is a slight shift in the distribution of the types of illness course; the proportion of patients with a simple (unremitting) course and chronic onset increased, whereas the proportion of patients with an undulating (episodic) course and recovery decreased. However, the distribution of patients among the eight types of illness course did not significantly differ between Bleuler’s original sample and the patients rediagnosed with the other diagnostic systems (Table 4).
On the other hand, in all groups whose schizophrenia diagnosis was confirmed by modern diagnostic systems (but not with Bleuler’s and Schneider’s criteria) the number of patients with an undulating course and the number who recovered were disproportionally lower and the numbers who had a simple course with chronic onset and who had a severe end state were disproportionally higher than in Bleuler’s original sample (Table 5). In contrast, undulating course was identified in over 80% of all patients for whom the diagnosis of schizophrenia was not confirmed, and only patients with an undulating course recovered. Also, few of these patients showed a simple course with chronic onset (about 10%); they fell ill earlier, and fewer were single. Incidentally, a lower proportion of single people was also found in the original sample in patients who had a simple course and chronic onset of disease; in this context, it is important that the age at illness onset for these patients was significantly higher. The latter is an unexpected finding that, however, should not be overvalued; age at illness onset was not associated with worse end state in spite of the high association between course and outcome. The appearance of Bleuler’s symptoms seems to characterize an earlier schizophrenia onset, and Schneider’s symptoms seem related to later onset.
In summary, it is fair to say that the modern diagnostic criteria for schizophrenia identify a more homogenous group of patients. Stricter operationalized diagnostic criteria for schizophrenic illness tend to identify a population of patients with a greater tendency toward chronicity and less frequent recovery. Nevertheless, as our data and those of Harding et al. (5) demonstrate, the more stringent criteria fail to produce a uniformly poor outcome: half of our patients with a confirmed schizophrenia diagnosis had an undulating illness course, and 12%–15% recovered (see Table 4). It is important to point out that the assessment of the final outcome required that the same condition be maintained over 5 years, a criterion also applied to other severe illnesses, such as cancer. A severe end state was reached by 27% to 28% of these patients. However, we must not forget that the study terminated in 1965, before the large-scale deinstitutionalization took place and before other modern therapeutic methods were introduced. Differences in therapeutic policies and programs contribute to differences in clinical outcome (19), which improved significantly in the course of the last century (20). Beyond that, for many patients the therapeutic response to neuroleptics would have been compromised by their long previous duration of illness.
In conclusion, we confirmed that in diagnosing the patients in his original sample, Manfred Bleuler relied heavily on the basic schizophrenic symptoms delineated by Eugen Bleuler. Compared with the main modern diagnostic systems (DSM-IV, DSM-III-R, ICD-10, RDC), Bleuler advocated a broader schizophrenia concept; for about 30% of his patients the diagnosis of schizophrenia could not be confirmed. Between the main diagnostic systems applied there was a high degree of diagnostic agreement; in contrast, Schneider’s and Bleuler’s criteria identified different patient groups.
In the majority of patients for whom a diagnosis of schizophrenia could not be confirmed, the diagnosis of schizoaffective disorder or brief psychotic reaction was given. The majority of these patients showed undulating illness course with recovery—a finding confirming the validity of the distinction of these disorders from schizophrenia.
A total of 58% of the patients of Bleuler’s original sample showed an undulating illness course; 22% developed severe end states, and 22% recovered. In the smaller group of all patients with a confirmed diagnosis of schizophrenia (atypical courses included), an undulating illness course was observed in about 48%–49% and the proportion of patients with severe end state increased to 27%–28%. Recovery occurred in 12%–15% of all patients; thus, even a patient diagnosed with schizophrenic illness according to DSM-IV or ICD-10 has a chance to recover.
On the whole, the prognosis of the patients with a diagnosis of schizophrenia according to modern criteria appears worse; nevertheless, half of them still show an undulating illness course, and some 25%–30% of the latter recover.
The high proportion, 27%–28%, of patients with severe end state in the group with confirmed schizophrenia must be seen against the background of the therapeutic possibilities available in the 1940s to 1960s.
 |
 |
 |
 |
 |
Received Oct. 9, 2002; revision received April 8, 2003; accepted June 20, 2003. From the Psychiatric Hospital, University of Zurich. Address reprint requests to Dr. Modestin, Psychiatric Hospital, University of Zurich, Lenggstrasse 31, CH-8029 Zurich, Switzerland; [email protected] (e-mail). The authors thank Prof. D. Umbricht for his comments.
1. Bleuler M: The Schizophrenic Disorders: Long-Term Patient and Family Studies (1972). London, Yale University Press, 1978Google Scholar
2. Ciompi L, Müller C: Lebensweg und Alter der Schizophrenen, eine katamnestische Langzeitstudie bis ins Senium. Berlin, Springer, 1976Google Scholar
3. Huber G, Gross G, Schüttler R: Schizophrenie: Eine verlaufs- und sozialpsychiatrische Langzeitstudie. Berlin, Springer, 1978Google Scholar
4. Harding CM, Brooks GW, Ashikaga T, Strauss JS, Breier A: The Vermont longitudinal study of persons with severe mental illness, I: methodology, study sample, and overall status 32 years later. Am J Psychiatry 1987; 144:718–726Link, Google Scholar
5. Harding CM, Brooks GW, Ashikaga T, Strauss JS, Breier A: The Vermont longitudinal study of persons with severe mental illness, II: long-term outcome of subjects who retrospectively met DSM-III criteria for schizophrenia. Am J Psychiatry 1987; 144:727–735Link, Google Scholar
6. Bleuler E: Dementia praecox oder Gruppe der Schizophrenien. Leipzig, Germany, Deuticke, 1911Google Scholar
7. Spitzer RL, Endicott J, Robins E: Research Diagnostic Criteria (RDC) for a Selected Group of Functional Disorders, 3rd ed. New York, New York State Psychiatric Institute, Biometrics Research, 1977Google Scholar
8. Schneider K: Klinische Psychopathologie, 7 Auflage. Stuttgart, Germany, Thieme, 1966Google Scholar
9. Blum DJ: On changes in psychiatric diagnosis over time. Am Psychol 1978; 33:1017–1031Crossref, Medline, Google Scholar
10. Gruenberg AM, Kendler KS, Tsuang MT: Reliability and concordance in the subtyping of schizophrenia. Am J Psychiatry 1985; 142:1355–1358Link, Google Scholar
11. Morrison J, Clancy J, Crowe R, Winokur G: The Iowa 500, I: diagnostic validity in mania, depression, and schizophrenia. Arch Gen Psychiatry 1972; 27:457–461Crossref, Medline, Google Scholar
12. Bleuler E: Lehrbuch der Psychiatrie, 11 Auflage; umgearbeitet von M Bleuler. Berlin, Springer, 1969Google Scholar
13. Pope HG Jr, Lipinski JF Jr: Diagnosis in schizophrenia and manic-depressive illness: a reassessment of the specificity of “schizophrenic” symptoms in the light of current research. Arch Gen Psychiatry 1978; 35:811–828Crossref, Medline, Google Scholar
14. Berner P: Modifications in the psychopathologic definition of schizophrenia—alterations during the last two decades: expectations for the future. Compr Psychiatry 1980; 21:475–482Crossref, Medline, Google Scholar
15. Modestin J: Clinical diagnostic practice reviewed: a comparison of clinical and RDC diagnoses. Psychopathology 1984; 17:80–89Crossref, Medline, Google Scholar
16. Harrow M, Grossman LS, Herbener ES, Davies EW: Ten-year outcome: patients with schizoaffective disorders, schizophrenia, affective disorders and mood-incongruent psychotic symptoms. Br J Psychiatry 2000; 177:421–426Crossref, Medline, Google Scholar
17. Morrison J, Winokur G, Crowe R, Clancy J: The Iowa 500: the first follow-up. Arch Gen Psychiatry 1973; 29:678–682Crossref, Medline, Google Scholar
18. McGlashan TH: The Chestnut Lodge follow-up study, II: long-term outcome of schizophrenia and the affective disorders. Arch Gen Psychiatry 1984; 41:586–601Crossref, Medline, Google Scholar
19. DeSisto M, Harding CM, McCormick RV, Ashikaga T, Brooks GW: The Maine and Vermont three-decade studies of serious mental illness, II: longitudinal course comparisons. Br J Psychiatry 1995; 167:338–342Crossref, Medline, Google Scholar
20. Hegarty JD, Baldessarini RJ, Tohen M, Waternaux C, Oepen G: One hundred years of schizophrenia: a meta-analysis of the outcome literature. Am J Psychiatry 1994; 151:1409–1416Link, Google Scholar



