Testosterone Gel Supplementation for Men With Refractory Depression: A Randomized, Placebo-Controlled Trial
Abstract
OBJECTIVE: Testosterone supplementation may produce antidepressant effects in men, but until recently it has required cumbersome parenteral administration. In an 8-week randomized, placebo-controlled trial, the authors administered a testosterone transdermal gel to men aged 30–65 who had refractory depression and low or borderline testosterone levels. METHOD: Of 56 men screened, 24 (42.9%) displayed morning serum total testosterone levels of 350 ng/dl or less (normal range=270–1070). Of these men, 23 entered the study. One responded to an initial 1-week single-blind placebo period, and 22 were subsequently randomly assigned: 12 to 1% testosterone gel, 10 g/day, and 10 to identical-appearing placebo. Each subject continued his existing antidepressant regimen. Ten subjects receiving testosterone and nine receiving placebo completed the 8-week trial. RESULTS: The groups were closely matched on baseline demographic and psychiatric measures. Subjects receiving testosterone gel had significantly greater improvement in scores on the Hamilton Depression Rating Scale than subjects receiving placebo. These changes were noted on both the vegetative and affective subscales of the Hamilton Depression Rating Scale. A significant difference was also found on the Clinical Global Impression severity scale but not the Beck Depression Inventory. One subject assigned to testosterone reported increased difficulty with urination, suggesting an exacerbation of benign prostatic hyperplasia; no other subject reported adverse events apparently attributable to testosterone. CONCLUSIONS: These preliminary findings suggest that testosterone gel may produce antidepressant effects in the large and probably underrecognized population of depressed men with low testosterone levels.
Several lines of evidence suggest that testosterone and other androgens might be effective in the treatment of major depressive disorder in certain men. First, depressed men in some studies (1, 2) exhibited low plasma or serum testosterone levels, although this association is inconsistent and probably influenced by additional factors (3–5). Second, hypogonadal men often exhibit depressive symptoms, and testosterone replacement may improve these symptoms (6, 7). This finding extends to men with HIV-induced hypogonadism (8, 9). Third, anabolic steroid abusers, who ingest markedly supraphysiologic doses of testosterone and related androgens, sometimes develop manic or hypomanic symptoms during androgen use and depressive symptoms during androgen withdrawal (10).
Fourth, uncontrolled studies of depressed men in the 1940s and 1950s (10, 11), together with a few controlled studies in the 1970s and 1980s (12, 13), have suggested that testosterone and other androgens might have antidepressant properties. Two more recent studies have produced somewhat contradictory results in this area. In the first, Seidman and Rabkin (14) added open-label intramuscular testosterone enanthate, 400 mg every 2 weeks, to the existing antidepressant regimens of five men with refractory depression and low or borderline plasma total testosterone levels (200–350 ng/dl; reference range=300–990 ng/dl). These men’s mean score on the Hamilton Depression Rating Scale declined significantly over 8 weeks. Subsequently, Seidman et al. (15) conducted a randomized, placebo-controlled trial of testosterone enanthate for 30 men with major depressive disorder and testosterone levels of 350 ng/dl or less. Unlike the men in the previous open-label study, however, these subjects were not simultaneously taking antidepressants. After 6 weeks of treatment, the investigators found no significant difference between testosterone and placebo in scores on the Hamilton Depression Rating Scale or Beck Depression Inventory.
The preceding lines of evidence, although inconsistent, suggest that testosterone might benefit at least some depressed men—perhaps especially those with low plasma testosterone levels—although these antidepressant effects are likely variable and idiosyncratic (15). However, given the prevalence of treatment-resistant depression (16), further investigation of testosterone’s possible antidepressant effects seems warranted.
Another stimulus for further investigation has been the introduction of new modes of administration for testosterone, such as patch (17, 18) and gel (19) preparations, which offer alternatives to intramuscular injections of testosterone and to potentially hepatotoxic orally active synthetic androgens (20). We took advantage of one of these products, a transdermal 1% testosterone gel, to conduct a placebo-controlled, double-blind study of testosterone supplementation for men with refractory depression and low or borderline testosterone levels.
Method
Subjects
We recruited men meeting the following inclusion criteria: 1) age between 30 and 65 years, 2) current treatment with an adequate dose of antidepressant medication (as defined by the manufacturer’s published product information) for at least 4 weeks, 3) symptoms still meeting the DSM-IV criteria for current major depressive disorder, 4) a low or borderline morning serum total testosterone level (100–350 ng/dl; normal range in our laboratory, 270–1070 ng/dl), and 5) a normal prostate-specific antigen (PSA) level (<1.5 ng/ml in men aged 30–39, <2.5 ng/ml in men 40–49, <3.5 ng/ml in men 50–59, and <4.0 ng/ml in men 60–64).
Potential subjects, recruited through radio advertisements and referrals, were seen at the Biological Psychiatry Laboratory at McLean Hospital for an initial screening visit, scheduled before 10:00 a.m., when testosterone levels would normally be at their diurnal maximum (21). After complete description of the study to the subjects, written informed consent was obtained. The subjects were then assessed with the depression module of the Structured Clinical Interview for DSM-IV (SCID) (22) to confirm the diagnosis of current major depressive disorder. Subjects who did not meet the criteria for current major depressive disorder or who reported active suicidal ideation were excluded from the study. We next administered the American Urological Association Symptom Index for benign prostatic hyperplasia (23), in which a score of 0–7 is defined as “mild,” 8–19 as “moderate,” and 20–35 as “severe.” Subjects scoring higher than 14 on this index were excluded. Blood was then collected for measurement of total testosterone and PSA levels.
Men displaying low testosterone and normal PSA levels according to our laboratory criteria were invited to return for a second screening evaluation. The assessments at this visit included 1) basic demographic questions, 2) the remainder of the SCID, 3) questions regarding history of previous antidepressant drug treatment, 4) the Hamilton Depression Rating Scale, 5) the Beck Depression Inventory, 6) the Clinical Global Impression, 7) a medical history, 8) a physical examination, including measurement of vital signs, calculation of body mass index, and digital rectal examination of the prostate, 9) collection of blood and urine samples for urinalysis, standard chemistries, blood cell counts, and HIV serology measurements, 10) ECG, and 11) determination of body fat with calipers, together with calculated fat-free mass index, a measure of muscularity previously developed in our laboratory (24). Subjects were excluded if they exhibited 1) any substance use disorder within the past year (or illicit anabolic steroid use at any time in their lives), 2) current or past psychotic symptoms, 3) a history of bipolar I or bipolar II disorder, 4) any abnormality during the digital rectal examination, or 5) evidence of other clinically significant medical disease. The qualifying subjects then began 1 week of single-blind administration of placebo gel. All subjects continued taking their existing antidepressant medications, together with any other prescribed medications, at their present doses throughout the study.
Week 0 (Baseline)
After the single-blind placebo period, the subjects returned for a baseline visit, during which they were assessed for scores on the Hamilton Depression Rating Scale, Beck Depression Inventory, and Clinical Global Impression measure of severity of illness; for adverse events; and for vital signs. Results from the ECGs and the laboratory tests for which blood was drawn at screening were also reviewed. Subjects were withdrawn from the study at this point if they 1) displayed more than 50% improvement on the Hamilton Depression Rating Scale or Beck Depression Inventory after the placebo treatment or 2) were found to have a clinically significant abnormality on the laboratory tests or ECG. The subjects who qualified to continue in the study were then randomly assigned to receive either 10 g of 1% testosterone gel or placebo gel daily for the next 7 days. Drug and placebo were supplied in identical-appearing packets containing either 2.5 g of testosterone gel or a placebo gel, so that the starting dose was four packets per day.
Randomization and Blinding
An independent research assistant, not otherwise involved in the study, placed testosterone and placebo gel packets in numbered containers, using a randomization schedule that was not “blocked” or stratified. Thus, each subject had a 50% chance of receiving either treatment, determined independently of the treatment assignment of all other subjects. At baseline, the principal investigator (H.G.P.) assigned sequential numbers to the subjects as they were randomly assigned and supplied study medication to them from the corresponding numbered containers. Each subject and all study investigators (except for the unblinded dose adjuster; see following section) remained blinded to that subject’s treatment assignment until all of his ratings were completed at study termination.
Week 1
At week 1, the subjects were again assessed for scores on the Hamilton Depression Rating Scale, Beck Depression Inventory, and Clinical Global Impression (both severity of illness and improvement from baseline); for adverse events; and for vital signs. In addition, the subjects provided blood for determination of total testosterone level; the blood sample was drawn at least 4 hours after the morning application of the gel. This level was communicated to a separate unblinded investigator (J.I.H.), who ordered a reduced dose of gel (7.5 g, or three packets) for any subject exceeding the normal range (>1070 ng/dl). This investigator also performed sham dose adjustments for the placebo-treated patients to ensure that the subjects and investigators remained blinded. The unblinded dose adjuster was permitted only to lower, not to raise, the dose of study drug. Throughout the study he had no contact with any of the subjects and no discussions with the other investigators regarding the subjects.
Weeks 2, 4, 6, and 8
The subjects were seen at each of these time points for assessment with the Hamilton Depression Rating Scale, Beck Depression Inventory, and Clinical Global Impression; for determination of adverse events; and for measurement of vital signs. At week 8, the subjects also received an additional determination of PSA level and measurement of weight and body fat. When these assessments were completed, the blind was then broken and the treatment assignment determined. Since randomization was performed without blocking or stratification, as already mentioned, this unblinding gave the investigators no information regarding the treatment assignment of subsequent subjects still undergoing blinded treatment. Subjects who had received testosterone and who felt that they had responded were referred to their original physicians for consideration of continued testosterone treatment. Subjects who had received placebo were offered up to 4 weeks of treatment with testosterone gel by the investigators, followed by referral to their original physicians.
Subjects were withdrawn before the 8-week point if they 1) voluntarily elected to withdraw for any reason, 2) displayed an adverse event judged clinically significant by the investigators, or 3) failed to comply with the requirements of the protocol.
Objectives, Outcomes, and Group Size
We hypothesized that testosterone supplementation would be more effective than placebo in reducing depression, as assessed by improvement in scores on the Hamilton Depression Rating Scale, Beck Depression Inventory, and Clinical Global Impression. We also hypothesized that the subjects receiving testosterone gel would exhibit greater reductions in body fat and increases in muscle mass than the subjects receiving placebo. The study was planned to be exploratory and to guide future studies by providing an estimate of the magnitude and standard deviation of the changes in outcome measures for each group. We chose a group size of 22 for this purpose, recognizing that this small study group would limit our power to detect significant differences between groups in outcome measures.
Statistical Analysis
The baseline characteristics of the two groups were compared by using Fisher’s exact test for categorical variables and the t test for continuous variables. Outcomes were assessed in both an intent-to-treat group of patients, including those with at least one available score on the efficacy measures, and a completers group, defined as patients who completed the 8-week treatment period.
The primary protocol-defined analysis of efficacy was a repeated measures random regression analysis comparing the two groups’ rates of change in scores on the Hamilton Depression Rating Scale, Beck Depression Inventory, and Clinical Global Impression severity measure during treatment, conducted according to methods previously described (25, 26). Our model for the mean value for each outcome measure included terms for treatment, time, and treatment-by-time interaction. We modeled time as a continuous variable, with weeks ranging from 0 to 8. The measure of effect was the treatment-by-time interaction, which can be interpreted as the difference in slope, or rate of change per unit of time, of the efficacy measure. To account for the correlation of observations within individuals, we calculated the standard errors of the parameter estimates using generalized estimating equations, with compound symmetry as the working covariance structure, as implemented by the PROC GENMOD command in SAS software (Cary, N.C., SAS Institute).
In the secondary intent-to-treat analysis, we used the last observation carried forward for all subjects completing at least one postbaseline assessment and conducted t tests to compare the groups on change from baseline to endpoint in scores on the Hamilton Depression Rating Scale, Beck Depression Inventory, and Clinical Global Impression severity scale.
For laboratory measures, including body fat and fat-free mass index, we computed the mean difference between the endpoint and baseline measurements, and we then compared the treatment groups using t tests. We calculated correlation coefficients by using rank-transformed data (Spearman rank correlation). All statistical tests were two-sided with alpha=0.05.
Results
Recruitment and Participant Flow
We screened 56 men between September and December 2001. The mean age of these men was 46.9 years (SD=9.2, range=30–65). All of the 56 subjects met our criteria for PSA level, benign prostatic hyperplasia, and persistent major depressive disorder despite current antidepressant treatment. Their mean serum total testosterone level, 403 ng/dl (SD=152), was remarkably low for their age range (1, 27). Testosterone level was inversely, but not quite significantly, correlated with age (rs=–0.25, N=56, p=0.06). Thirty-two subjects had testosterone levels above 350 ng/dl and were excluded. Twenty-four (42.9%) of the subjects had levels of 350 ng/dl or below; one of these men had a value of only 84 ng/dl—below the limit of our inclusion criteria—and was referred for endocrinological evaluation. The remaining 23 qualifying subjects all agreed to participate in the study. During the single-blind placebo period, one subject improved by 61% on the Beck Depression Inventory and thus was withdrawn before randomization. The remaining 22 subjects were randomly assigned at week 0. Of these, three (13.6%) withdrew during the trial: one failed to return for any postrandomization visits, citing “scheduling problems,” and another withdrew at week 4 for lack of improvement and increased nocturia; both of these men had been randomly assigned to testosterone. A third man was withdrawn by the investigators at week 4 for worsening depression and suicidal ideation; he had been assigned to placebo. The remaining 19 men (86.4%) completed the full 8-week study, 10 receiving testosterone and nine receiving placebo.
Baseline Characteristics of Subjects
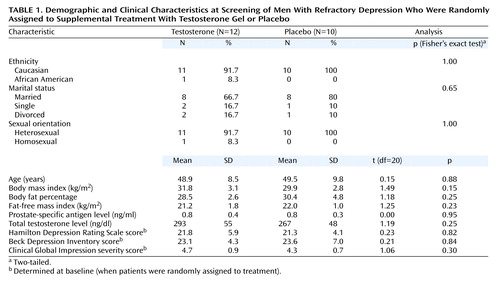
The 12 subjects randomly assigned to testosterone did not differ significantly from the 10 assigned to placebo in terms of their attributes at screening (Table 1). The antidepressant medications and daily doses for the subjects receiving testosterone were paroxetine, 20–40 mg (N=3); citalopram, 20 mg (N=2); bupropion, 300–450 mg (N=2); venlafaxine, 150–225 mg (N=3); nefazodone, 400 mg (N=1); and methylphenidate, 54 mg (N=1). The subjects assigned to placebo were taking paroxetine, 20–40 mg (N=3); citalopram, 30–40 mg (N=2); fluoxetine, 60 mg (N=1); sertraline, 100 mg (N=1); venlafaxine, 200 mg (N=1); and citalopram, 20–40 mg, plus bupropion, 300–400 mg (N=2). All subjects had been taking their medications for at least 8 weeks at the time of random assignment, with the exception of one subject assigned to testosterone, who had been taking paroxetine, 20 mg, for 5 weeks. However, this man had not responded to previous trials of paroxetine, fluoxetine, and venlafaxine that had each lasted more than 8 weeks.
Efficacy Analyses
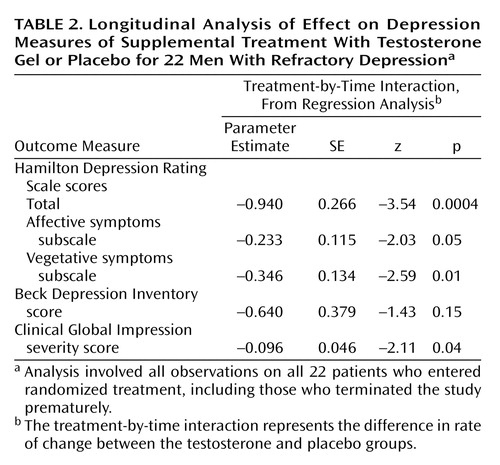
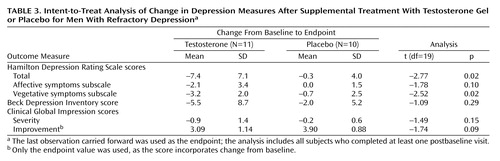
The primary analysis of efficacy, involving all 22 subjects who entered randomized treatment, revealed that the testosterone-treated patients had a significantly greater rate of decrease in scores on the Hamilton Depression Rating Scale than the placebo-treated patients (Figure 1, top), as indicated by the treatment-by-time interaction Table 1). This improvement was evident on both the vegetative and affective symptoms subscales of the Hamilton Depression Rating Scale (Table 2). Testosterone was also associated with a significantly greater rate of decrease in the Clinical Global Impression severity scores although not the Beck Depression Inventory scores (Figure 1, Table 2). The weaker results on the Beck Depression Inventory appeared attributable to the greater variability of scores on this instrument, together with the fact that two placebo subjects had substantial improvements in their scores on the Beck Depression Inventory, although not on the Hamilton Depression Rating Scale. The intent-to-treat endpoint analysis produced similar results but with higher p values, consistent with less statistical power than the longitudinal analysis (Table 3). Among the study completers, there were no significant differences between the subjects receiving testosterone and those receiving placebo in change in percentage of body fat (mean=–2.8%, SD=1.7%, versus mean=–1.9%, SD=2.6%) (t=0.90, df=17, p=0.38) or change in muscle mass as expressed by the fat-free mass index (mean=1.1 kg/m2, SD=0.9, versus mean=0.6 kg/m2, SD=1.2) (t=1.03, df=17, p=0.32).
Among the 21 men who returned at week 1, the mean serum total testosterone levels were 789 ng/dl (SD=519) in the testosterone group and 249 ng/dl (SD=68) in the placebo group (t=3.26, df=19, p=0.004). Notably, three of the 11 testosterone subjects displayed increases of 70 ng/dl or less in their total testosterone levels with the gel; unfortunately, the unblinded dose adjuster was not allowed to increase the dose of gel for these subjects, since our protocol had not anticipated this possibility. Perhaps not surprisingly, these three subjects also displayed little improvement in depressive symptoms (changes of 0, 0, and 1, respectively, on the Clinical Global Impression severity rating at termination). The remaining eight subjects all achieved increases greater than 200 ng/dl in testosterone levels at week 1; four (50.0%) of these subjects improved by 2 or more points on Clinical Global Impression severity, as compared to none of the 10 subjects receiving placebo (p=0.03 by Fisher’s exact test, two-tailed). Among the eight testosterone subjects with increases of more than 200 ng/dl, three had improvements of more than 50% on the Hamilton Depression Rating Scale, and three others had improvements of 36%–43%. No placebo subject had an improvement of more than 30% on the Hamilton Depression Rating Scale.
Adverse Events
One subject receiving testosterone reported increased nocturia and difficulty initiating urination, suggesting a possible exacerbation of benign prostatic hyperplasia. These symptoms, coupled with lack of improvement in depression, prompted him to withdraw after week 4. His urinary symptoms remitted within 3 weeks after withdrawal. No other subject reported adverse effects apparently attributable to testosterone during the study. Among the study completers, the change in PSA level from screening to week 8 did not differ significantly between the testosterone group (mean=0.11 ng/ml, SD=0.23) and the placebo group (mean=0.00 ng/ml, SD=0.30) (t=0.90, df=17, p=0.38).
Discussion
We conducted an 8-week randomized, placebo-controlled trial of testosterone transdermal gel with 22 men who had treatment-resistant depression and low or borderline serum total testosterone levels (≤350 ng/dl). Testosterone gel, added to the subjects’ existing antidepressant regimens, proved significantly superior to placebo in reducing scores on the Hamilton Depression Rating Scale and the Clinical Global Impression severity scale, although not on the Beck Depression Inventory. These findings suggest that testosterone supplementation may produce antidepressant effects in some men with treatment-resistant depression.
Two observations in the study deserve particular comment. First, the men in our study, with a mean age of only 46.9 years, displayed a mean total testosterone level of only 403 ng/dl (SD=152)—strikingly lower than the mean of 605 ng/dl (SD=212) among men aged 45–54 in a typical study of the general population (27), and even slightly below the mean of 429 (SD=124) in a recent study (4) of men with major depressive disorder in their 60s and 70s, when testosterone would normally be much lower than in middle age. These observations suggest that low testosterone levels may be unexpectedly common in middle-aged men with treatment-resistant major depressive disorder, perhaps because chronic depressive symptoms lead to blunting of the hypothalamic-pituitary-gonadal axis (4) or, possibly, because of effects of the antidepressant medications themselves.
Second, testosterone gel appeared to benefit psychological aspects of depression (represented by the depressed mood, guilt, and psychological anxiety items of the Hamilton Depression Rating Scale) to nearly the same degree as the somatic aspects of depression (represented by the Hamilton scale items involving sleep, appetite, libido, and somatic symptoms). This finding differs somewhat from that of a previous study of testosterone for HIV-infected men (8), who experienced substantially greater improvement in vegetative than in affective symptoms—raising the important question of whether testosterone benefited their depression only because of its effects on somatic symptoms such as fatigue and libido (28). One reason for this difference in findings may be that HIV-infected men have higher initial levels of somatic symptoms, such as anorexia, weight loss, and fatigue, than did our study group of medically healthy depressed men.
The mechanism of testosterone’s antidepressant effects, and the variability of these effects among subjects, remains speculative. Testosterone modulates brain monoamine levels, as evidenced by one study (29) that showed lowered CSF 3-methoxy-4-hydroxyphenylglycol and elevated 5-hydroxyindoleacetic acid (5-HIAA) levels in normal volunteers after methyltestosterone administration. Notably, CSF 5-HIAA changes were positively correlated with activation scores in this study, suggesting that the psychiatric effects of testosterone might be mediated through serotonergic function. The inconsistent relationship between endogenous plasma testosterone levels and depression, and the inconsistent antidepressant effects of exogenous testosterone, may be attributable to the weak association between plasma and CSF testosterone levels. For instance, in one recent study (30), patients with posttraumatic stress disorder had low CSF testosterone levels but normal plasma testosterone levels, and there was no significant association between plasma and CSF testosterone levels.
Several limitations of our study must be considered. First, the small number of subjects limits statistical power. Second, the study assessed the effects of testosterone for only 8 weeks and does not permit conclusions about long-term efficacy or safety for depressed men. Third, the blind was broken for each subject individually at termination, rather than for all subjects at the conclusion of the study, as is more conventional. However, since randomization was performed without blocking or stratification, investigator bias due to unblinding should be largely eliminated, as we have already explained. Fourth, the study used a single serum total testosterone level to determine eligibility. More sophisticated laboratory screening (including measurements of free testosterone, sex hormone-binding globulin, and pituitary gonadotropins, together with serial chemistry and hematology measurements) might help to identify candidates for treatment, laboratory predictors of treatment response, and potential adverse effects. Fifth, testosterone was added to existing antidepressant treatment for men who were not responding to antidepressants. It is unclear whether testosterone would prove equally effective for depressed men not currently taking antidepressants. The findings of Seidman and colleagues (14, 15), summarized earlier in this article, combined with the results of the present study, suggest that testosterone might be more useful as a supplement to conventional antidepressant treatment than as an antidepressant by itself. Sixth, our study was limited to men because of the masculinizing effects of testosterone. However, preliminary data (31) suggest that in much lower doses, testosterone may exhibit antidepressant effects in women as well; this possibility deserves exploration.
The benefits of testosterone supplementation must also be weighed against potential risks. For example, in one early paper (32) it was reported that of five men receiving imipramine for depression, four developed paranoid symptoms when the synthetic androgen methyltestosterone was added to their regimen. In our study, by contrast, no subject assigned to testosterone was rated on any study visit as having “ideas of reference” or “delusions of reference and persecution” on the “paranoid symptoms” item of the Hamilton Depression Rating Scale. However, none of our subjects was receiving a tricyclic antidepressant.
Our brief study also did not permit assessment of possible longer-term risks of testosterone administration, such as gynecomastia, adverse effects on lipid fractions, or gradual exacerbation of benign prostatic hyperplasia (33). Long-term exogenous testosterone administration also suppresses the hypothalamic-pituitary-testicular axis, with consequent oligospermia and the risk of severe temporary suppression of gonadal function if testosterone is abruptly withdrawn (33). Finally, there remains the question of whether long-term testosterone supplementation might increase the risk of prostate or other cancers. The present data on this issue are still inadequate (28, 33, 34).
In conclusion, these findings may have important consequences for public health. In a given year, about 8% of American men over the age of 30 years exhibit major depressive disorder (35), and many of these cases will be partially or completely refractory to an adequate trial of antidepressant medication (16). If this subgroup with refractory depression has a 43% prevalence of low testosterone levels, as found in the present study, then hundreds of thousands of men in a given year might at least theoretically be candidates for testosterone supplementation to treat depression. Given the size of this population, together with the increased availability and convenience of transdermal testosterone preparations, it seems important to assess carefully both the benefits and the risks of this antidepressant treatment strategy.
 |
 |
 |
Received March 18, 2002; revision received July 24, 2002; accepted Aug. 17, 2002. From the Biological Psychiatry Laboratory, McLean Hospital; the Department of Psychiatry, Harvard Medical School, Boston; and the Departments of Biostatistics and Epidemiology, Harvard School of Public Health, Boston. Address reprint requests to Dr. Pope, Biological Psychiatry Laboratory, McLean Hospital, 115 Mill St., Belmont, MA 02478-9106; [email protected] (e-mail). Supported in part by a grant from Unimed Pharmaceuticals Corporation.
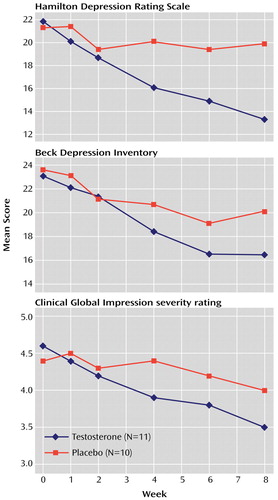
Figure 1. Scores on Depression Measures Over 8 Weeks of Supplemental Treatment With Testosterone Gel or Placebo for Men With Refractory Depression
1. Barrett-Connor E, von Mühlen DG, Kritz-Silverstein D: Bioavailable testosterone and depressed mood in older men: the Rancho Bernardo study. J Clin Endocrinol Metab 1999; 84:573-577Crossref, Medline, Google Scholar
2. Schweiger U, Deuschle M, Weber B, Körner A, Lammers C-H, Schmider J, Gotthardt U, Heuser I: Testosterone, gonadotropin, and cortisol secretion in male patients with major depression. Psychosom Med 1999; 61:292-296Crossref, Medline, Google Scholar
3. Levitt AJ, Joffe RT: Total and free testosterone in depressed men. Acta Psychiatr Scand 1988; 77:346-348Crossref, Medline, Google Scholar
4. Seidman SN, Araujo AB, Roose SP, Devanand DP, Xie S, Cooper TB, McKinlay JB: Low testosterone levels in elderly men with dysthymic disorder. Am J Psychiatry 2002; 159:456-459Link, Google Scholar
5. Booth A, Johnson DR, Granger DA: Testosterone and men’s depression: the role of social behavior. J Health Soc Behav 1999; 40:130-140Crossref, Medline, Google Scholar
6. Burris AS, Banks SM, Carter CS, Davidson JM, Sherins RJ: A long-term, prospective study of the physiologic and behavioral effects of hormone replacement in untreated hypogonadal men. J Androl 1992; 13:297-304Medline, Google Scholar
7. Wang C, Alexander G, Berman N, Salehian B, Davidson T, McDonald V, Steiner B, Hull L, Callegari C, Swerdloff RS: Testosterone replacement therapy improves mood in hypogonadal men—a clinical research center study. J Clin Endocrinol Metab 1996; 81:3578-3583Medline, Google Scholar
8. Rabkin JG, Wagner GJ, Rabkin R: A double-blind, placebo-controlled trial of testosterone therapy for HIV-positive men with hypogonadal symptoms. Arch Gen Psychiatry 2000; 57:141-147Crossref, Medline, Google Scholar
9. Grinspoon S, Corcoran C, Stanley T, Baaj A, Basgoz N, Klibanski A: Effects of hypogonadism and testosterone administration on depression indices in HIV-infected men. J Clin Endocrinol Metab 2000; 85:60-65Medline, Google Scholar
10. Pope HG Jr, Katz DL: Psychiatric effects of exogenous anabolic-androgenic steroids, in Psychoneuroendocrinology for the Clinician. Edited by Wolkowitz OM, Rothschild AJ. Washington, DC, American Psychiatric Press (in press)Google Scholar
11. Altschule MD, Tillotson KJ: The use of testosterone in the treatment of depressions. N Engl J Med 1948; 239:1036-1038Crossref, Medline, Google Scholar
12. Itil TM, Michael ST, Shapiro DM, Itil KZ: The effects of mesterolone, a male sex hormone in depressed patients (a double-blind controlled study). Methods Find Exp Clin Pharmacol 1984; 6:331-337Medline, Google Scholar
13. Vogel W, Klaiber EL, Braverman DM: A comparison of the antidepressant effect of a synthetic androgen (mesterolone) and amitriptyline in depressed men. J Clin Psychiatry 1985; 46:6-8Medline, Google Scholar
14. Seidman SN, Rabkin J: Testosterone replacement therapy for hypogonadal men with SSRI-refractory depression. J Affect Disord 1998; 48:157-161Crossref, Medline, Google Scholar
15. Seidman SN, Spatz E, Rizzo C, Roose SP: Testosterone replacement therapy for hypogonadal men with major depressive disorder: a randomized, placebo-controlled trial. J Clin Psychiatry 2001; 62:406-412Crossref, Medline, Google Scholar
16. Depression Guideline Panel: Depression in Primary Care, vol 2: Treatment of Major Depression: Clinical Practice Guideline 5: AHCPR Publication 93-0551. Rockville, Md, US Department of Health and Human Services, 1993Google Scholar
17. Cunningham GR, Cordero E, Thornby JI: Testosterone replacement with transdermal therapeutic systems: physiological serum testosterone levels and elevated dihydrotestosterone levels. JAMA 1989; 261:2525-2530Crossref, Medline, Google Scholar
18. Dobs AS, Meikle AW, Arver S, Sanders SW, Caramelli AE, Mazer NA: Pharmacokinetics, efficacy, and safety of a permeation-enhanced testosterone transdermal system in comparison with bi-weekly injections of testosterone enanthate for the treatment of hypogonadal men. J Clin Endocrinol Metab 1999; 84:3469-3478Medline, Google Scholar
19. Wang C, Swerdloff RS, Iranmanesh A, Dobs A, Snyder PJ, Cunningham G, Matsumoto AM, Weber T, Berman N: Transdermal testosterone gel improves sexual function, mood, muscle strength, and body composition parameters in hypogonadal men. J Clin Endocrinol Metab 2000; 85:2839-2853Medline, Google Scholar
20. Haupt HA, Rovere GD: Anabolic steroids: a review of the literature. Am J Sports Med 1984; 12:469-484Crossref, Medline, Google Scholar
21. Winters SJ: Diurnal rhythm of testosterone and luteinizing hormone in hypogonadal men. J Androl 1991; 12:185-190Medline, Google Scholar
22. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders (SCID). New York, New York State Psychiatric Institute, Biometrics Research, 1996Google Scholar
23. Barry MJ, Fowler FJ Jr, O’Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, Cockett AT (Measurement Committee of the American Urological Association): The American Urological Association symptom index for benign prostatic hyperplasia. J Urol 1992; 148:1549-1557Crossref, Medline, Google Scholar
24. Kouri EM, Pope HG Jr, Katz DL, Oliva PS: Fat-free mass index in users and nonusers of anabolic-androgenic steroids. Clin J Sport Med 1995; 5:223-228Crossref, Medline, Google Scholar
25. Diggle PJ, Liang K, Zeger SL: Analysis of Longitudinal Data. Oxford, UK, Oxford University Press, 1995Google Scholar
26. Gibbons RD, Hedeker D, Elkin I, Waternaux C, Kraemer HC, Greenhouse JB, Shea MT, Imber SD, Sotsky SM, Watkins JT: Some conceptual and statistical issues in analysis of longitudinal psychiatric data. Arch Gen Psychiatry 1993; 50:739-750Crossref, Medline, Google Scholar
27. Vermeulen A, Kaufman JM, Giagulli VA: Influence of some biological indexes on sex hormone-binding globulin and androgen levels in aging or obese males. J Clin Endocrinol Metab 1996; 81:1821-1826Medline, Google Scholar
28. Daly RC, Schmidt PJ, Roca CA, Rubinow DR: Testosterone’s effects not limited to mood. Arch Gen Psychiatry 2001; 58:403-404Crossref, Medline, Google Scholar
29. Daly RC, Su TP, Schmidt PJ, Pickar D, Murphy DL, Rubinow DR: Cerebrospinal fluid and behavioral changes after methyltestosterone administration: preliminary findings. Arch Gen Psychiatry 2001; 58:172-177Crossref, Medline, Google Scholar
30. Mulchahey JJ, Ekhator NN, Zhang H, Kasckow JW, Baker DG, Geracioti TD Jr: Cerebrospinal fluid and plasma testosterone levels in post-traumatic stress disorder and tobacco dependence. Psychoneuroendocrinology 2001; 26:273-285Crossref, Medline, Google Scholar
31. Shifren JL, Braunstein GD, Simon JA, Casson PR, Buster JE, Redmond GP, Burki RE, Ginsburg ES, Rosen RC, Leiblum SR, Caramelli KE, Mazer NA: Transdermal testosterone treatment in women with impaired sexual function after oophorectomy. N Engl J Med 2000; 343:682-688Crossref, Medline, Google Scholar
32. Wilson IC, Prange AJ Jr, Lara PP: Methyltestosterone with imipramine in men: conversion of depression to paranoid reaction. Am J Psychiatry 1974; 131:21-24Link, Google Scholar
33. Rolf C, Nieschlag E: Potential adverse effects of long-term testosterone therapy. Baillières Clin Endocrinol Metab 1998; 12:521-534Crossref, Medline, Google Scholar
34. Guay AT, Perez JB, Fitaihi WA, Vereb M: Testosterone treatment in hypogonadal men: prostate-specific antigen level and risk of prostate cancer. Endocr Pract 2000; 6:132-138Crossref, Medline, Google Scholar
35. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8-19Crossref, Medline, Google Scholar



