Major Depression in Elderly Home Health Care Patients
Abstract
OBJECTIVE: Despite the growth of geriatric home health services, little is known about the mental health needs of geriatric patients seen in their homes. The authors report the distribution, correlates, and treatment status of DSM-IV major depression in a random sample of elderly patients receiving home health care for medical or surgical problems. METHOD: Geriatric patients newly admitted to a large, traditional visiting nurse agency were sampled on a weekly basis over a period of 2 years. The 539 patients ranged in age from 65 to 102 years; 351 (65%) were women, and 81 (15%) were nonwhite. The Structured Clinical Interview for DSM-IV Axis I Disorders was used to interview patients and informants. The authors reviewed the results of these interviews plus the patients’ medical charts to generate a best-estimate DSM-IV psychiatric diagnosis. RESULTS: The patients had substantial medical burden and disability. According to DSM-IV criteria, 73 (13.5%) of the 539 patients were diagnosed with major depression. Most of these patients (N=52, 71%) were experiencing their first episode of depression, and the episode had lasted for more than 2 months in most patients (N=57, 78%). Major depression was significantly associated with medical morbidity, instrumental activities of daily living disability, reported pain, and a past history of depression but not with cognitive function or sociodemographic factors. Only 16 (22%) of the depressed patients were receiving antidepressant treatment, and none was receiving psychotherapy. Five (31%) of the 16 patients receiving antidepressants were prescribed subtherapeutic doses, and two (18%) of the 11 who were prescribed appropriate doses reported not complying with their antidepressant treatment. CONCLUSIONS: Geriatric major depression is twice as common in patients receiving home care as in those receiving primary care. Most depressions in patients receiving home care are untreated. The poor medical and functional status of these patients and the complex organizational structure of home health care pose a challenge for determining safe and effective strategies for treating depressed elderly home care patients.
Home care has grown into a vital source of health care, especially for older adults, who represent 72% of recipients (1). Little is known about the mental health needs of these patients. In this article we report the distribution, correlates, and treatment status of DSM-IV major depression in a random sample of elderly patients receiving home health care for medical or surgical problems. Because major depression is associated in more healthy populations with significant risk for mortality, morbidity, institutionalization, and functional decline (2–8), investigating the extent to which depression affects home health care recipients represents an important step toward improving the clinical care and outcomes of this medically and functionally compromised patient population.
Home care services for patients confined to their homes by illness and disability is an important component of the overall health care system. Home care agencies typically offer a range of services, including skilled nursing care, occupational therapy, physical therapy, and home assistance. The great majority of home care patients (85%) are referred for medical or surgical diagnoses for which they receive skilled nursing care (9, 10).
In the past two decades, use of home care services and the sector itself have grown rapidly. Between 1987 and 1997, Medicare’s spending for home care rose at an annual rate of 21%, and home care’s share of total Medicare expenditures increased from 2% to 9% (11). During this time, the number of agencies certified by Medicare and the number of patients served annually doubled. In 1997, home health care cost Medicare $16.7 billion and served approximately 4 million Medicare enrollees, most of whom (85%) received skilled nursing care (9–11). Federal projections through 2008 estimate that the cost of home health care services will rise at a faster rate than the economy (12). Factors fueling this rapid growth include increased size and longevity of the elderly population, shorter hospital stays, expansion of Medicare eligibility, and technological advances allowing delivery of more complex care in the home (11).
This study is the first, to our knowledge, to investigate major depression among elderly recipients of home care nursing in the United States. Several investigators have reported high prevalence rates of depressive syndromes in elderly recipients of home-based health and social services in other countries (13–17). U.S. investigations have generally relied on convenience samples (18–20), chart diagnoses (21), or symptom screens (19, 20), which limit their utility for determining treatment needs (2, 3).
High prevalence rates of current major depression have been reported in other medically ill or disabled elderly populations, including medical inpatients (11.5%–13.2%) (22, 23) and nursing home residents (9.7%–12.6%) (24–26). These rates exceed those in elderly community samples (0.7%–1.4%) (27–29) and primary care patients (6.5%–9.0%) (30, 31). On the basis of these data we expected that major depression would be highly common in home care patients and associated with greater medical morbidity, disability, and pain.
We also hypothesized that major depression in these patients would be largely undetected and untreated. Efficacious treatments for depression are available and can be effectively used in medically ill elderly patients (3). In elderly primary care patients, however, depression goes undiagnosed more often than not, and, when diagnosed, is often inadequately treated (32).
Method
This study received full review and approval from the Institutional Review Board of Weill Medical College of Cornell University. All patients included in the study provided signed informed consent.
Sample
The study drew a random sample of elderly patients newly admitted to the Visiting Nurse Services in Westchester, a traditional, not-for-profit certified home health agency serving a 450-square-mile county north of New York City. Visiting nurse services originated in the late 1800s and are now found throughout the United States (11). Like many home health agencies, the collaborating agency employed social workers but no psychiatric nurses when these data were collected. Partially in response to its collaboration in this project, the agency has since opened a division of psychiatric home health care.
The study’s sampling strategy was designed to recruit a representative sample of agency patients admitted over a 2-year period (Dec. 1997 to Dec. 1999) who met the following criteria: 1) age 65 years old or older, 2) new admission, 3) able to give informed consent, and 4) able to speak English or Spanish. On a weekly basis, visiting nurse services admission data for each new patient were evaluated for potential study eligibility.
From the 3,416 potentially eligible patients, the study selected 40% at random (N=1,359); 470 patients (35%) were identified subsequently as ineligible. The primary reasons for ineligibility were termination from home care (by death, institutionalization, or recovery) and inability to give informed consent. Physicians and home health nurses were notified when their patients were sampled so they could notify the study if patients were inappropriate for study inclusion. The research associate fully explained the study aims and procedures to eligible patients, and 539 patients (61%) subsequently signed consent to participate.
Aggregate data provided by the agency indicated that, on average, participants were 2 years younger than patients who refused (mean age=78.4 years, SD=7.5, versus mean=80.2 years, SD=7.3) (t=3.58, df=885, p<0.001) but did not differ significantly by gender, nurse-reported mental status (e.g., disoriented, forgetful, depressed), prognosis, or ICD referring diagnosis (33).
Participants were interviewed in their homes. With the patient’s permission, the study also obtained information about depression from an informant (informants were available for 355 patients [66%]). The majority of informants were spouses (N=144 [41%]) or adult children (N=131 [37%]). Patients with informant data did not differ from patients without informants in age, ethnicity, cognitive function, or functional status, but significantly more were men (χ2=5.39, df=1, p<0.03), married (χ2=35.1, df=1, p<0.0001), and living with children (χ2=3.82, df=1, p<0.06), and they had significantly more comorbid medical diagnoses (34) (mean=2.8, SD=2.1, versus mean=2.3, SD=1.9) (t=2.61, df=537, p<0.009).
Measures
Data reported in this paper come from the patient interview, informant interview, and visiting nurse services medical records (Health Care Financing Administration form 485).
To assess current and past history of depression, the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) (35) was given to patients and informants by research associates trained in its use. Interrater reliability in the assessment of SCID symptoms was evaluated by having a second research associate observe and independently rate symptoms during in-person interviews with 42 patients. Reliability was excellent (intraclass r=0.91, 95% confidence interval [CI]=0.86–0.95) for the number of symptoms present. Interviewer ratings were monitored throughout the study by the study psychologist (P.J.R.).
To protect patient confidentiality, research associates informed patients of symptoms consistent with a diagnosis of major depression and suggested they discuss these symptoms with their physician or home care nurse. In cases of high suicide risk, the research associates immediately notified the agency and physician, following a prescribed protocol.
A DSM-IV diagnosis of current major depression was determined by using consensus best-estimate conferences (36, 37) that included the study’s geriatric psychiatrist (B.S.M.), geriatrician (D.J.K.), clinical psychologist (P.J.R.), and principal investigator (M.L.B.). The conference reviewed information from the patient SCID, informant SCID, and medical record data on medications and medical status. Case presentations protected the individual identity of the patient. Diagnoses of major depression followed DSM-IV’s “etiologic” approach, which excludes from diagnostic criteria symptoms judged solely attributable to general medical conditions or medications, a distinction that clinicians are able to judge reliably (38).
The test-retest reliability of the consensus best-estimate process was evaluated approximately 6 months after the final patient follow-up interview. Thirty previously reviewed patients were randomly selected, stratified by depression severity, and reevaluated by the panel. Reliability for the three-level outcome of major, subthreshold, or no depression was excellent (weighted kappa=0.89, 95% CI=0.77–1.00).
Cognitive impairment was assessed by using the Mini-Mental State Examination (MMSE) (39). Medical morbidity was determined from the medical record and patient interview by a geriatric internist (D.J.K.) using the Charlson Comorbidity Index (34), excluding scores for psychiatric illness. This index takes into account both the number of illnesses and their severity by assigning different weights to each major category of disorder. The Charlson Comorbidity Index was originally created as a method for classifying medical comorbidity in order to predict mortality.
Disabilities in activities of daily living, instrumental activities of daily living, and mobility were measured by counts of activities that the patient was unable to do without assistance (40). Pain intensity was assessed by the single three-level item from the Medical Outcomes Study 36-item Short-Form Health Survey (41). Poverty status was estimated by using an algorithm that compared self-reported household income and family size with 1998 U.S. Department of Health and Human Services poverty guidelines (42, 43).
Medication use was obtained from the medical record augmented by in-home review of medications. For antidepressants, dose adequacy was coded by using the Composite Antidepressant Treatment Intensity Scale (44). Adherence to antidepressant medication was assessed by self-report; patients were classified as adherent if they used the medication as prescribed and forgot no more than 20% of weekly doses.
Statistical Analyses
Chi-square and t tests were used in bivariate analyses of major depression and sociodemographic, clinical, and functional factors. Logistic regression models estimated whether these factors were independently associated with major depression. Variables initially entered into the logistic model included age, gender, and variables whose bivariate relationship with depression was significant at p<0.25 (45). Likelihood ratio chi-square tests were computed to eliminate nonsignificant variables from the model by using a stepwise procedure. The final model included age, gender, and variables significant at p<0.10. Odds ratios were computed for the final model with 95% confidence intervals. All analyses were performed by using SAS software (46), and tests of significance were two-tailed.
Results
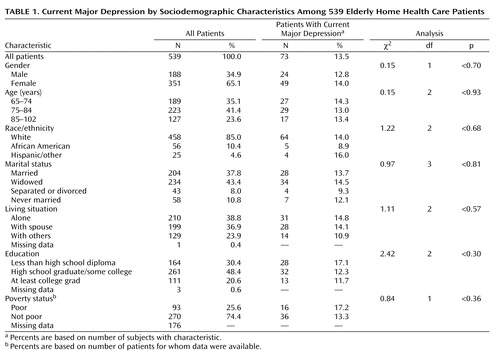
The demographic characteristics of the 539 patients (Table 1) were similar to national statistics of home care patients (1). Patients’ ages ranged from 65 to 102 years (mean=78.4, SD=7.5). The majority (65%) were female; 10% were African American, and 5% were Hispanic or other. Most patients lived alone (39%) or with a spouse (37%). Among the 363 patients with income data, 26% lived in poverty.
Most patients (N=347 [65% of the 534 patients for whom data were available]) began home care directly on hospital discharge; 121 (23%) were admitted after leaving nursing homes or rehabilitation facilities. The 539 patients had been referred by 359 different physicians.
Similar to home care patients nationally (9), the most common referral diagnoses were circulatory diseases (N=164 [30%]), injuries (N=76 [14%]), and cancer (N=57 [11%]). Most patients had multiple medical conditions; the overall Charlson Comorbidity Index medical morbidity ranged from 0 to 10 (mean=2.7, SD=2.1). Ninety-six patients (18%) scored lower than 24 on the MMSE, indicating mild to severe cognitive impairment. More than half (N=289 [55% of the 527 patients for whom data were available]) reported at least one disability in activities of daily living (mean=1.1, SD=1.3, range=0–6). The sample averaged 3.3 disabilities in instrumental activities of daily living (SD=1.5, range=0–6) and 2.0 mobility restrictions (SD=1.0, range=0–3).
In comparison with the full population of elderly Medicare beneficiaries (47), this sample of home care patients was older (24% versus 11% were 85 years old or older), disproportionately female (65% versus 57%), and more likely to live in poverty (26% versus 11%) but similar in racial/ethnic distribution. Compared with all Medicare beneficiaries, these home care patients were more than twice as likely to report at least one disability in activities of daily living (55% versus 23%).
According to DSM-IV criteria, 73 (13.5%) of the 539 patients (95% CI=10.8%–16.7%) were diagnosed with major depression. According to all available evidence, 52 (71%) of these 73 patients were classified as having their first episode of depression, although the accuracy of reported past history could not be determined and may be underestimated, as in other studies in late life (48). Patients with reported new-onset depression were similar to those who had a previous episode on sociodemographic characteristics, medical comorbidity, and functional ability, but they were more likely to score below 24 on the MMSE (14 [27%] of 51 patients for whom MMSE data were available compared with one [5%] of 21) (Fisher’s exact test, p=0.05). In most cases (N=57 [N=78%]), the episode of depression had lasted at least 2 months (mean=13.3 months, SD=15.3, range=<1 to 60).
In bivariate analyses, major depression was not significantly associated with any sociodemographic factors (Table 1) but was associated with greater medical morbidity, disability in instrumental activities of daily living, mobility disability, reported pain, and a past history of depression (Table 2). The relationships of major depression with medical morbidity (adjusted odds ratio=1.13, 95% CI=1.01–1.27 per Charlson Comorbidity Index point, Wald χ2=4.37, df=1, p<0.04), instrumental activities of daily living function (adjusted odds ratio=1.25, 95% CI=1.02–1.52, Wald χ2=4.67, df=1, p<0.03), reported pain (adjusted odds ratio=1.82, 95% CI=1.27–2.62, Wald χ2=10.64, df=1, p<0.001), and past history of depression (adjusted odds ratio=4.33, 95% CI=2.29–8.20, Wald χ2=20.28, df=1, p<0.0001) remained significant in a multivariate logistic regression model controlling for age and gender. The relationship with mobility did not remain significant. Statistical interactions among these variables were tested, but none was significant.
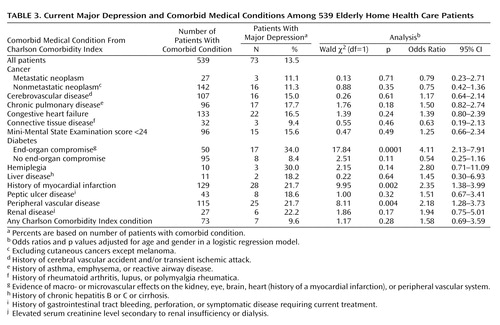
Consistent with the strong association between overall medical morbidity and major depression, three specific Charlson Comorbidity Index medical conditions had significantly higher rates of major depression when we controlled for age and gender (Table 3): diabetes with end-organ compromise (adjusted odds ratio=4.11, 95% CI=2.13–7.91), history of myocardial infarction (adjusted odds ratio=2.35, 95% CI=1.38–3.99), and peripheral vascular disease (adjusted odds ratio=2.18, 95% CI=1.28–3.73). When statistical significance was set at p<0.004 to account for multiple comparisons (49), all three conditions remained at least marginally significant (p<0.004). Several other medical conditions were positively associated with major depression but had limited statistical power.
Consistent with medical/surgical home care services, no patient had a psychiatric disorder listed as primary diagnosis on the home care medical record. Depression (ICD-9: 296.2, 296.3, 311.0) was a secondary diagnosis in 15 (3%) of the 539 patients, including two (3%) of the 73 patients with major depression.
Among the 73 depressed patients, 16 (22%) were receiving antidepressant treatment and none was receiving psychotherapy. Five (31%) of the 16 patients receiving antidepressants were prescribed subtherapeutic doses according to treatment guidelines (50). Of the 11 patients prescribed appropriate doses, two (18%) reported not complying with their antidepressant treatment. According to these definitions, nine (12%) of 73 home care patients diagnosed with major depression were receiving adequate treatment.
Conclusions
This study’s primary finding is that 13.5% of newly admitted, geriatric home health care patients suffered from major depression. The majority of depressed patients (78%) were not receiving treatment for depression. Of those treated, a third had not been prescribed an appropriate dose according to accepted treatment guidelines.
In assessing major depression in elderly home care patients, the study hoped to determine the treatment needs of this large and growing patient population. Intensive diagnostic procedures were chosen to address the difficulties of accurately diagnosing depression in the elderly and medically ill. On the one hand, depression can be underestimated because many older adults minimize psychological symptoms and attribute sleep disturbances, fatigue, and other somatic symptoms of depression to physical health causes (51, 52). On the other hand, the prevalence of major depression can be inflated in medically ill populations by misattributing symptoms of medical illness, medication side effects, or treatment sequelae to depression. Because we chose methods designed to minimize both potential sources of diagnostic measurement error, we believe that the estimated prevalence of major depression has clinical significance in this sample.
Is 13.5% a high rate of major depression? Research demonstrates that depression is both prevalent throughout the life span and costly in terms of individual suffering, negative sequelae, and health care utilization (3). Embedded in this literature are debates on whether depression is better conceptualized and measured as a diagnosis or spectrum of symptoms (53, 54) and whether diagnoses are more validly or reliability assessed by clinical judgment or self-report (55–57). We chose what might be considered the most conservative approach, using clinical judgment to make a strict DSM-IV diagnosis. Using similar criteria and procedures, Lyness et al. (30) reported a prevalence of 6.5% in a representative sample of older primary care patients. The difference between that rate and the rate of 13.5% in our sample suggests that depression is twice as common in elderly home care patients.
In these patients, depression was usually first-onset, persistent, and associated with medical comorbidity, disability, and reported pain. These correlates have been implicated in both the risk and outcome of late life depression (58, 59). These findings suggest that these complex and difficult-to-disentangle relationships persist even among patients suffering severe medical burden and disability. The specific associations with myocardial infarction, peripheral vascular disease, and diabetes are consistent with theories of vascular depression (60). The sustained episodes suggest that depression was often more than a brief reaction to the events precipitating home care and may be associated with long-term declines in medical and functional status.
Factors that potentially limit the generalizability of these findings are sampling from a single agency and the 39% refusal rate. The agency is similar to visiting nurse services agencies throughout the United States, however, and the sample characteristics are similar to national norms (9). The refusal rate reflects the challenges of conducting research with medically ill, frail patients in nonacademic settings and is consistent with other recent U.S. studies conducted in the homes of medically ill older adults (61–63). Patients who refused were surprisingly similar to participants.
Any attempt to characterize the needs of home care patients is challenged by the volatile home care environment. The Balanced Budget Act of 1997 restricted Medicare reimbursement for home health care in an effort to curb rising Medicare costs. Our sample was accrued during this period of constriction in Medicare spending. How these changes, as well as Medicare’s recently implemented home care prospective payment system, affect the needs and treatment options for older patients is not yet known.
Because major depression can be successfully treated in older patients (3), our finding that depression is not only prevalent but mostly untreated in home health care patients is important for clinical practice. The complex configuration of home care presents a challenge to identifying depression in these patients. Physicians have little opportunity for directly assessing their home health care patients, unlike the patients they see in primary care. The visiting nurse generally serves as the eyes and ears of the physician, thereby playing a key role in establishing the presence of depression and potential need for treatment.
Depressive symptoms are an accepted component of a comprehensive geriatric assessment (64, 65), and nurses are now expected to assess depressive symptoms as part of the Health Care Financing Administration’s mandatory use, collection, encoding, and transmission of outcome and assessment set (66). However, home health nurses typically are not trained in the assessment of depression or in diagnostic criteria (67), limiting the usefulness of their observations for making treatment decisions (68). This study found that over 40% of the depressed patients receiving antidepressant therapy received inadequate treatment either because the prescribed dose was below recommended guidelines or the patient was noncompliant. Accordingly, home care strategies are needed to improve treatment initiation and management as well as case identification. The challenge is to improve depression care in the context of the complex organization of the nurse-physician-patient triad, the increasing time and financial pressures faced by both home care agencies and physicians, and patient frailty.
Effective strategies will likely draw from three areas of research. First are primary care interventions to improve treatment of geriatric depression through the use of structured treatment guidelines and care managers (32, 69). Second are comprehensive home-based interventions that target the full range of nursing and psychosocial needs in geriatric patients (62, 63, 70). Third are “telemedicine” strategies to facilitate clinical care for hard-to-reach populations, such as the rural and homebound (71).
The immediate goal of any depression intervention in home health care is recovery from depression and reduction of depressive symptoms. Data from other populations suggest that treating depression may reduce the risk of negative functional outcomes as well. Functional outcomes are especially important in home health care, both because good functional status is critical in allowing older adults to remain in their own homes and because Medicare’s prospective payment system bases reimbursement on functional outcomes. Despite the availability of efficacious treatments for depression, however, only nine (12%) of our depressed home care patients received adequate antidepressant treatment. This magnitude of untreated major depression underscores the critical need for effective strategies to reduce the burden of depression in older home health care patients.
 |
 |
 |
Received Nov. 26, 2001; revision received March 27, 2002; accepted April 4, 2002. From the Department of Psychiatry and the Division of Geriatrics, Weill Medical College of Cornell University; the School of Public Health, Columbia University, New York; and the Visiting Nurse Services in Westchester, N.Y. Address reprint requests to Dr. Bruce, Department of Psychiatry, Westchester Division, Weill Medical College of Cornell University, 21 Bloomingdale Rd., White Plains, NY 10605; [email protected] (e-mail). Supported by NIMH grants MH-56482 and MH-01634. The authors thank the nurses, administrators, other staff, and patients of the Visiting Nurse Services in Westchester for their support for this project.
1. Haupt BJ, Jones A: The National Home and Hospice Care Survey: 1996 summary. Vital Health Stat 1999; 13:1-238Google Scholar
2. NIH Consensus Panel on Diagnosis and Treatment of Depression in Late Life: Diagnosis and treatment of depression in late life. JAMA 1992; 268:1018-1024Crossref, Medline, Google Scholar
3. Lebowitz BD, Pearson JL, Schneider LS, Reynolds CF III, Alexopoulos GS, Bruce ML, Conwell Y, Katz IR, Meyers BS, Morrison MF, Mossey J, Niederehe G, Parmelee P: Diagnosis and treatment of depression in late life: consensus statement update. JAMA 1997; 278:1186-1190Crossref, Medline, Google Scholar
4. Murray CG, Lopez AD: The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability From Disease, Injuries, and Risk Factors in 1990 and Projected to 2020. Geneva, World Health Organization, 1996Google Scholar
5. Bruce ML, Leaf PJ: Psychiatric disorders and 15 month mortality in a community sample of older adults. Am J Public Health 1989; 79:727-730Crossref, Medline, Google Scholar
6. Bruce ML, Leaf PJ, Rozal GPM, Florio L, Hoff RA: Psychiatric status and 9-year mortality data in the New Haven Epidemiologic Catchment Area study. Am J Psychiatry 1994; 151:716-721Link, Google Scholar
7. Bruce ML, Seeman TE, Merrill SS, Blazer DG: The impact of depressive symptomatology on physical disability: MacArthur Studies of Successful Aging. Am J Public Health 1994; 84:1796-1799Crossref, Medline, Google Scholar
8. Ford AB, Roy AW, Haug MR, Folmar SJ, Jones PK: Impaired and disabled elderly in the community. Am J Public Health 1991; 81:1207-1209Crossref, Medline, Google Scholar
9. Munson ML: Characteristics of Elderly Home Health Care Users: Data From the 1994 National Home and Hospice Care Survey: Advanced Data From Vital and Health Statistics 309. Hyattsville, Md, National Center for Health Statistics, 1999Google Scholar
10. Kramarow E, Lentzner H, Rooks R, Weeks J, Saydah S: Health and Aging Chartbook: Health, United States 1999. Hyattsville, Md, National Center for Health Statistics, 1999Google Scholar
11. Health Care Financing Administration Office of Strategic Planning: A Profile of Medicare Home Health. Washington, DC, HCFA, 1999Google Scholar
12. Centers for Medicare and Medicaid Services: Health Care Financing Administration National Health Expenditures Projects:1998-2008. http://www.hcfa.gov/stats/nhe-oact/default.htmGoogle Scholar
13. Banerjee S: Prevalence and recognition of psychiatric disorder in the elderly clients of a community care service. Int J Geriatr Psychiatry 1993; 8:125-131Crossref, Google Scholar
14. Kivela SL, Lehtomake E, Kivekas J: Prevalence of depression symptoms and depression in elderly Finnish home nursing patients and home help clients. Int J Soc Psychiatry 1986; 32:3-13Crossref, Medline, Google Scholar
15. Nagatomo I, Takigawa M: Mental status of the elderly receiving home health services and the associated stress of home helpers. Int J Geriatr Psychiatry 1998; 13:57-63Crossref, Medline, Google Scholar
16. Iliffle S, Haynes A, Booroff A, Golderberg E, Morgan P: Assessment of elderly people in general practice, IV: depression, functional ability and contact with services. Br J Gen Pract 1993; 43:371-374Medline, Google Scholar
17. Harrison R, Savla N, Kaftez K: Dementia, depression, and physical disability in a London borough: a survey of elderly people in and out of residential care and implications for future development. Age Aging 1990; 19:97-103Crossref, Medline, Google Scholar
18. Levy MT: Psychiatric assessment of elderly patients in the home: a survey of 176 cases. J Am Geriatr Soc 1985; 33:9-12Crossref, Medline, Google Scholar
19. Krach P, DeVaney S, DeTurk C, Zink MH: Functional status of the oldest-old in a home setting. J Adv Nurs 1996; 24:456-464Crossref, Medline, Google Scholar
20. Kennedy CW, Polivka BJ, Steel JS: Psychiatric symptoms in a community-based medically ill population. Home Healthc Nurse 1997; 15:431-441Crossref, Medline, Google Scholar
21. Horton-Deutsch SL, Farran CJ, Loukissa D, Fogg L: Who are these patients and what services do they receive? Home Healthc Nurse 1997; 15:845-854Crossref, Google Scholar
22. Koenig HG, Meador KG, Cohen HJ, Blazer DG: Depression in elderly hospitalized patients with medical illness. Arch Intern Med 1988; 148:1929-1936Crossref, Medline, Google Scholar
23. Koenig HG, O’Connor CM, Guarisco SA, Zabel M, Ford SM: Depressive disorder in older medical inpatients on general medicine and cardiology services at a university teaching hospital. Am J Geriatr Psychiatry 1993; 1:197-210Crossref, Medline, Google Scholar
24. Rovner BW, German PS, Brant LJ, Clark R, Burton L, Folstein MF: Depression and mortality in nursing homes. JAMA 1991; 265:993-996Crossref, Medline, Google Scholar
25. Phillips CJ, Henderson AS: The prevalence of depression among Australian nursing home residents: results using draft ICD-10 and DSM-III-R criteria. Psychol Med 1991; 21:739-748Crossref, Medline, Google Scholar
26. Parmelee PA, Katz IR, Lawton MP: Depression among institutionalized aged: assessment and prevalence estimation. J Gerontol Med Sci 1989, 44:M22-M29Google Scholar
27. Regier DA, Farmer ME, Rae DS, Myers JK, Kramer M, Robins LN, George LK, Karno M, Locke BZ: One-month prevalence of mental disorders in the United States and sociodemographic characteristics: the Epidemiologic Catchment Area study. Acta Psychiatr Scand 1993; 88:35-47Crossref, Medline, Google Scholar
28. Bland RC, Newman SC, Orn H: Prevalence of psychiatric disorders in the elderly in Edmonton. Acta Psychiatr Scand Suppl 1988; 338:57-63Crossref, Medline, Google Scholar
29. Henderson AS, Jorm AF, Mackinnon A, Christensen H, Scott LR, Korten AE, Doyle C: The prevalence of depressive disorders and the distribution of depressive symptoms in later life: a survey using draft ICD-10 and DSM-III-R. Psychol Med 1993; 23:719-729Crossref, Medline, Google Scholar
30. Lyness JM, Caine ED, King DA, Cox C, Yoediono Z: Psychiatric disorders in older primary care patients. J Gen Intern Med 1999; 14:249-254Crossref, Medline, Google Scholar
31. Schulberg HC, Mulsant B, Schulz R, Rollman BL, Houck PR, Reynolds CF III: Characteristics and course of major depression in older primary care patients. Int J Psychiatry Med 1998; 28:421-436Crossref, Medline, Google Scholar
32. Unutzer J, Katon W, Sullivan M, Miranda J: Treating depressed older adults in primary care: narrowing the gap between efficacy and effectiveness. Milbank Q 1999; 77:225-241Crossref, Medline, Google Scholar
33. The International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM), volume 1: Diseases Tabular List, 2nd ed: DHHS Publication PHS 80-1260. Washington, DC, US Government Printing Office, 1980Google Scholar
34. Charlson ME, Pompei P, Ales KL, MacKenzie CR: A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40:373-383Crossref, Medline, Google Scholar
35. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders (SCID). Washington, DC, American Psychiatric Press, 1995Google Scholar
36. Leckman JF, Sholomskas D, Thompson WD, Belanger A, Weissman MM: Best estimate of lifetime psychiatric diagnoses. Arch Gen Psychiatry 1982; 39:879-883Crossref, Medline, Google Scholar
37. Klein DN, Ouimette PC, Kelly HS, Ferro T, Riso LP: Test-retest reliability of team consensus best-estimate diagnoses of axis I and II disorders in a family study. Am J Psychiatry 1994; 151:1043-1047Link, Google Scholar
38. Koenig HG, Pappas P, Holsinger T, Bachar JR: Assessing diagnostic approaches to depression in medically ill older adults: how reliably can mental health professionals make judgments about the cause of symptoms? J Am Geriatr Soc 1995; 43:472-487Crossref, Medline, Google Scholar
39. Folstein MF, Folstein SE, McHugh PR: “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12:189-198Crossref, Medline, Google Scholar
40. Lawton MP, Brody EM: Assessment of older people: self-maintaining instrumental activities of daily living. Gerontologist 1969; 9:179-186Crossref, Medline, Google Scholar
41. Ware JE Jr, Sherbourne CD: The MOS 36-Item Short-Form Health Survey (SF-36), I: conceptual framework and item selection. Med Care 1992; 30:473-483Crossref, Medline, Google Scholar
42. Federal Register, vol 63, number 36, Feb 24, 1998, pp 9235-9238Google Scholar
43. Bruce ML, Takeuchi DT, Leaf P: Poverty and psychiatric status: longitudinal evidence from the New Haven Epidemiologic Catchment Area Study. Arch Gen Psychiatry 1991; 48:470-474Crossref, Medline, Google Scholar
44. Alexopoulos GS, Meyers BS, Young RC, Kakuma T, Feder M, Einhorn A, Rosendahl E: Recovery in geriatric depression. Arch Gen Psychiatry 1996; 53:305-312Crossref, Medline, Google Scholar
45. Hosmer DW, Lemeshow S: Applied Logistic Regression. New York, John Wiley & Sons, 1989Google Scholar
46. SAS/STAT User’s Guide, version 8. Cary, NC, SAS Institute, 1999Google Scholar
47. Health Care Financing Administration Office of Strategic Planning: A Profile of Medicare. Washington, DC, HCFA, 1998Google Scholar
48. Farrer LA, Florio LP, Bruce ML, Leaf PJ, Weissman MM: Reliability and consistency of self-reported age at onset of major depression. J Psychiatr Res 1989; 23:35-47Crossref, Medline, Google Scholar
49. Fleiss JL: The Design and Analysis of Clinical Experiments. New York, John Wiley & Sons, 1986Google Scholar
50. Depression Guideline Panel: Clinical Practice Guideline Number 5: Depression in Primary Care, 2: Treatment of Major Depression: AHCPR Publication 93-0551. Rockville, Md, US Department of Health and Human Services, 1993Google Scholar
51. Cohen-Cole SA, Stoudemire A: Major depression and physical illness: special considerations in diagnosis and biological treatment. Psychiatr Clin North Am 1987; 10:1-17Crossref, Medline, Google Scholar
52. Hasin D, Link B: Age and recognition of depression: implications for a cohort effect in depression. Psychol Med 1998; 18:683-688Crossref, Google Scholar
53. Mirowsky J, Ross CE: Psychiatric diagnosis as reified measurement. J Health Soc Behav 1989; 30:11-25Crossref, Medline, Google Scholar
54. Klerman GL: Comment on Mirowsky and Ross. J Health Soc Behav 1989; 30:26-32Crossref, Google Scholar
55. Regier DA: Limitations of diagnostic criteria and assessment instruments for mental disorders. Arch Gen Psychiatry 2000; 57:109-115Crossref, Google Scholar
56. Frances A: Problems in defining clinical significance in epidemiologic studies (comment). Arch Gen Psychiatry 2000; 57:119Crossref, Medline, Google Scholar
57. Spitzer RL: Diagnosis and need for treatment are not the same (comment). Arch Gen Psychiatry 2000; 57:120Google Scholar
58. Bruce ML: Depression and disability in late life: directions for future research. Am J Geriatr Psychiatry 2001; 9:102-112Crossref, Medline, Google Scholar
59. Pincus T, Williams A: Models and measurements of depression in chronic pain. J Psychosom Res 1999; 47:211-219Crossref, Medline, Google Scholar
60. Alexopoulos GS, Meyers BS, Young RC, Campbell S, Silbersweig D, Charlson M: “Vascular depression” hypothesis. Arch Gen Psychiatry 1997; 54:915-922Crossref, Medline, Google Scholar
61. Fried TR, van Doorn C, O’Leary JR, Tinetti ME, Drickamer MA: Older person’s preferences for home vs hospital care in the treatment of acute illness. Arch Intern Med 2000; 160:1501-1506Crossref, Medline, Google Scholar
62. Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, Schwartz JS: Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA 1999; 281:613-620Crossref, Medline, Google Scholar
63. Reuben DB, Frank JC, Hirsch SH, McGuigan KA, Maly RC: A randomized clinical trial of outpatient comprehensive geriatric assessment coupled with an intervention to increase adherence to recommendations. J Am Geriatr Soc 1999; 47:269-276Crossref, Medline, Google Scholar
64. Harper MS: Behavioral, social and mental health aspects of home care for older Americans. Home Health Care Serv Q 1989; 9:61-124Crossref, Google Scholar
65. Wykle ML: Geriatric mental health interventions in the home. J Gerontol Nurs 1995; 21:47-48Crossref, Medline, Google Scholar
66. Medicare and Medicaid Programs: Mandatory Use, Collection, Encoding and Transmission of Outcome and Assessment Set (OASIS) for Home Health Agencies. Federal Register, vol 64, number 117, June 18, 1999, pp 32984-32991Google Scholar
67. Dalton JR, Busch KD: Depression: the missing diagnosis in the elderly. Home Healthc Nurs 1995; 13:31-35Crossref, Medline, Google Scholar
68. Brown EL, McAvay GJ, Raue PJ, Moses S, Bruce ML: Recognition of depression in the elderly receiving homecare services. Psychiatr Serv (in press)Google Scholar
69. Bruce ML, Pearson JL: Designing an intervention to prevent suicide: PROSPECT (Prevention of Suicide in Primary Care Elderly: Collaborative Trial). Dialogues in Clin Neurosci 1999; 1:100-112Medline, Google Scholar
70. Stuck AE, Minder CE, Peter-Wüest I, Gillmann G, Egli C, Kesselring A, Leu RE, Beck JC: A randomized trial of in-home visits for disability prevention in community-dwelling older people at low and high risk for nursing home admission. Arch Intern Med 2000; 160:977-986Crossref, Medline, Google Scholar
71. Johnston B, Wheeler L, Deuser J, Sousa KH: Outcomes of the Kaiser Permanente Tele-Home Health Research Project. Arch Fam Med 2000; 9:40-45Crossref, Medline, Google Scholar



