Neuropsychological Function in Children With Maltreatment-Related Posttraumatic Stress Disorder
Abstract
OBJECTIVE: Studies in adults have reported changes in concentration, learning, and memory in individuals with posttraumatic stress disorder (PTSD). However, there are few studies of cognitive function in children with PTSD. The goal of the current study was to evaluate cognition in children with PTSD. METHOD: The cognitive status of 14 pediatric psychiatric outpatients with maltreatment-related PTSD and 15 sociodemographically similar children who were healthy and had not been maltreated was examined. Neuropsychological instruments measured language, attention, abstract reasoning/executive function, learning and memory, visual-spatial processing, and psychomotor function. RESULTS: The children with PTSD performed more poorly on measures of attention and abstract reasoning/executive function. CONCLUSIONS: Although based on a small number of subjects, these results support cognitive differences between children with and without maltreatment-related PTSD.
Posttraumatic stress disorder (PTSD) is now widely recognized in children. Although findings are equivocal (1), studies of adults have reported cognitive problems in individuals with PTSD, particularly in the areas of concentration, learning, and memory (2). In contrast, cognitive function indexed by performance on standardized neuropsychological instruments has not been extensively evaluated in children with PTSD. It is particularly important to characterize the neuropsychological deficits associated with childhood PTSD because they are likely to have broad developmental ramifications, affecting both response to therapy and school performance.
Unlike studies in adults with PTSD, neuroimaging studies indicate that PTSD in children is associated with diffuse CNS effects (i.e., smaller cerebral volumes and corpus callosum areas) but no anatomical changes in limbic structures (3). Functional imaging procedures indicate that medial prefrontal cortical dysfunction may be associated with both adult and pediatric PTSD (4). The neuropsychological consequences of these brain alterations have not been extensively studied.
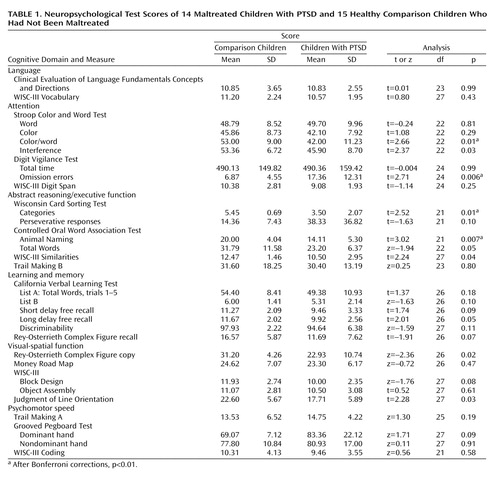
In this pilot study, we examined cognitive functioning using a battery of neuropsychological instruments measuring language, attention, abstract reasoning/executive function, learning and memory, visual-spatial processing, and psychomotor functioning in maltreated children with PTSD and sociodemographically similar comparison children who had not been maltreated and who did not have PTSD. The tests, described by Spreen and Strauss (5), are listed in Table 1. On the basis of neuroimaging research (3, 4), we hypothesized that the children with PTSD would perform more poorly on cognitive measures, particularly in the domains mediated by the prefrontal cortex.
Method
We recruited 14 medication-naive children with PTSD secondary to maltreatment who were psychiatric outpatients and 15 healthy comparison children who had not been maltreated and who were similar to the PTSD patients in age, race, socioeconomic status, and IQ. The mean age of the PTSD patients was 11.38 years (SD=2.60) and that of the comparison children was 12.17 (SD=1.75). Six of the PTSD patients were girls and eight were boys; seven of the comparison subjects were girls and eight were boys. In the PTSD group, 10 patients were white, two were African American, and two were biracial (white and African American); in the comparison group, 12 subjects were white, one was African American, and two were biracial. In the PTSD group, the mean socioeconomic level according to the Hollingshead Four-Factor Index of Socioeconomic Status (6) was 39.21 (SD=11.28); in the comparison group the mean was 39.60 (SD=7.69). The mean full-scale IQ (estimated by the WISC-III four-factor score [7]) was 105.71 (SD=11.89) in the PTSD group and 113.20 (SD=11.69) in the comparison group.
After complete description of the study was given to the children and their parents, written informed consent was obtained. All of the children assented to their participation. Subjects received monetary compensation for participation.
A board-certified child psychiatrist (M.D.D.) conducted psychiatric interviews of all subjects and their legal guardians using a detailed trauma interview described elsewhere (8). A master’s-level clinician, blind to clinical status, completed a modified version of the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version (9). The diagnosis of the children with chronic PTSD was based on DSM-IV. The traumata they experienced included sexual abuse (N=7), physical abuse (N=2), and witnessing domestic violence (N=5). Comorbid disorders included major depressive disorder (N=5), dysthymic disorder (N=2), separation anxiety disorder (N=2), oppositional defiant disorder (N=6), and attention deficit hyperactivity disorder (inattentive subtype) (N=1). Comparison subjects had no lifetime history of any axis I diagnosis.
Inclusion criteria for the PTSD group were “reported and indicated” child maltreatment experiences noted by child protective services before this investigation, the availability of one nonabusing caregiver who could cooperate with this protocol, and a stable home environment (i.e., the child had not been in danger from the perpetrator[s] for at least the previous 3 months). Exclusion criteria for all subjects included birth complications; substantial medical illness; head injury associated with wounds requiring sutures, emergency room treatment, or loss of consciousness; gross obesity (i.e., weight greater than 150% of ideal body weight) or growth failure (i.e., height less than the third percentile); Wechsler full-scale IQ less than 80; history of treatment with psychotropic medications; anorexia nervosa, pervasive developmental disorder, schizophrenia, adolescent-onset alcohol or substance abuse or dependence; prenatal exposure to alcohol and/or other substance use greater than twice a month during the 3 months before discovery of pregnancy; and mother’s use of controlled substances during the known period of pregnancy.
Subjects completed a comprehensive neuropsychological battery administered blind to whether the child did or did not have PTSD. Instruments are described in Spreen and Strauss (5) and listed in Table 1.
We evaluated the distribution of our data for normality using Shapiro and Wilks’s W statistics. When no transformation normalized the data, we applied nonparametric tests. Student’s t test or Wilcoxon/Kruskal-Wallis rank sums were used to assess between-group differences on cognitive results. Two-tailed alpha equaled 0.05; analyses were completed with Statistical Discovery Software (SAS Institute, Cary, N.C.).
Results
Children with PTSD performed more poorly on measures in four of the six cognitive domains (Table 1). In the domain of attention, PTSD subjects performed more poorly on two measures of freedom from distractibility, Stroop Color and Word Test color/word and interference. The PTSD group made significantly more omission errors on a measure of sustained visual attention (Digit Vigilance Test).
On measures of problem solving and abstract reasoning/executive function, PTSD subjects completed fewer categories on the Wisconsin Card Sorting Test. On two measures of semantic organization, the Controlled Oral Word Association Test Animal Naming and the Total Words, children with PTSD generated fewer category members and named fewer words beginning with target letters (i.e., F, A, S). Significant differences were also identified on WISC-III Similarities; again, the children with PTSD scored lower than the comparison subjects.
Children with PTSD performed more poorly on one test of learning and memory, the California Verbal Learning Test long delay free recall. Finally, on measures of visual-spatial function, children with PTSD completed a poorer copy of the Rey-Osterrieth Complex Figure and made more errors on the Judgment of Line Orientation.
No significant differences between groups were found on any tests of language or psychomotor speed. After a Bonferroni correction for multiple comparisons was applied within each of the cognitive domains, only results within the domains of attention (i.e., Stroop color/word and Digit Vigilance Test omission errors) and abstract reasoning/executive function (i.e., Wisconsin Card Sorting Test categories and Controlled Oral Word Association test Animal Naming) remained significant.
In the PTSD group, variables that remained significant between groups were correlated with the number of clinical symptoms grouped by PTSD clusters (i.e., cluster B, intrusive symptoms; cluster C, avoidant symptoms; and cluster D, increased arousal symptoms) by applying Spearman’s rank-order correlation. After Bonferroni corrections for multiple correlations, no significant correlations were seen between clinical symptoms and cognitive variables.
Discussion
Children with maltreatment-related PTSD demonstrated significant deficits within the domains of attention and abstract reasoning/executive function when compared with sociodemographically similar healthy children who had not been maltreated. The children with PTSD were more susceptible to distraction and demonstrated greater impulsivity, making more errors on a task of sustained attention. Children with PTSD also demonstrated deficits on two tests designed to measure frontal lobe function (10)—the Wisconsin Card Sorting Test, an instrument requiring hypothesis testing and problem solving, and the Controlled Oral Word Association Test, a measure of semantic organization. These findings are consistent with neuroimaging studies showing CNS changes in the frontal cortex in PTSD (4). In contrast, after corrections to protect from experiment-wise error, PTSD children did not perform differently from comparison children on measures of language, memory and learning, visual-spatial abilities, or psychomotor skills.
Memory problems associated with PTSD are commonly identified in adults (2). We were unable to replicate the findings of Moradi et al. (11) of general memory deficits associated with childhood PTSD. However, the small number of subjects in our study may have obscured significant findings in this domain. Our findings suggest deficits in long-term memory for verbal information.
The study reported here must be considered preliminary because of the lack of a comparison group of children who had been maltreated but did not have PTSD. Therefore, we do not know if our results are related to maltreatment or the presence of an anxiety disorder. Additionally, these findings may be explained by the presence of comorbid psychiatric disorders, particularly mood disorders, in the children with PTSD. Although it is tempting to assert that psychiatric symptoms may account for neuropsychological deficits, further research is necessary to ascertain how psychiatric symptoms interact with neuropsychological deficits.
 |
Received May 11, 2001; revision received Aug. 21, 2001; accepted Oct. 9, 2001. From the Department of Psychiatry and the Developmental Traumatology Neuroimaging Laboratory, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine. Address reprint requests to Dr. Beers, Western Psychiatric Institute and Clinic, 3811 O’Hara St., Pittsburgh, PA 15213; [email protected] (e-mail). Supported in part by NIMH grant MH-01324-02 (Dr. De Bellis) and 1995 and 1998 National Alliance for Research on Schizophrenia and Depression Young Investigator Awards. The authors thank Grace Moritz, M.S.W., and Julie Hall, B.A., for their assistance in this work.
1. Barrett DH, Green ML, Morris R, Giles WH, Croft JB: Cognitive functioning and posttraumatic stress disorder. Am J Psychiatry 1996; 153:1492-1494Link, Google Scholar
2. McNally RJ: Experimental approaches to cognitive abnormality in posttraumatic stress disorder. Clin Psychol Rev 1998; 18:971-982Crossref, Medline, Google Scholar
3. De Bellis MD, Keshavan M, Clark DB, Casey BJ, Giedd J, Boring AM, Frustaci K, Ryan ND: AE Bennett Research Award: developmental traumatology, part II: brain development. Biol Psychiatry 1999; 45:1271-1284Crossref, Medline, Google Scholar
4. De Bellis MD, Keshavan MS, Spencer S, Hall J: N-Acetylaspartate concentration in the anterior cingulate of maltreated children and adolescents with PTSD. Am J Psychiatry 2000; 157:1175-1177Link, Google Scholar
5. Spreen O, Strauss E: A Compendium of Neuropsychological Tests, 2nd ed. New York, Oxford University Press, 1998Google Scholar
6. Hollingshead AB: Four-Factor Index of Social Status. New Haven, Conn, Yale University, Department of Sociology, 1975Google Scholar
7. Sattler JM: Assessment of Young Children, 3rd ed, revised. San Diego, JM Sattler, 1992Google Scholar
8. De Bellis MD: Posttraumatic stress disorder and acute stress disorder, in Handbook of Prevention and Treatment With Children and Adolescents. Edited by Ammerman RT, Hersen M. New York, John Wiley & Sons, 1997, pp 455-494Google Scholar
9. Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N: Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 1997; 36:980-988Crossref, Medline, Google Scholar
10. Levin HS, Culhane KA, Hartman J, Evankovich K, Mattson AJ: Developmental changes in performance on tests of purported frontal lobe functioning. Dev Neuropsychol 1991; 12:377-395Crossref, Google Scholar
11. Moradi AR, Doost HTN, Taghavi MR, Yule W, Dalgleish T: Everyday memory deficits in children and adolescents with PTSD: performance on the Rivermead Behavioral Memory test. J Child Psychol Psychiatry 1999; 40:357-361Crossref, Medline, Google Scholar



