Inpatient Antipsychotic Drug Use in 1998, 1993, and 1989
Abstract
OBJECTIVE: Patterns of clinical use of antipsychotic agents have changed greatly in the past decade. The authors’ goal was to examine these patterns. METHOD: They evaluated medication use in all McLean Hospital inpatients treated with antipsychotic drugs during 3 months in 1998 (N=349) and compared the results with McLean Hospital inpatients treated with antipsychotics in 1993 (N=299) and Boston area inpatients in 1989 (N=50). RESULTS: The most commonly prescribed antipsychotics in 1998 were atypical agents; olanzapine was prescribed more often than risperidone or quetiapine, which were prescribed more often than other antipsychotics. Two or more antipsychotics were prescribed at some time during their hospitalization for 150 (43%) of the patients in 1998. The total discharge dose in chlorpromazine equivalents for the 349 patients for whom antipsychotics were prescribed at discharge was 371 mg/day, 29% higher than the total discharge dose for patients in 1993 and 46% greater than the dose in 1989. The dose of antipsychotics was greater for patients with psychotic illnesses than for those with affective illnesses. Higher doses were associated with greater clinical improvement, polypharmacotherapy, and younger patient age. CONCLUSIONS: Emerging trends toward higher total antipsychotic doses and polypharmacotherapy require critical assessments of cost-benefit relationships.
We surveyed hospital practices in the Boston area regarding use of antipsychotic drugs in 1984, 1989, and 1993 (1, 2). In contrast to earlier American practices, mean chlorpromazine-equivalent daily doses fell by the late 1980s, to accord with standard international practices, and conservative dosing was sustained into the early 1990s (2, 3). More recently, growing numbers of atypical antipsychotics have entered clinical use, along with other innovative treatments (4). It is our clinical impression, supported by recent research reports (5–8), that simultaneous use of multiple dissimilar antipsychotics is increasing. Accordingly, we completed a new survey of antipsychotic use to document current trends compared with our earlier findings over the past decade (1, 2).
Method
Consecutive patients admitted to McLean Hospital in March–May 1998 who were treated with antipsychotic medications were considered. Following review and approval for confidential and anonymous use of aggregate data by the hospital’s institutional review board, we reviewed clinical records to determine the patient’s sex, age, discharge DSM-IV diagnosis, and all medications given, with their doses and times.
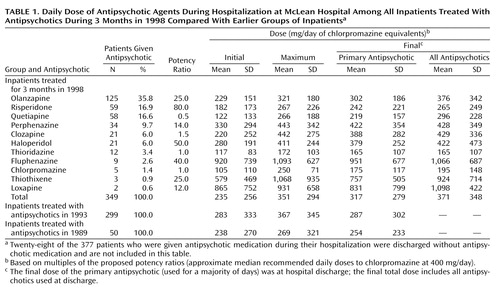
Doses of antipsychotics were converted to chlorpromazine equivalents (mg/day) on the basis of potency ratios of approximate median recommended daily doses to chlorpromazine at 400 mg/day (4) (Table 1). For each patient, we compiled initial, maximum, and final (discharge) doses of primary antipsychotic agents (those used for the majority of inpatient days), as well as the total final dose when multiple antipsychotics were given. Comparisons were made of McLean patients treated in 1998 (N=349) with similar McLean inpatients in 1993 (N=299) and Boston area patients in 1989 (N=50) (2). Data on patients’ clinical improvement were obtained from hospital discharge records.
Averages are means and standard deviations. Continuous data were compared by using one-way analysis of variance, paired t tests, or unpaired t tests for unequal groups across years. Categorical data were compared by using contingency tables (chi-square). Correlations were based on Spearman nonparametric rank methods (rs). Factors associated with median-split final total chlorpromazine-equivalent dose were evaluated by logistic regression multivariate methods (risk ratio and 95% confidence interval [CI]). We used Statview-5 programs (SAS Corp., Cary, N.C.) for statistical analyses.
Results
In the 3-month 1998 group, antipsychotics were prescribed for 377 (50%) of 754 psychiatric inpatients; antipsychotics were prescribed for 349 of these patients at the time of their hospital discharge. These 349 inpatients comprise the present study group of 211 women (60.0%) and 138 men (40.0%). The patients’ mean age was 45.7 years (SD=19.6, range=18–91), and they were hospitalized for a mean of 29.0 days (SD=26.2) (compared with a mean of 18.5 days in 1993 and 73.1 days in 1989). Their DSM-IV diagnoses were primary psychosis (N=136 [39.0%]), major depression (N=73 [20.9%]), bipolar disorder (N=78 [22.3%]), dementia (N=41 [11.7%]), substance use (N=8 [2.3%]), and miscellaneous disorders (N=13 [3.7%]). Average time from admission to first antipsychotic dose was 0.9 days (versus 1.5 in 1993 and 6.8 in 1989).
The ranking of antipsychotic use for the 349 patients was as follows: olanzapine 36%, risperidone 17%, quetiapine 17%, perphenazine 10%, clozapine 6%, and haloperidol for 6%; other typical neuroleptics were used for 3% or less of the patients (Table 1). An atypical agent was the initial treatment for 254 (72.8%) of the patients; women started with atypical agents nonsignificantly more often than men (N=107 [77.5%] compared with N=145 [69.7%]) (χ2=2.61, df=1, p=0.11). Frequency of atypical primary agents among all antipsychotics was similar across diagnostic groups: psychotic (N=101 [74.3%]), affective (N=108 [71.5%]), and other disorders (N=50 [80.6%]).
Atypical agents were used in lower initial chlorpromazine-equivalent doses than typical neuroleptics (mean=190 mg/day, SD=164, versus mean=318 mg/day, SD=384) (F=20.5, df=1, 375, p<0.0001) as well as in lower discharge doses (mean=277 mg/day, SD=202, versus mean=438 mg/day, SD=415) (F=22.9, df=1, 347, p<0.0001). Maximum and total final doses of chlorpromazine and thioridazine were the most conservative, and the doses of fluphenazine, loxapine, and thiothixene were the highest (Table 1).
At discharge, two or more antipsychotics were prescribed for 55 [15.8%] of the patients (37 [17.5%] of the women and 18 [13.0%] of the men). By diagnosis, discharge polypharmacotherapy ranked as follows: psychotic (N=34 [25.0%]), affective (N=16 [10.6%]), and other (N=5 [8.1%]) disorders (χ2=14.5, df=2, p=0.0007). However, this practice included 133 (38.1%) of patients at some time during hospitalization and accounted for 20.0% of inpatient days in 1998, compared with 5.7% of inpatient days in 1993 and 1.7% in 1989 (1, 2). Typical neuroleptics were added only to primary atypical antipsychotics, but atypical agents were combined with both typical (217 patients [62.2%]) and other atypical (132 patients [37.8%]) primary antipsychotics.
The chlorpromazine-equivalent mean dose at discharge was 317 mg/day (SD=279) for primary agents but 371 mg/day (SD=348) with combinations included (Table 1) (t=5.92, df=348, p<0.0001). Discharge doses were also higher than initial doses (t=18.3, df=348, p<0.0001) but not significantly different from final doses in 1993 (t=1.85, df=646, p=0.08), although 24.8% greater than in 1989 (t=6.03, df=387, p<0.0001) (Table 1). However, the final total dose in 1998 was 29.3% greater than in 1993 (t=3.48, df=646, p<0.001) and 46.1% greater than in 1989 (t=2.56, df=397, p<0.02).
Discharge total doses were also 24.9% greater in men than women (mean=422 mg/day, SD=379, versus mean=338 mg/day, SD=323) (F=4.90, df=1, 347, p=0.03). However, 65 (47.1%) of the men were psychotic, whereas 101 (47.9%) of the women were affectively ill (χ2=6.64, df=1, p=0.04). By diagnosis, final total doses were ranked as follows: primary psychosis (mean=547 mg/day, SD=418), major affective disorder (mean=286 mg/day, SD=240), and other disorders (mean=194 mg/day, SD=209) (overall F=35.8, df=2, 346, p<0.0001). The final total dose fell somewhat with increasing age (rs=–0.22, N=349, p<0.001) and was higher in patients with ratings of moderate or major than in those with ratings of minor or no improvement (mean=423 mg/kg, SD=397, versus mean=329 mg/kg, SD=371) (F=2.95, df=1, 193, p=0.09) but was unrelated to longer hospitalization (rs=–0.08, N=349, p<0.14).
Since some factors may covary, multivariate analysis was applied. Four factors were associated with higher total discharge chlorpromazine-equivalent antipsychotic dose: psychotic versus major affective diagnosis (risk ratio=6.80, 95% CI=3.22–14.3), greater clinical improvement (risk ratio=3.36, 95% CI=1.65–6.84), use of two or more antipsychotics (risk ratio=1.94, 95% CI=1.14–3.22), and younger age (risk ratio=1.03, 95% CI=1.01–1.05). Discharge dose was no longer associated with sex, number of days in the hospital, primary agent typical versus atypical, use of depot neuroleptic, or use of a supplemental sedative.
Discussion
Over the past decade, atypical agents have emerged as the dominant choice among antipsychotics. At our hospital in 1993 (2), atypical agents accounted for only 12% of antipsychotics prescribed, compared with 72% in 1998 (Table 1). The most commonly used agents in 1998 were olanzapine, risperidone, and quetiapine (olanzapine was used more than risperidone, which was used as much as quetiapine), and atypical agents were used at similar rates across diagnostic groups. By multivariate analysis, total chlorpromazine-equivalent discharge doses were significantly higher for patients with psychotic diagnoses than those with major affective diagnoses, for those with greater clinical improvement during hospitalization (despite clinically individualized dosing), those prescribed multiple antipsychotics, and younger patients. Discharge doses were not significantly related to sex, hospital stay, typical/atypical antipsychotic type, or addition of sedatives. Total discharge chlorpromazine-equivalent antipsychotic doses increased by approximately 46% over the past decade.
It seems unlikely that increasing total doses of antipsychotics reflect major changes in admission policies or the impact of managed care. The length of stay did not decrease between 1993 and 1998 (range=19–29 days). Instead, increasing antipsychotic dosing appears to reflect use of moderate doses of individual agents but a rising cumulative total because of polypharmacotherapy. Simultaneous use of two or more antipsychotics was found in 55 (15.8%) of the patients in the 1998 study group at discharge, but in 133 (38.1%) at some time during hospitalization. The most frequent combinations involved typical antipsychotics added to atypical primary agents. This tendency may reflect incomplete confidence in monotherapy with atypical antipsychotic agents in inpatient practice. Additional combinations of several psychotropic agents also were common in 1998 (69 [19.8%] of the patients received four or more agents).
Polypharmacotherapy in major psychiatric disorders is a growing international phenomenon, despite lack of research evidence of superior effectiveness without compromising safety or acceptable financial cost (5–12). We conclude that upward trends in total antipsychotic dosing and growing use of different forms of polypharmacotherapy require additional empirical study with modern antipsychotic agents to evaluate critically their risks, benefits, and costs.
 |
Received Feb. 12, 2002; revision received May 7, 2002; accepted May 20, 2002. From the Department of Psychiatry and Neuroscience Program, Harvard Medical School, Boston; the Bipolar and Psychotic Disorders Program, McLean Hospital; the Department of Neuropsychiatry, Catholic University of Korea, College of Medicine, Seoul; and Bouvé College of Pharmacy and Allied Health Sciences, Northeastern University, Boston. Address reprint requests to Dr. Centorrino, Bipolar and Psychotic Disorders Clinic, North Belknap III, McLean Hospital, 115 Mill St., Belmont, MA 02478-9106; [email protected] (e-mail). Supported in part by NIMH grant MH-47370, an award from the Bruce J. Anderson Foundation, and the McLean Private Donors Neuropsychopharmacology Research Fund (Dr. Baldessarini).
1. Baldessarini RJ, Katz B, Cotton P: Dissimilar dosing with high-potency and low-potency neuroleptics. Am J Psychiatry 1984; 141:748-752Link, Google Scholar
2. Baldessarini RJ, Kando JC, Centorrino F: Hospital use of antipsychotic agents in 1989 and 1993: stable dosing with decreased length of stay. Am J Psychiatry 1995; 152:1038-1044Link, Google Scholar
3. Baldessarini RJ, Cohen BM, Teicher MH: Significance of neuroleptic dose and plasma level in the pharmacological treatment of psychoses. Arch Gen Psychiatry 1988; 45:79-91Crossref, Medline, Google Scholar
4. Baldessarini RJ, Tarazi FI: Drugs and the treatment of psychiatric disorders: antipsychotic and antimanic agents, in Goodman and Gilman’s The Pharmacological Basis of Therapeutics, 10th ed. Edited by Hardman JG, Limbird LE, Gilman AG. New York, McGraw-Hill, 2001, pp 485-520Google Scholar
5. Stahl SM: Antipsychotic polypharmacy: tips on use and misuse. J Clin Psychiatry 1999; 60:506-507Crossref, Medline, Google Scholar
6. Frye MA, Ketter TA, Leverich GS, Huggins T, Lantz C, Denicoff KD, Post RM: The increasing use of polypharmacotherapy for refractory mood disorders: 22 years of study. J Clin Psychiatry 2000; 61:9-15Crossref, Medline, Google Scholar
7. Wang PS, West JC, Tanielian T, Pincus HA: Recent patterns and predictors of antipsychotic medication regimens used to treat schizophrenia and other psychotic disorders. Schizophr Bull 2000; 26:451-457Crossref, Medline, Google Scholar
8. Procyshyn RM, Kennedy NB, Tse G, Thompson B: Antipsychotic polypharmacy: a survey of discharge prescriptions from a tertiary-care psychiatric institution. Can J Psychiatry 2001; 46:334-339Crossref, Medline, Google Scholar
9. Pearsall R, Glick ID, Pickar D, Suppes T, Tauscher J, Jobson KO: A new algorithm for treating schizophrenia. Psychopharmacol Bull 1998; 34:349-353Medline, Google Scholar
10. Zito JM: Pharmacoeconomics of the new antipsychotics for the treatment of schizophrenia. Psychiatr Clin North Am 1998; 21:181-202Crossref, Medline, Google Scholar
11. Hellewell JSE: Treatment-resistant schizophrenia: reviewing the options and identifying the way forward. J Clin Psychiatry 1999; 60(suppl 23):14-19Google Scholar
12. Rittmannsberger H, Meise U, Schauflinger K, Horvath E, Donat H, Hinterhuber H: Polypharmacy in psychiatric treatment: patterns of psychotropic drug use in Austrian psychiatric clinics. Eur Psychiatry 1999; 14:33-40Crossref, Medline, Google Scholar



