Abuse, Bullying, and Discrimination as Risk Factors for Binge Eating Disorder
Abstract
OBJECTIVE: This study examined whether sexual and physical abuse, bullying by peers, and ethnicity-based discrimination are associated with an increased risk for developing binge eating disorder in black women and in white women and whether any increase in risk is specific for the development of binge eating disorder. METHOD: A community sample of 162 women with binge eating disorder and 251 healthy and 107 psychiatric comparison subjects was interviewed for exposure to the risk factors under investigation. RESULTS: White subjects with binge eating disorder reported significantly higher rates of sexual abuse, physical abuse, bullying by peers, and discrimination than healthy comparison subjects. Only rates of discrimination were significantly higher in white women with binge eating disorder than in matched psychiatric comparison subjects. In black women with binge eating disorder, rates of sexual abuse, physical abuse, and bullying by peers—but not discrimination—were significantly higher than in healthy comparison women. Rates of sexual abuse were significantly higher in black women with binge eating disorder than in psychiatric comparison subjects. CONCLUSIONS: Consistent with previous research examining ethnicity-specific patterns of risk for psychiatric disorder, we found both ethnic similarities (physical abuse and bullying by peers) and differences (sexual abuse and discrimination) in the risk for binge eating disorder.
The role of sexual abuse as a risk factor for the development of eating disorders has been a source of considerable controversy, largely because of inconsistent findings (1). Conflicting results have been attributed to methodological limitations and differences across studies. Reviewing early studies on the relationship between sexual abuse and bulimia nervosa, Pope and Hudson (2) identified five methodological shortcomings: 1) inadequate comparison groups, 2) problematic sexual abuse definitions, 3) inadequate sexual abuse assessment, 4) inattention to the timing of abuse in relation to onset of bulimia nervosa, and 5) no psychiatric comparison groups, thus making an examination of specificity (i.e., whether the association is unique to bulimia nervosa) impossible. Also, Welch and Fairburn (3) noted an overreliance on patient samples, which likely resulted in an oversampling of individuals with a history of abuse (4).
A comprehensive review of studies that addressed these methodological concerns (5) concluded that childhood sexual abuse is a nonspecific risk factor for bulimia nervosa (i.e., abuse also increases risk for other mental disorders) and that the relationship of childhood sexual abuse to bulimia nervosa appears to be stronger than its association with anorexia nervosa. The authors hypothesized that binge eating may be an important strategy for coping with the aversive states that result from childhood abuse. This report uses data collected during a community-based study of risk factors for binge eating disorder in women to advance understanding of the relationship between childhood sexual abuse and eating disorders in three ways: by studying binge eating disorder, by including a sample of black women with binge eating disorder, and by integrating the study of sexual abuse with physical abuse and other abusive events.
Epidemiological studies suggest that binge eating disorder is more common than bulimia nervosa (6, 7) and represents a clinically significant syndrome (8, 9). To our knowledge, no study has examined the relationship between childhood sexual abuse and binge eating disorder as defined in DSM-IV with use of the methods recommended by Pope and Hudson (2). The present study replicates and extends the Oxford case-control studies of risk factors for the development of eating disorders (3, 10, 11).
Although epidemiological studies have found no differences in the prevalence of binge eating disorder across different ethnic groups (12, 13), most nonepidemiological studies of eating disorders have included only white participants. Ethnic minority populations are less likely than white populations to use mental health services and, consequently, are underrepresented in studies that rely on patient samples (9, 14, 15). Studies of mental health among ethnic minority groups are needed that focus on variation by ethnicity in the expression of disorders and on risk factors associated with these disorders (16). This report extends the investigation of binge eating disorder by including an ethnic minority group that appears to be as vulnerable to developing binge eating disorder as the white population (17).
Experts have urged researchers to comprehensively assess abusive experience in the study of risk factors for mental disorders (18). Research on the adverse mental health effects of childhood physical abuse has underscored its public health importance (18, 19). Physical bullying by peers is another form of abuse that is gaining attention, given data documenting its relationship to adverse mental health outcomes (20), including binge eating (21). Finally, studies of health and psychological problems among black Americans have identified discrimination based on ethnicity as an important ethnicity-specific risk factor (22, 23). The present study examined the contribution of four types of abusive experiences to risk for the development of binge eating disorder: childhood sexual abuse, physical abuse, bullying by peers, and discrimination.
A critical methodological consideration in the study of risk factors for mental disorders involves documenting the time sequence of the potential risk event and symptom onset. Distinguishing between risk factors versus correlates of psychiatric disorder requires that the risk variable occur before the onset of psychiatric symptoms (24, 25). Thus, the present study focused the assessment of abusive experiences on the time before onset of the eating disorder.
The present study examined in a community-based sample of black women and white women whether abusive experiences in childhood increase the risk of developing binge eating disorder and whether the increase in risk is specific to binge eating disorder or reflects a greater general risk for psychiatric disorder. Data about childhood sexual and physical abuse, bullying by peers, and discrimination were collected as part of a case-control study, the New England Women’s Health Project, designed to investigate risk factors for binge eating disorder in non-Hispanic black American and white American women.
As previously described in detail (8, 17), the New England Women’s Health Project recruited women aged 18 to 40 years from the general community in distinct geographic areas in Connecticut, New York City, and the greater Boston area. All women were told that the purpose of the study was to understand factors that might influence the development of an eating disorder; childhood abuse was not specifically referenced. A detailed examination of ethnic differences in the clinical presentation of binge eating disorder has been the subject of a previous report (9). Given significant differences in ethnic groups in the clinical presentation of binge eating disorder and in exposure to certain types of victimization (e.g., discrimination), the relationship between childhood abuse and the risk for binge eating disorder was examined separately for black and white women.
Method
Participants
The New England Women’s Health Project recruited three groups of women from the community who identified themselves as either white American or black American. The binge eating disorder group consisted of 60 black women (mean age=30.1 years, SD=5.8) and 102 white women (mean age=30.5 years, SD=5.8) who met DSM-IV criteria for current binge eating disorder. The highest education level among the black and white women with binge eating disorder was as follows, respectively: high school or less: 18.1%, 19.6%; some college: 50.0%, 35.5%; college graduate or beyond: 31.9%, 44.9% (χ2=10.69, df=2, p<0.005). Mean age at onset of binge eating disorder was 18.6 years (SD=8.5) for black women and 14.0 (SD=5.5) for white women (F=16.91, df=1, 160, p<0.0001, eta2=0.10). Two comparison groups were recruited from the same communities as the subjects with binge eating disorder and were individually matched to the women with binge eating disorder on ethnicity, age (within 2 years), and level of education. The healthy comparison group included 85 black women and 164 white women with no history of clinically significant eating disorder symptoms and no current psychiatric disorder. To increase statistical power, the healthy comparison group was oversampled when possible: 89 subjects with binge eating disorder had two matched comparison subjects, and 73 subjects with binge eating disorder had one matched healthy comparison subject. The psychiatric comparison group consisted of 21 black women and 86 white women with a current DSM-IV axis I psychiatric disorder but no history of clinically significant eating disorder symptoms. Using our matching criteria, we were able to locate only 107 psychiatric comparison subjects. For analyses comparing the psychiatric comparison group with the binge eating disorder group, only the 107 women with binge eating disorder who had a matched psychiatric comparison subject were included. Women in the psychiatric comparison group had the following diagnoses: mood disorder (N=53, 49.5%), anxiety disorder (N=47, 43.9%), substance disorder (N=4, 3.7%), body dysmorphic disorder (N=1, 0.9%), adjustment disorder (N=1, 0.9%), and psychotic disorder not otherwise specified (N=1, 0.9%).
Instruments and Procedure
As described further elsewhere (8), an initial telephone screening interview (participation rate: 91%) was administered in the New England Women’s Health Project to determine eligibility, identify potential subjects with binge eating disorder and comparison subjects, and collect, at the end of the screening interview, demographic information (by using questions about race or ethnicity consistent with questions from the U.S. Census Bureau) needed for matching. Eligible women were invited to complete a diagnostic and risk factor assessment interview (participation rates of black and white women, respectively: subjects with binge eating disorder: 84.8%, 85.2%; healthy comparison subjects: 62.7%, 74.5%; and psychiatric comparison subjects: 76.6%, 73.9%). The study protocol was approved by the institutional review boards of all participating institutions.
Diagnostic Assessment
Diagnoses were determined by using the Structured Clinical Interview for DSM-IV Axis I Disorders—Non-Patient Edition (26) and the Eating Disorder Examination (27), both standardized investigator-based interviews with well-established reliability and validity.
Assessment of Abusive Experiences
For determination of a history of abuse, the Oxford assessment (3) was used to incorporate the methodological recommendations of previous investigators (5, 28). Abuse was operationally defined and ascertained by interview, abuse assessment was embedded within a broader assessment of childhood experiences, and a personal timeline was established, with major life events (including onset of eating disorder) articulated and subsequent questions regarding life events cross-referenced with this timeline.
The definition of childhood sexual abuse was limited to sexual experiences involving physical contact with a family member or with a non-family-member 5 or more years older than the participant. Sexual abuse was categorized further as follows: repeated (any) sexual abuse, very severe sexual abuse (oral sex, anal sex, rape, or digital penetration), repeated very severe sexual abuse, and any sexual abuse by a family member. Childhood physical abuse was defined as any deliberate physical contact resulting in bruises or worse injuries. Physical abuse was coded further into the following categories: repeated (any) physical abuse, severe physical abuse (resulting in severe injuries, including those to the head or face, burns, or fractures), and repeated severe physical abuse. Physical bullying by peers was recorded if the participant had experienced physical threat of violence or actual physical harm by peers. All participants were asked whether they had encountered discrimination based on their ethnicity or race.
Coding for the four abuse categories was mutually exclusive. Specifically, if a bullying incident was racially motivated, it was coded under discrimination; if a participant was physically harmed during a sexual assault, the event was coded under sexual abuse. To ensure that the abuse preceded the eating disorder, participants were asked only about abusive experiences occurring before the onset of the first clinically significant and persistent symptomatic eating disorder behavior (e.g., regular episodes of overeating) or before age 18 years (whichever was earlier). Individuals in the comparison groups were questioned about the same age period as the subjects with binge eating disorder thereby matching for time of recall and for vulnerability to exposure.
Data Analysis
Chi-square analyses were used to examine the relationship between case status and the dichotomous abusive experiences. Fisher’s exact test was used when cell frequencies were below five. Odds ratios with 95% confidence intervals (CIs) were computed when significant relationships between variables were found.
Results
Subjects With Binge Eating Disorder Versus Healthy Comparison Subjects
For white women, any sexual abuse, repeated sexual abuse, and very severe sexual abuse were significantly more common among those with binge eating disorder than among healthy comparison women (Table 1). Repeated very severe sexual abuse was reported by more women with binge eating disorder, but the difference only approached statistical significance. Among those reporting a history of sexual abuse, women with binge eating disorder (N=10, 27.8%) were not significantly more likely than healthy comparison women (N=4, 20.0%) to have been abused by a family member (p=0.75, Fisher’s exact test). All physical abuse categories were reported by significantly more women with binge eating disorder than by healthy comparison women. White women with binge eating disorder also were significantly more likely than healthy comparison women to report a history of discrimination and bullying by peers.
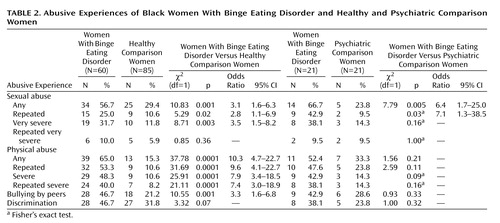
For black women, any sexual abuse, repeated sexual abuse, and very severe sexual abuse were more common among women with binge eating disorder than among the matched healthy comparison group (Table 2). The two groups did not differ significantly in exposure to repeated very severe sexual abuse. Of the black women who had a history of childhood sexual abuse, the subjects with binge eating disorder (N=7, 20.6%) were not significantly more likely than the healthy comparison women (N=7, 28.0%) to have been sexually abused by a family member (χ2=0.44, df=1, p=0.51). All categories of physical abuse were significantly more common among black women with binge eating disorder than among the healthy comparison women. Significantly more black women with binge eating disorder than healthy comparison women reported having been bullied by peers. Compared to healthy comparison women, more women with binge eating disorder reported discrimination experiences; however, this difference did not reach statistical significance (χ2=3.32, df=1, p=0.07).
Subjects With Binge Eating Disorder Versus Psychiatric Comparison Subjects
For white women, no significant differences were found between women with binge eating disorder and psychiatric comparison women in any sexual abuse category or in the rate of abuse by a family member (N=9, 28.1%, N=8, 34.8%, respectively) (χ2=0.28, df=1, p=0.60) (Table 1). Women with binge eating disorder and psychiatric comparison women did not differ significantly on any physical abuse category or on bullying. White women with binge eating disorder were significantly more likely than psychiatric comparison women to report discrimination.
Among black women, any sexual abuse and repeated sexual abuse were more common among women with binge eating disorder than among psychiatric comparison women (Table 2). The two groups did not differ significantly on rates of very severe or repeated very severe sexual abuse. Abuse committed by a family member was not significantly more likely among black women with binge eating disorder (N=2, 14.3%) than among psychiatric comparison women (N=0, 0.0%) (p=1.00, Fisher’s exact test). For each category of physical abuse and for discrimination or bullying by peers, higher rates were observed in women with binge eating disorder than among psychiatric comparison women, but these differences were not statistically significant.
Discussion
This study examined the relationship of abusive experiences in childhood to the development of binge eating disorder, a diagnosis in need of further study (13). Consistent with studies of the relationship between childhood sexual abuse and bulimia nervosa (5), our findings suggest an association between sexual abuse and binge eating disorder. In our community sample, more than one in three white women with binge eating disorder and more than one-half of the black women with binge eating disorder reported childhood sexual abuse. Our results are consistent with other studies (3, 10, 11, 29) that found that childhood sexual abuse is associated with an increased risk for eating disorders involving binge eating. Our study provides further evidence for the association between childhood sexual abuse and binge eating disorder and suggests that this finding is not limited to white women.
As articulated by Wyatt (30), ethnic differences in the impact of sexual abuse on risk for specific mental disorders need to be understood within the context of cultural and historical experiences of these ethnic groups in the United States, and some differential effects have already been demonstrated. For example, Roosa and colleagues (31) found that childhood sexual abuse was associated with an increased risk for depression in white women but not black women. As in previous studies of white women with bulimia nervosa, childhood sexual abuse did not appear to be associated uniquely with binge eating disorder; rather, it was associated with a greater risk for the development of psychiatric disorders in general. In contrast, for black women, childhood sexual abuse may be a specific risk factor for binge eating disorder. The rate of sexual abuse for black women with binge eating disorder was exceptionally high (66.7%), whereas the rate of sexual abuse in psychiatric comparison women (23.8%) was comparable to the rate reported by women in the healthy comparison group (29.4%). This ethnic difference was not hypothesized a priori, and our finding is based on a small sample because of the matching criteria used. Further study of the association between sexual abuse and binge eating disorder and its underlying mechanisms is needed to clarify the particular adjustment responses to abusive experiences in childhood across ethnic groups.
Our study expanded on previous research by including assessments of physical abuse, bullying, and discrimination in women with binge eating disorder. Alarmingly high rates of physical abuse were found among white women (49.0%) and black women (65.0%) with binge eating disorder, and for many women (31.4% white and 40.0% black), physical abuse was repeated and severe. In black and white women with binge eating disorder, physical abuse at all severity levels was significantly more common than in the matched healthy comparison groups. Moreover, having been bullied by peers was associated significantly with binge eating disorder in both ethnic groups, consistent with the results of a survey of secondary school students (21) that found that binge eating was associated with bullying by peers. In both ethnic groups, childhood physical abuse and bullying by peers were found to be associated with general risk for the development of mental disorders rather than representing unique risk factors for the development of binge eating disorder. It is of note that Roosa and colleagues (31) found that physical abuse and depression were associated significantly across ethnic groups, suggesting that cultural factors influencing the adverse impact of physical abuse on mental health may be similar for black and white women. These findings could be extended in a number of ways, including to studies that examine the particular significance of the role of the relationship between the perpetrator and victim on the impact of abuse across ethnic groups.
Although many black women in our sample reported discrimination, our results suggest that self-reported discrimination is neither a specific nor a general risk factor for binge eating disorder among black women. When one considers the rate of discrimination observed in this sample, it is important to keep in mind that assessment of exposure was limited to the time before the onset of disordered eating or age 18 years. As expected, few white women reported discrimination based on ethnicity; unexpectedly, however, white women with binge eating disorder were significantly more likely to report discrimination than healthy comparison or psychiatric comparison women. Inspection of the reasons provided by white participants suggests that physical features stereotypically associated with belonging to a particular ethnic group were identified as the reasons for being the target of discrimination. In contrast, the attributions of black women regarding discrimination were focused on their membership in a minority group. This illustrates the centrality of attribution in self-report of exposure to discrimination incidents (22). Consistent with retrospective studies that have found that teasing about weight is a risk factor for the development of bulimia nervosa (10), we hypothesize that, for white women, being mistreated because of physical attributes may contribute uniquely to the risk of developing an eating disorder.
Our study had several strengths. Our sample included a large number of black women; healthy and psychiatric comparison subjects were recruited from the same communities as the subjects with binge eating disorder and were matched for relevant characteristics. Diagnostic status and history of abuse were determined by using state-of-the-art interviews rather than self-report questionnaires. Analyses focused on abusive experiences before the onset of disordered eating. A psychiatric comparison group was included to examine whether risk arising from childhood abuse is specific to the development of binge eating disorder. Finally, by adopting the design of the Oxford studies, we minimized the chance that differences in results across studies could be due to differences in methodology.
There were also several limitations. First, as in all previous studies of abuse and full-syndrome eating disorders, exposure to childhood abuse was determined retrospectively. Such data do not permit causal inferences (25) and are subject to recall bias. Individuals with psychiatric disorders may be more likely to report exposure to events that they perceive as causing their disorder. Psychiatric treatment may render individuals more comfortable with reporting abusive experiences, potentially resulting in higher rates of abuse in the binge eating disorder or psychiatric comparison groups than in the healthy comparison groups. This specific form of bias was probably not a major influence in our study as few of our participants reported having received psychiatric treatment (9). Second, interviewers were not blind to the participants’ diagnostic status. To minimize this potential problem, interviewers were blind to the study hypotheses, and they were carefully trained and supervised to ensure standard administration of the interview. Third, our psychiatric comparison groups were composed of individuals with various psychiatric disorders. It is unlikely that the particular mix of disorders represented in our psychiatric comparison groups would be easily replicated, and it is possible that the heterogeneity of the psychiatric comparison groups would affect the exposure rates reported in these groups. The study was not designed to permit conclusions about specific risk factors for disorders other than binge eating disorder; however, the psychiatric comparison groups should have provided a good representation of general risk factors across psychiatric disorders. Among black women, comparisons of the binge eating disorder and psychiatric comparison groups were limited because of the small number of suitable psychiatric comparison subjects. The costs involved in establishing a community-based sample of black women (who represent less than 20% of the population in the communities where this study was conducted) pose a considerable challenge to researchers who need to find specific matched subsamples. Fourth, for pragmatic reasons, the study was limited to non-Hispanic white and black women. Recent studies have shown that other ethnic minority populations also experience eating disturbances (32), and future studies of these groups are needed. Finally, we caution that carefully designed observational studies are needed to test the hypothesis that abusive childhood experiences represent causal risk factors for the development of eating disorders and to elucidate more specifically the potential causal mechanisms underlying the associations observed in the present study. Of importance, such research needs to measure prospectively (and repeatedly) exposure to risk and onset of eating disorder symptoms, thus permitting both careful monitoring of the key variables of interest and delineation of the temporal ordering of the hypothesized causal variables relative to the outcomes of interest. Moreover, such studies need to anticipate the possibility that abusive experiences may be markers rather than causal factors for the development of eating disorders by assessing exposure to other potential causal risk factors (e.g., genetic vulnerability factors and familial factors) that may also be associated with abusive experiences.
 |
 |
Received May 8, 2001; revisions received Dec. 14, 2001, and May 9, 2002; accepted June 27, 2002. From the Department of Psychology, Wesleyan University. Address reprint requests to Dr. Striegel-Moore, Department of Psychology, Wesleyan University, 207 High St., Middletown, CT 06459; [email protected] (e-mail). Supported by NIMH grant MH-52348 (to Dr. Striegel-Moore) and by a supplemental grant from the Office for Research on Women’s Health at NIH. Dr. Fairburn is supported by a Principal Fellowship from the Wellcome Trust (046386). The authors thank Dr. Sarah Welch for assisting Dr. Christopher Fairburn in providing training on the Eating Disorder Examination and Risk Factors Interview and Mimi Gibbon for providing initial training on the Structured Clinical Interview for DSM-IV and annual retraining workshops.
1. Kearney-Cooke A, Striegel-Moore RH: Treatment of childhood sexual abuse in anorexia nervosa and bulimia nervosa: a feminist psychodynamic approach. Int J Eat Disord 1994; 15:305-319Crossref, Medline, Google Scholar
2. Pope HG Jr, Hudson JI: Is childhood sexual abuse a risk factor for bulimia nervosa? Am J Psychiatry 1992; 149:455-463Link, Google Scholar
3. Welch SL, Fairburn CG: Childhood sexual and physical abuse as risk factors for the development of bulimia nervosa: a community-based case-control study. Child Abuse Negl 1996; 20:633-642Crossref, Medline, Google Scholar
4. Walker EA, Unutzer J, Rutter C, Gelfand A, Saunders K, VonKorff M, Koss MP, Katon W: Costs of health care use by women HMO members with a history of childhood abuse and neglect. Arch Gen Psychiatry 1999; 56:609-613Crossref, Medline, Google Scholar
5. Wonderlich SA, Brewerton TD, Jocic Z, Dansky BS, Abbott DW: Relationship of childhood sexual abuse and eating disorders. J Am Acad Child Adolesc Psychiatry 1997; 36:1107-1115Crossref, Medline, Google Scholar
6. Gotesman KG, Agras WS: General population-based epidemiological study of eating disorders in Norway. Int J Eat Disord 1995; 18:119-126Crossref, Medline, Google Scholar
7. Hay P: The epidemiology of eating disorder behaviors: an Australian community-based survey. Int J Eat Disord 1998; 23:371-382Crossref, Medline, Google Scholar
8. Pike KM, Dohm FA, Striegel-Moore RH, Wilfley DE, Fairburn CG: A comparison of black and white women with binge eating disorder. Am J Psychiatry 2001; 158:1455-1460Link, Google Scholar
9. Wilfley DE, Pike KM, Dohm FA, Striegel-Moore RH, Fairburn CG: Bias in binge eating disorder: how representative are recruited clinical samples? J Consult Clin Psychol 2001; 69:383-388Crossref, Medline, Google Scholar
10. Fairburn CG, Welch SL, Doll HA, Davies BA, O’Connor ME: Risk factors for bulimia nervosa: a community-based case-control study. Arch Gen Psychiatry 1997; 54:509-517Crossref, Medline, Google Scholar
11. Fairburn CG, Doll HA, Welch S, Hay PJ, Davies BA, O’Connor ME: Risk factors for binge eating disorder: a community-based, case-control study. Arch Gen Psychiatry 1998; 55:425-432Crossref, Medline, Google Scholar
12. Spitzer RL, Devlin M, Walsh BT, Hasin D, Wing R, Marcus M, Stunkard A, Wadden T, Yanovski S, Agras S, Mitchell J, Nonas C: Binge eating disorder: a multisite field trial of the diagnostic criteria. Int J Eat Disord 1992; 11:191-203Crossref, Google Scholar
13. Smith DE, Marcus MD, Lewis CE, Fitzgibbon M, Schreiner P: Prevalence of binge eating disorder, obesity, and depression in a biracial cohort of young adults. Ann Behav Med 1998; 20:227-232Crossref, Medline, Google Scholar
14. Pincus HA, Zarin DA, Tanielian TL, Johnson JL, West JC, Pettit AR, Marcus SC, Kessler RC, McIntyre JS: Psychiatric patients and treatments in 1997: findings from the American Psychiatric Practice Research Network. Arch Gen Psychiatry 1999; 56:441-449Crossref, Medline, Google Scholar
15. Weinick RM, Krauss NA: Racial/ethnic differences in children’s access to care. Am J Public Health 2000; 90:1771-1774Crossref, Medline, Google Scholar
16. Vega W, Rumbaut R: Ethnic minorities and mental health. Annu Rev Sociol 1991; 17:351-383Crossref, Google Scholar
17. Striegel-Moore RH, Wilfley DE, Pike KM, Dohm FA, Fairburn CG: Recurrent binge eating in black American women. Arch Fam Med 2000; 9:83-87Crossref, Medline, Google Scholar
18. Gorey KM, Leslie DR: The prevalence of child sexual abuse: integrative review adjustment for potential response and measurement biases. Child Abuse Negl 1997; 21:391-398Crossref, Medline, Google Scholar
19. Becker JV, Alpert JL, BigFoot DS, Bonner BL, Geddie LF, Henggeler SC, Kaufman KL, Walker CE: Empirical research on child abuse treatment. J Clin Child Psychol 1995; 24(suppl):23-46Google Scholar
20. Nansel TR, Overpeck M, Pilla RS, Ruan WJ, Simons-Morton B, Scheidt P: Bullying behaviors among US youth: prevalence and association with psychosocial adjustment. JAMA 2001; 285:2094-2100Crossref, Medline, Google Scholar
21. Kaltiala-Heino R, Rissanen A, Rimpela M, Rantanen P: Bulimia and bulimic behaviour in middle adolescence: more common than thought? Acta Psychiatr Scand 1999; 100:33-39Crossref, Medline, Google Scholar
22. Clark R, Anderson NB, Clark VR, Williams DR: Racism as a stressor for African Americans: a biopsychosocial model. Am Psychol 1999; 54:805-816Crossref, Medline, Google Scholar
23. Contrada RJ, Ashmore RD, Gary ML, Coups E, Egeth JD, Sewell A, Ewell K, Goyal TM, Chasse V: Ethnicity-related sources of stress and their effects on well-being. Current Directions in Psychol Sci 2000; 9:136-139Crossref, Google Scholar
24. Kraemer HC, Kazdin AE, Offord DR, Kessler RC, Jensen PS, Kupfer DJ: Coming to terms with the terms of risk. Arch Gen Psychiatry 1997; 54:337-343Crossref, Medline, Google Scholar
25. Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D: How do risk factors work together? mediators, moderators, and independent, overlapping, and proxy risk factors. Am J Psychiatry 2001; 158:848-856Link, Google Scholar
26. First MB, Spitzer RL, Gibbon M, Williams JB: Structured Clinical Interview for DSM-IV Axis I Disorders—Non-Patient Edition (SCID-I/NP), version 2.0. New York, New York State Psychiatric Institute, Biometrics Research, 1996Google Scholar
27. Fairburn CG, Cooper Z: The Eating Disorder Examination, 12th ed, in Binge Eating: Nature, Assessment and Treatment. Edited by Fairburn CG, Wilson GT. New York, Guilford, 1993, pp 317-360Google Scholar
28. Wyatt GE, Peters SD: Methodological considerations in research on the prevalence of child sexual abuse. Child Abuse Negl 1986; 10:241-251Crossref, Medline, Google Scholar
29. Fleming J, Mullen PE, Sibthorpe B, Bammer G: The long-term impact of childhood sexual abuse in Australian women. Child Abuse Negl 1999; 23:145-159Crossref, Medline, Google Scholar
30. Wyatt GE: The sociocultural context of African American and white American women’s rape. J Soc Issues 1992; 48:77-91Crossref, Google Scholar
31. Roosa MW, Reinholtz C, Angelini PJ: The relation of child sexual abuse and depression in young women: comparisons across four ethnic groups. J Abnorm Child Psychol 1999; 27:65-76Medline, Google Scholar
32. Smolak L, Striegel-Moore RH: Challenging the myth of the golden girl, in Eating Disorders. Edited by Striegel-Moore RH, Smolak L. Washington, DC, American Psychological Association, 2001, pp 111-132Google Scholar



