Incidence and Prediction of Posttraumatic Stress Disorder Symptoms in Severely Injured Accident Victims
Abstract
OBJECTIVE: This study was designed to assess the incidence of posttraumatic stress disorder (PTSD) in severely injured accident victims and to predict the presence of PTSD symptoms at a 12-month follow-up. METHOD: A longitudinal, 1-year follow-up study was carried out with 106 consecutive patients with severe accidental injuries who were admitted to the trauma surgeons’ intensive care unit at a university hospital. Patients were interviewed within 1 month and 12 months after the accident. Assessments included an extensive clinical interview, the Impact of Event Scale, the Clinician-Administered PTSD Scale, the Sense of Coherence questionnaire, and the Freiburg Questionnaire of Coping With Illness. RESULTS: A total of 13.4 days (SD=6.6) after the accident, five patients (4.7%) met all criteria for PTSD with the exception of the time criterion. A total of 22 other patients (20.8%) had subsyndromal PTSD. At the 1-year follow-up, two patients (1.9%) had PTSD, and 13 (12.3%) had subsyndromal PTSD. Multiple regression analysis explained 34% of the variance of PTSD symptoms 12 months after the accident. Biographical risk factors, the sense of a death threat, symptoms of intrusion, and problem-oriented coping each contributed significantly to the predictive model. CONCLUSIONS: In severely injured accident victims who were healthy before experiencing trauma, the incidence of PTSD was low. One-third of the variance of PTSD symptoms at 1-year follow-up could be predicted by mainly psychosocial variables.
In 1866, Erichsen (1) described a syndrome consisting of cognitive impairments and psychosomatic symptoms that occurred in survivors of railway accidents. Erichsen’s “railway spine” can be regarded as one of the roots of modern psychotraumatology. Despite this, the psychosocial effects of accidental injuries have not yet been studied thoroughly, so epidemiological data are still inconsistent. This might be because some accidents, traffic accidents in particular, are viewed by society as such routine occurrences that they are no longer considered to be “an event that is outside the range of usual human experience” (DSM-III-R). However, an epidemiological study on the frequency and psychological impact of 10 potentially traumatic events (2) found motor vehicle accidents to present the most adverse combination of frequency and impact.
During the first few hours and days following an accidental injury, most patients have at least short periods in which they feel anxious or worried; dissociative symptoms such as derealization may occur in about 15% of patients but are usually of short duration (3, 4). Over the following weeks and months, the rates of posttraumatic stress disorder (PTSD) reported in the literature range from 8% (5) to 39% (6). More recent publications report that 32%–34% of patients suffer from PTSD after traffic accidents (7, 8). Only a few long-term follow-up studies have been carried out so far, reporting psychiatric morbidity (mostly depressive disorders) in 22% of accident victims over an observation period of 28 months (9) and PTSD in 8% 5 years after the accident (10). The prevalence of PTSD with delayed onset remains unclear, although cases with a delayed onset of up to 4 years have been reported (11).
Most of the samples of accident victims investigated to date have consisted of a mixture of patients with injuries of varying severity (12). A homogenous sample of exclusively severely injured patients has, to our knowledge, never been used. The present study, therefore, was aimed at assessing the incidence of PTSD in a group of accident victims who sustained severe physical trauma and met the stressor criterion according to DSM-IV, thus qualifying for a possible diagnosis of PTSD. Second, we tried to establish a predictive model for early identification of persons at risk for developing PTSD symptoms.
Method
Participants
All participants had sustained accidental injuries that caused a life-threatening or critical condition requiring their referral to the intensive care unit of the Traumatology Department at the University Hospital of Zurich (13). An Injury Severity Score (14) of 10 or more and a Glasgow Coma Scale (15) score of 9 or more were required for inclusion, thus excluding all patients with severe head injuries. Furthermore, patients had to be 18–70 years of age and capable with regard to both their clinical condition and fluency in German to take part in an extensive interview within 1 month of the accident. Patients suffering from any serious somatic illness or who had been under treatment for any mental disorder immediately before the accident and/or those who showed marked clinical signs or symptoms of mental disorders that were obviously unrelated to the accident were excluded. This way, 16 patients were excluded because of the presence of preexisting psychiatric pathology. In addition, all patients who sustained their injuries as a result of a suicide attempt or from a physical attack were excluded from the study.
During a recruitment period of 18 months, all patients in the intensive care unit were consecutively screened: 135 patients were deemed eligible for inclusion in the study. After the study was completely described to the subjects, written informed consent was obtained from 121 patients (time 1); 14 of 135 (10.4%) refused to participate. Follow-up interviews were performed 12 months (plus or minus 3 weeks) after the trauma (time 2). Fifteen out of 121 patients (12.4%) were lost during the follow-up period. Thus, the final group for which we had complete longitudinal data consisted of 106 patients.
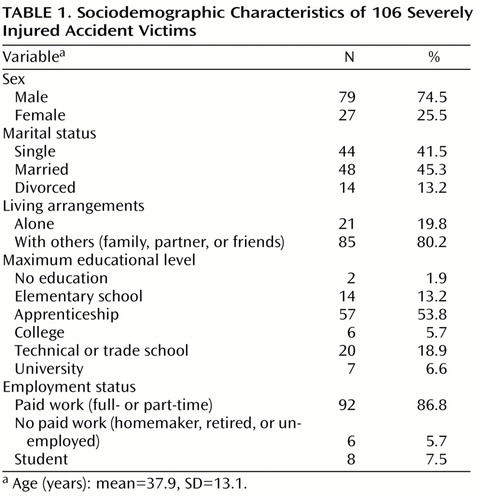
The sociodemographic characteristics of the group are presented in Table 1. Traffic accidents were most frequent (N=64 patients, 60.4%), followed by severe sports and leisure time accidents (N=23, 21.7%), accidents in the workplace (N=13, 12.3%), and household accidents (N=6, 5.7%). No significant differences in injury severity (Injury Severity Score) were found between these four types of accidents (F=0.19, df=3, 102, p=0.90). According to the surgeons’ files, 40 patients (37.7%) suffered from retrograde amnesia; 44 patients (41.5%) sustained a traumatic brain injury, i.e., they had objectively reported loss of consciousness and/or pathological findings were revealed by a cranial computerized tomograph scan. A significant association was found between retrograde amnesia and traumatic brain injury (Pearson’s χ2=21.5, df=1, p<0.001).
The patients who refused to participate in the study (14 out of 135 eligible patients, 10.4%) did not differ significantly from the final study group with regard to sex, age, Injury Severity Score or Glasgow Coma Scale scores. However, significantly more work-related accidents were found among those refusing to participate (refusers: N=7, 50%; remainder of study group: N=13, 12.3%) (p<0.01, Fisher’s exact test). Therefore, the patients in the study group who had sustained accidents in the workplace (N=13, 12.3%) were compared to the rest of the group with regard to PTSD symptom profiles by means of the Clinician-Administered PTSD Scale. However, no significant differences were found between groups (mean total score=24.5 versus 18.1, respectively) (t=–1.32, df=104, p=0.19). Furthermore, the 15 dropouts did not differ significantly from the final study group with regard to sociodemographic characteristics, accident-related variables, or measures of postaccident psychopathology.
Measures
The mean length of stay at an intensive care unit was 5.5 days (SD=5.0, range=1–26). The mean number of days between the accident and initial assessment (time 1) was 13.4 (SD=6.6, range=3–29). All interviews were conducted by a medical doctor, a clinically experienced internist who had been involved in research for a number of years and was thoroughly trained in the specifics of traumatic stress research. All patients to whom the exclusion criterion “preexisting psychiatric pathology” was potentially applicable were discussed in detail by the interviewer and Dr. Schnyder before any decision about inclusion was made.
Posttraumatic psychological symptoms were assessed by using the Impact of Event Scale (16), a 15-item questionnaire comprising two subscales (intrusion and avoidance), with high reliability and validity as a screening instrument for PTSD (17). Furthermore, the Clinician-Administered PTSD Scale (18) was administered; this instrument allows quantification of the frequency plus intensity of each of the 17 PTSD symptoms per DSM-III-R. The Clinician-Administered PTSD Scale has excellent psychometric properties (19).
Information about the patients’ social network and recent life events was gathered by using a 39-item questionnaire compiled from a revised version of the Social Network Index (20), an adapted version of the Social Support Questionnaire (21) and the Inventory for Determining Life-Changing Events (22). Biographical protective and risk factors for the development of psychological and psychosomatic disorders were determined by using a compilation of scientifically established factors (23). The Sense of Coherence questionnaire (24) is a measure of an individual’s resilience to stress and his or her capacity to cope with it. Individuals with high Sense of Coherence questionnaire scores are likely to perceive stressors as predictable and explicable, have confidence in their capacity to overcome stressors, and judge it worthwhile to rise to the challenges they face. Test properties such as test-retest reliability and internal consistency of the Sense of Coherence questionnaire scale are excellent (25). The Freiburg Questionnaire of Coping With Illness (26) is a coping questionnaire that includes five subscales: depressive reaction; active, problem-oriented coping; distraction and enhancement of self-esteem; religiosity and the search for meaning; and downplaying and wishful thinking.
The Impact of Event Scale, Sense of Coherence questionnaire, and Freiburg Questionnaire of Coping With Illness are self-rating scales. Data on the patients’ social network, life events, biographical protective and risk factors, and scores on the Clinician-Administered PTSD Scale were gathered during the clinical interview. Internal consistencies of the instruments used in this study were comparable to those reported in the literature. Cronbach’s alpha was 0.89 for the Impact of Event Scale, 0.90 for the Sense of Coherence questionnaire, 0.46–0.73 for the five Freiburg Questionnaire of Coping With Illness scales, and 0.71 for the Clinician-Administered PTSD Scale. The patients with retrograde amnesia scored extremely high on item 7 (psychogenic amnesia) of the Clinician-Administered PTSD Scale. Being unable to differentiate organic from psychogenic amnesia, we decided to omit item 7 in all further calculations. This procedure resulted in an increase in Cronbach’s alpha from 0.71–0.77 at time 1 and from 0.79–0.86 at time 2. At the end of the initial interview, patients were asked to make a subjective appraisal of the severity of the accident by using a Likert scale ranging from “1=very slight” to “5=very severe.”
Predictive Model and Statistical Analyses
For the establishment of a stable regression model predicting PTSD symptom profiles at the 12-month follow-up, a selection of 10 potential predictor variables, all assessed at measurement point time 1, was made on the basis of both “pathogenic” and “salutogenic” considerations (24): Injury Severity Score was chosen as the only objective accident-related variable. Sex was included because, in general, PTSD is more likely to develop in women than in men after exposure to a traumatic event (27). Biographical risk factors and stress due to life events were selected as potential pretraumatic risk factors. Furthermore, the patients’ subjective view was represented in the model by their appraisals of the severity and threat of the accident. Early posttraumatic psychopathology was entered into the equation by use of the Impact of Event Scale intrusion subscale score; salutogenic aspects were represented by the Sense of Coherence questionnaire score and the patients’ social network. Finally, the Freiburg Questionnaire of Coping With Illness subscale score for active, problem-oriented coping was included because such coping strategies were most frequently used in our study group and also because the literature on the adaptivity of active coping strategies is still controversial (28, 29).
Linear multiple regression analysis was used for the prediction of PTSD symptoms (Clinician-Administered PTSD Scale total score) at the 1-year follow-up. Assumptions of multiple regression analysis include normality, linearity, and homoscedasticity between predicted dependent variable scores and errors of prediction (30). No violation of assumptions was found after performance of a logarithmic data transformation (log [x + 1]) of the positively skewed Clinician-Administered PTSD Scale total score. The Kolmogorov-Smirnov goodness-of-fit test showed that residuals were normally distributed (Kolmogorov-Smirnov Z=0.55, p>0.25). In addition, tolerances larger than 0.67 for all predictor variables indicated low multicollinearity. Therefore, the predictors are almost independent, and a stable estimation of beta coefficients in the regression analysis can be assumed.
Results
Descriptive Data
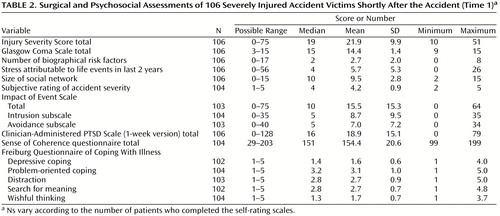
Surgical and psychosocial assessments at measurement point time 1 (shortly after the accident) are presented in Table 2. A mean Injury Severity Score of 21.9 indicates that patients were severely injured. Fifteen patients (14.2%) had a Glasgow Coma Scale score of 9–13, indicating moderate traumatic brain injury; the Glasgow Coma Scale score was 14 in five patients (4.7%) and 15 in 86 patients (81.1%). Twenty-six patients (24.5%) had experienced a sense of a death threat during the accident. Patients with retrograde amnesia did not differ significantly from the rest of the group with regard to Clinician-Administered PTSD Scale mean scores (time 1: 16.4 versus 20.4, respectively, t=1.32, df=104, p=0.19; time 2: 11.7 versus 14.3, t=0.84, df=104, p=0.40). Also, patients with traumatic brain injury did not differ significantly from the rest of the group with regard to Clinician-Administered PTSD Scale mean scores (time 1: 18.6 versus 19.0, t=0.14, df=104, p=0.89; time 2: 12.9 versus 13.6, t=0.24, df=104, p=0.81).
Shortly after the accident (time 1), five patients (4.7%) met all criteria for PTSD with the exception of the time criterion. In accordance with the criteria of other authors (6, 31), patients were diagnosed with subsyndromal PTSD if they met the symptomatic criteria for criterion B (DSM-III-R) plus either C or D but not C and D. Twenty-two patients (20.8%) had subsyndromal PTSD at time 1. At the 1-year follow-up (time 2), two patients (1.9%) had PTSD, and 13 (12.3%) had subsyndromal PTSD.
The longitudinal course of the cases of PTSD and subsyndromal PTSD is visualized in Figure 1. The decrease in the number of patients meeting the criteria for subsyndromal or full-blown PTSD was statistically significant (exact p<0.05, McNemar test). None of the five patients who met all criteria for PTSD, with the exception of the time criterion, shortly after the accident had full-blown PTSD at the 1-year follow-up. Nevertheless, a significant association between the two measurement points was found regarding diagnosis (subsyndromal or full-blown PTSD versus no PTSD) (p<0.01, Fisher’s exact test).
Prediction of PTSD Symptoms at 12-Month Follow-Up
Except for the Injury Severity Score (r=–0.02), all potential predictor variables correlated significantly with the Clinician-Administered PTSD Scale total score at the 12-month follow-up. Intercorrelations of predictor variables were mainly near zero or in the low range (r=0.10–0.29). It is of importance that the Injury Severity Score did not correlate significantly with the patients’ subjective appraisals of the event (death threat: r=0.07, accident severity: r=–0.07).
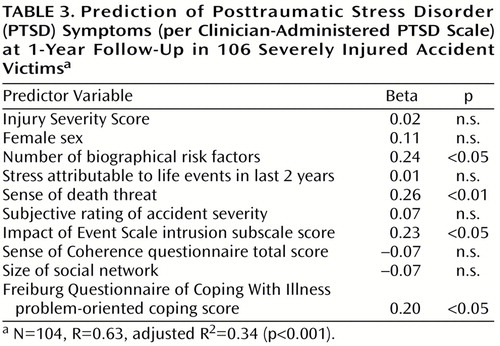
In multiple regression analysis, 34% of the variance of PTSD symptom profiles 12 months after the accident could be explained by means of 10 predictor variables. Out of these, four variables, namely biographical risk factors, sense of a death threat, the Impact of Event Scale intrusion subscale score, and problem-oriented coping, contributed significantly to the predictive model (Table 3).
Discussion
To the best of our knowledge, this is the first study to examine a group exclusively comprising accident victims who received severe, life-threatening injuries. Our aim was to collect as homogeneous a group as possible, with patients free from mental disturbances attributable to severe head injuries. Furthermore, patients were excluded if they showed any signs of prior psychological problems. The exclusion of patients who had attempted suicide or had been exposed to a physical assault further contributed to the homogeneity of the group.
Although all patients sustained severe physical trauma and met the stressor criterion A1 per DSM-IV, only 26 had actually experienced the sense of a death threat during the accident. It must be assumed that many patients in this group, particularly those with retrograde amnesia, did not fulfill stressor criterion A2 and thus, strictly speaking, did not qualify for a possible diagnosis of PTSD. This is a problem that occurs in all studies of accident survivors, particularly in patients with severe physical trauma.
The literature on the development of PTSD after traumatic brain injury is still quite controversial: although some authors found that brief unconsciousness and consecutive amnesia may protect against the development of PTSD (32, 33), others reported substantial prevalences of PTSD after mild or even severe head injuries (34–36). Our data revealed somewhat lower Clinician-Administered PTSD Scale scores for patients with retrograde amnesia and traumatic brain injury, but the differences were not statistically significant. Therefore, we decided not to analyze these groups separately.
Contrary to the handling of other groups that were drawn from accident victims seeking treatment for their posttraumatic psychological problems, our study group was collected consecutively, with a trauma surgeon’s intensive care unit as the single source. In traumatic stress studies, it is particularly important to achieve high response rates because reluctance to participate in an interview focusing on the trauma might be a symptom of avoidance and thus indicate the possible presence of PTSD (37). In our study, 10.4% refused to participate. Compared to findings in the literature, this is an unusually low rate. In the studies of accident victims that we examined, if mentioned at all, the refusal rate was substantially higher (6, 8).
After we took into account the seriousness of the accidents and related injuries, we found that the number of patients with PTSD or subsyndromal PTSD was substantially lower than would have been expected from the current literature. We think that this finding is primarily due to a strict selection process that probably excluded most patients with pretraumatic psychiatric problems. Other authors have reported a much higher incidence of posttraumatic psychopathology in accident victims. For example, Blanchard et al. (6) found that 39% of their group had PTSD and another 29% had subsyndromal PTSD 1–4 months postaccident. However, the group studied by these researchers was recruited by referrals from medical practitioners and by “local media coverage and advertising,” and women comprised 68% of the group, which is not typical for accident victims. It is well known that women have approximately twice the risk of men of developing PTSD (27, 38). Therefore, a sampling bias with regard to gender must almost necessarily have led to excessively high PTSD rates in the Blanchard et al. study. More recently, Koren et al. (7) reported that 32% of accident victims with mild to moderate physical injuries suffered from PTSD; unfortunately, the authors did not specify their sampling method. Similarly, Ursano et al. (8) found that 34% of the victims of serious motor vehicle accidents had PTSD 1 month later. However, this group was recruited from a trauma center and local police reports. Refusal to participate ranged from 50% to 75% depending on where the patients were recruited from, and women comprised 48% of the final group; therefore, it remains unclear for which population this group can be regarded as representative.
Our findings are more in accordance with those of Malt (9), who investigated the only truly randomized sample of accident victims published so far, to our knowledge, and found that only one out of 107 patients was suffering from PTSD. It must be emphasized, however, that in the Malt study diagnoses were made on the basis of thoroughly conducted clinical interviews and not on standardized questionnaires such as the Clinician-Administered PTSD Scale.
The highly significant predictive value of the patients’ sense of threat to their lives during the incident lends support to the findings of other authors who found that the subjective appraisal of the trauma was highly predictive of the later development of psychological problems, including PTSD (3, 39). It should be pointed out that in our study the subjective appraisal variables were unrelated to Injury Severity Scores. This underlines once again the importance of the patients’ subjective appraisals in the development of posttraumatic psychological problems (3).
A similar predictive power was found for the biographical risk factors for the development of psychological and psychosomatic disorders. To our knowledge, no comparison data are available in the literature. Given the simple methodological level of the assessment, the importance of this variable should not be overestimated. Nevertheless, our results indicate that pretraumatic characteristics may have an influence on the development of PTSD symptoms after a serious accident.
It is no surprise that early symptoms of reexperiencing, as assessed with the Impact of Event Scale intrusion subscale, play an important role in this predictive model. The predictive value of the Impact of Event Scale has been demonstrated in numerous traumatic stress studies and has also been confirmed with accident victims (40, 41).
Although when patients have chronic health problems, active, problem-oriented coping strategies are seen as adaptive, this is apparently not the case in the acute phase after a serious accident. Our findings in this regard are in accordance with those of Malt (28), who suggests that at least in the acute treatment phase, an all-too-active tackling of the problem may be maladaptive.
A predictive model that explains 34% of the variance in PTSD symptoms 12 months after an accident is not a strong one. The computation of predictors in a group with low posttraumatic morbidity can only yield results that must be interpreted with great caution. However, other authors did not find substantially stronger models (39, 42, 43). When we take into account that our predictive model spans a period of 12 months, this may be what can realistically be expected, namely that the psychosocial variables assessed account for about one-third of the variance of PTSD symptoms.
This study has a number of limitations. First, patients were excluded from the study if they did not speak German sufficiently. Proficiency in the official language of a country is a strong determinant of social integration; patients with poor social integration may have had greater than average difficulties dealing with the consequences of their accident. In future studies, patients whose mother tongue is other than the country’s official language should be included with the use of interpreters. Second, we did not use a structured diagnostic interview for identifying preexisting psychiatric pathology. Had we done so, we would not have solved properly the methodological problem of retrospectively assessing pretraumatic psychopathology in the immediate posttraumatic stage. It is possible that some patients suffered from mental disorders before their accident. Therefore, preexisting psychopathology cannot be excluded as an etiologic factor for the development of PTSD in this group. Furthermore, the missing correlation between injury severity and PTSD symptom level may be at least in part due to a statistically restricted range phenomenon: it is possible that in a study including mild, moderate, and severe injuries, thus covering the full range of Injury Severity Score values, the correlation between Injury Severity Score and Clinician-Administered PTSD Scale score would become statistically significant. Finally, because patients with work-related accidents more frequently refused participation and tended to show more posttraumatic stress symptoms, they should be studied more thoroughly. The small number of patients with work-related accidents in our group did not allow us to draw any firm conclusions regarding their symptoms.
 |
 |
 |
Presented at the Sixth European Conference on Traumatic Stress, Istanbul, Turkey, June 5–8, 1999, and the 16th annual meeting of the International Society for Traumatic Stress Studies, Miami, Nov. 14–17, 1999. Received Dec. 29, 1999; revision received July 7, 2000; accepted Oct. 23, 2000. From the Departments of Psychiatry and Psychosocial Medicine, University Hospital. Address reprint requests to Dr. Schnyder, Psychiatric Department, University Hospital, Culmannstrasse 8, 8091 Zurich, Switzerland; [email protected] (e-mail). Supported by the Swiss National Science Foundation (project number 32-43640.95).
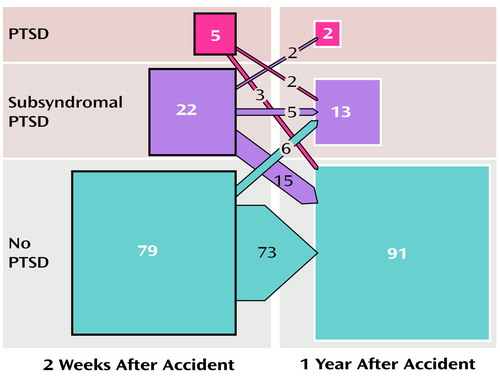
Figure 1. Diagnoses of Full-Blown, Subsyndromal, and No Posttraumatic Stress Disorder (PTSD) and Change of Diagnoses in the First Year After the Accident for 106 Severely Injured Accident Victimsa
aNumerals are numbers of patients; sizes of squares and arrows represent approximate quantitative proportions. The time criterion for PTSD was not fulfilled at 2 weeks after the accident.
1. Erichsen JE: On Railway and Other Injuries of the Nervous System. London, Walton & Maberly, 1866Google Scholar
2. Norris FH: Epidemiology of trauma: frequency and impact of different potentially traumatic events on different demographic groups. J Consult Clin Psychol 1992; 60:409–418Crossref, Medline, Google Scholar
3. Malt UF, Olafsen OM: Psychological appraisal and emotional response to physical injury: a clinical, phenomenological study of 109 adults. Psychiatr Med 1992; 10:117–134Medline, Google Scholar
4. Schnyder U, Malt UF: Acute stress response patterns to accidental injuries. J Psychosom Res 1998; 45:419–424Crossref, Medline, Google Scholar
5. Malt UF, Blikra G: Psychosocial consequences of road accidents. Eur Psychiatry 1993; 8:227–228Google Scholar
6. Blanchard EB, Hickling EJ, Taylor AE, Loos WR: Psychiatric morbidity associated with motor vehicle accidents. J Nerv Ment Dis 1995; 183:495–504Crossref, Medline, Google Scholar
7. Koren D, Arnon I, Klein E: Acute stress response and posttraumatic stress disorder in traffic accident victims: a one-year prospective, follow-up study. Am J Psychiatry 1999; 156:367–373Abstract, Google Scholar
8. Ursano RJ, Fullerton CS, Epstein RS, Crowley B, Kao T-C, Vance K, Craig KJ, Dougall AL, Baum A: Acute and chronic posttraumatic stress disorder in motor vehicle accident victims. Am J Psychiatry 1999; 156:589–595Abstract, Google Scholar
9. Malt U: The long-term psychiatric consequences of accidental injury: a longitudinal study of 107 adults. Br J Psychiatry 1988; 153:810–818Crossref, Medline, Google Scholar
10. Mayou R, Tyndel S, Bryant B: Long-term outcome of motor vehicle accident injury. Psychosom Med 1997; 59:578–584Crossref, Medline, Google Scholar
11. Lim LC: Delayed emergence of post-traumatic stress disorder. Singapore Med J 1991; 32:92–93Medline, Google Scholar
12. Schnyder U, Buddeberg C: Psychosocial aspects of accidental injuries—an overview. Langenbecks Arch Chir 1996; 381:125–131Crossref, Medline, Google Scholar
13. Schnyder U, Mörgeli HP, Nigg C, Klaghofer R, Renner N, Trentz O, Buddeberg C: Early psychological reactions to severe injuries. Crit Care Med 2000; 28:86–92Crossref, Medline, Google Scholar
14. Baker SP, O’Neill B: The injury severity score: an update. J Trauma 1976; 16:882–885Crossref, Medline, Google Scholar
15. Teasdale G, Jennett B: Assessment of coma and impaired consciousness: a practical scale. Lancet 1974; 2:81–84Crossref, Medline, Google Scholar
16. Horowitz MJ, Wilner N, Alvarez W: Impact of Event Scale: a measure of subjective stress. Psychosom Med 1979; 41:209–218Crossref, Medline, Google Scholar
17. McFall ME, Smith DE, Roszell DK, Tarver DJ, Malas KL: Convergent validity of measures of PTSD in Vietnam combat veterans. Am J Psychiatry 1990; 147:645–648Link, Google Scholar
18. Blake DD, Weathers FW, Nagy L, Kaloupek DG, Klauminzer G, Charney DS, Keane TM: A clinician rating scale for assessing current and lifetime PTSD: the CAPS-1. Behavior Therapist 1990; 18:187–188Google Scholar
19. Blake DD, Weathers FW, Nagy L, Kaloupek DG, Gusmann FD, Charney DS, Keane TM: The development of a clinician-administered PTSD scale. J Trauma Stress 1995; 8:75–90Crossref, Medline, Google Scholar
20. Berkman LF, Syme L: Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol 1979; 109:186–204Crossref, Medline, Google Scholar
21. Schaefer C, Coyne JC, Lazarus RS: The health-related functions of social support. J Behav Med 1981; 4:381–402Crossref, Medline, Google Scholar
22. Siegrist J, Dittmann KH: Inventar zur Erfassung lebensverändernder Ereignisse (ILE), in ZUMA—Handbuch sozialwissenschaftlicher Skalen. Bonn, Informationszentrum Sozialwissenschaften, 1983Google Scholar
23. Egle UT, Hoffmann SO, Steffens M: Psychosocial risk factors and protective factors in childhood as predisposition to psychic disorders in adulthood: current state of research. Nervenarzt 1997; 68:683–695Crossref, Medline, Google Scholar
24. Antonovsky A: Unraveling the Mystery of Health: How People Manage Stress and Stay Well. San Francisco, Jossey Bass, 1987Google Scholar
25. Antonovsky A: The structure and properties of the sense of coherence scale. Soc Sci Med 1993; 36:725–733Crossref, Medline, Google Scholar
26. Muthny FA: Freiburger Fragebogen zur Krankheitsverarbeitung: Manual. Weinheim, Germany, Beltz, 1989Google Scholar
27. Breslau N, Davis GC, Andreski P, Peterson EL, Schultz LR: Sex differences in posttraumatic stress disorder. Arch Gen Psychiatry 1997; 54:1044–1048Google Scholar
28. Malt UF: Coping with accidental injury. Psychiatr Med 1992; 10:135–147Medline, Google Scholar
29. Moore AD, Bombardier CH, Brown PB, Patterson DR: Coping and emotional attributions following spinal cord injury. Int J Rehab Res 1994; 17:39–48Crossref, Medline, Google Scholar
30. Tabachnick BG, Fidell LS: Using Multivariate Statistics. New York, HarperCollins, 1996Google Scholar
31. Stein MB, Walker JR, Hazen AL, Forde DR: Full and partial posttraumatic stress disorder: findings from a community survey. Am J Psychiatry 1997; 154:1114–1119Google Scholar
32. Mayou R, Bryant B, Duthie R: Psychiatric consequences of road traffic accidents. Br Med J 1993; 307:647–651Crossref, Medline, Google Scholar
33. Warden DL, Labbate LA, Salazar AM, Nelson R, Sheley E, Staudenmeier J, Martin E: Posttraumatic stress disorder in patients with traumatic brain injury and amnesia for the event? J Neuropsychiatry Clin Neurosci 1997; 9:18–22Google Scholar
34. Bryant RA, Marosszeky JE, Crooks J, Gurka JA: Posttraumatic stress disorder after severe traumatic brain injury. Am J Psychiatry 2000; 157:629–631Link, Google Scholar
35. Bryant RA, Harvey AG: Relationship between acute stress disorder and posttraumatic stress disorder following mild traumatic brain injury. Am J Psychiatry 1998; 155:625–629Link, Google Scholar
36. Ohry A, Rattok J, Solomon Z: Post-traumatic stress disorder in brain injury patients. Brain Injury 1996; 10:687–695Crossref, Medline, Google Scholar
37. Weisæth L: Importance of high response rates in traumatic stress research. Acta Psychiatr Scand Suppl 1989; 355:131–137Crossref, Medline, Google Scholar
38. Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P: Trauma and posttraumatic stress disorder in the community—the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry 1998; 55:626–632Crossref, Medline, Google Scholar
39. Bryant RA, Harvey AG: Initial posttraumatic stress responses following motor vehicle accidents. J Trauma Stress 1996; 9:223–234Crossref, Medline, Google Scholar
40. Feinstein A, Dolan R: Predictors of post-traumatic stress disorder following physical trauma: an examination of the stressor criterion. Psychol Med 1991; 21:85–91Crossref, Medline, Google Scholar
41. Mayou R, Simkin S, Threlfall J: The effects of road traffic accidents on driving behaviour. Injury 1991; 22:365–368Crossref, Medline, Google Scholar
42. Blanchard EB, Hickling EJ, Mitnick N, Taylor AE, Loos WR, Buckley TC: The impact of severity of physical injury and perception of life threat in the development of post-traumatic stress disorder in motor vehicle accident victims. Behav Res Ther 1995; 33:529–534Crossref, Medline, Google Scholar
43. Blanchard EB, Hickling EJ, Forneris CA, Taylor AE, Buckley TC, Loos WR, Jaccard J: Prediction of remission of acute posttraumatic stress disorder in motor vehicle accident victims. J Trauma Stress 1997; 10:215–234Medline, Google Scholar



