Outcome of Dysthymic Disorder at 5-Year Follow-Up: The Effect of Familial Psychopathology, Early Adversity, Personality, Comorbidity, and Chronic Stress
Abstract
OBJECTIVE: This study sought to identify predictors of course and outcome in dysthymic disorder. METHOD: Eighty-six outpatients with early-onset dysthymic disorder (before age 21) participated in a prospective 5-year follow-up study. Family history of psychopathology, early home environment, axis I and II comorbidity, social support, and chronic stress were assessed at baseline. The Longitudinal Interval Follow-up Evaluation and the Hamilton Depression Rating Scale were used in the follow-up assessments conducted at 30 and 60 months. RESULTS: Comorbid anxiety disorder, cluster C and depressive personality features, and chronic stress were associated with a lower rate of recovery from dysthymic disorder, while family history of bipolar disorder was associated with a higher probability of recovery. Family history of dysthymic disorder, poor childhood maternal and paternal relationships, childhood sexual abuse, cluster C features, neuroticism, a history of anxiety and eating disorders, and chronic stress predicted higher levels of depression at follow-up. Multivariate models indicated that almost all domains contributed to the prediction of course and outcome. CONCLUSIONS: The course and outcome of dysthymic disorder is best conceptualized within a multifactorial framework, with family history of psychopathology, early adversity, axis I and II comorbidity, and chronic stress all making important contributions.
Dysthymic disorder, a chronic, low-grade depressive condition, has a high prevalence in both community and outpatient samples, with rates of 3%–6% (1, 2) and 22%–36% (3, 4), respectively. Major depressive episodes are a frequent complication, as almost all individuals with dysthymic disorder experience exacerbations that meet criteria for a major depressive episode, or “double depression” (5), at some point in their lives (6–9). At any given point in the course of dysthymic disorder, the level of symptoms is typically mild. Over time, however, individuals with dysthymic disorder experience greater cumulative symptoms and more suicide attempts and hospitalizations than persons with episodic major depression (6). In addition, the level of functional impairment in dysthymic disorder typically equals or exceeds that in major depressive disorder and increases further during superimposed major depressive disorder episodes (10–12).
Since dysthymic disorder is defined largely by its persistence, studies examining factors that predict the long-term course and outcome of the disorder are critical. However, the few studies have focused primarily on demographic and clinical variables, and most have examined relatively short follow-up periods (i.e., 30 months or less). In a 2-year follow-up of patients with double depression, Keller and colleagues (13) found that age, marital status, number of previous major depressive disorder episodes, subtype of major depressive disorder episode, and duration and type of onset of major depressive disorder did not predict recovery from the preexisting dysthymic disorder. In a combined retrospective/prospective follow-up of depressive disorders in childhood, Kovacs and colleagues found that earlier age at onset (14) and comorbid externalizing disorders (15) predicted a longer duration of dysthymic disorder, while sex, superimposed major depressive disorder, and comorbid anxiety disorders failed to predict recovery (14, 16, 17). In a previous report from this project (18), we found that age, gender, educational attainment, history of major depressive disorder, age at onset of dysthymic disorder, and comorbid anxiety, substance use, and personality disorders did not predict recovery from dysthymic disorder or level of depressive symptoms at 30-month follow-up. However, depressive personality predicted level of depression even after baseline depressive symptoms were controlled (19). Early adversity and family history of psychopathology were also associated with course and outcome (20).
The present article extends our earlier reports by examining a longer follow-up period and a broader range of predictors. The follow-up period was increased to 5 years, exceeding the length of most previous studies of prognostic factors in dysthymic disorder. In addition, we hypothesized that the course of dysthymic disorder is influenced by several factors, including distal variables such as familial psychopathology and early adversity, clinical variables such as comorbid axis I psychopathology and personality traits and disorders, and proximal socioenvironmental factors such as chronic stress and social support. Hence, we explored the prognostic utility of a multifactorial model and examined whether each domain would contribute to predicting the outcome of dysthymic disorder. We were particularly interested in determining whether the variables that best distinguished patients with dysthymic disorder from those with episodic major depressive disorder—family history of dysthymic disorder, early adversity, and personality disorders (21–23)—would also be associated with a more chronic course of dysthymic disorder.
Method
Subjects
Data for this report come from a larger family follow-up study of early-onset (onset before age 21 years) dysthymic disorder, described in detail elsewhere (6, 21). Subjects were 97 outpatients with a DSM-III-R diagnosis of dysthymic disorder, primary and early-onset types. At entry into the study, 57.7% were experiencing a superimposed major depressive disorder episode, and 77.9% had a lifetime history of major depressive disorder. They were between the ages of 18 and 60 years, spoke English, and had knowledge of at least one first-degree relative. Most patients were recruited from the Outpatient Psychiatry Department and the Psychological Center at the State University of New York at Stony Brook. A few patients were referred from a community mental health center and the Counseling Center at the State University of New York at Stony Brook. As this was a naturalistic study, treatment was not controlled. However, we obtained detailed information about treatment during follow-up from patients and medical records. After giving a complete description of the study to patients, we obtained written informed consent from all participants.
We attempted to conduct follow-up evaluations at 30 and 60 months after the baseline assessment. At least one follow-up was completed for 86 patients (88.7% of the sample). The mean interval between baseline and last follow-up was 57.5 months (SD=7.5). Patients who were unavailable for follow-up were compared to those who were available on 14 baseline clinical and demographic variables, with no significant differences between groups (6).
Family history information was obtained from patients for all first-degree relatives older than 14 years (N=446). Direct interviews were conducted with 40% of these relatives (70% of the living relatives we had permission to contact). When we were unable to interview a family member, we attempted to obtain information about this relative from at least one additional informant.
Baseline Evaluation
The baseline evaluation included assessment with the Structured Clinical Interview for DSM-III-R (SCID) (24) and the 24-item modified Hamilton Depression Rating Scale (25), which focused on the worst week of the patient’s current major depressive disorder episode or the worst week in the past month if the patient was not currently experiencing an episode. Patients were administered the Personality Disorder Examination (26), expanded to assess depressive personality traits according to Akiskal’s criteria (9) (see reference 19 for details).
Early Home Environment
The Early Home Environment Interview (22) was administered at baseline. The Early Home Environment Interview is a semistructured interview that assesses five aspects of the early home environment before age 15: loss (parental death, divorce, or separation from a parent for at least 6 months), physical abuse (being hit hard or often enough to leave bruises, draw blood, or require medical attention), sexual abuse (nonconsenting genital contact initiated by someone at least 5 years older), and the quality of the relationship with each parent (two scales). Loss, physical abuse, and sexual abuse are scored as present or absent. The scales measuring quality of the relationship with parents include six items: rarely spent time or engaged in activities with parent, lack of parental supervision, rarely confided in parent, constantly criticized by parent, often rejected by parent, and rarely felt loved by parent. Scores range from 0 to 6, with higher scores indicating poorer relationships.
Family History
Family history data were collected by using an expanded version of the Family History Research Diagnostic Criteria interview (27), the Family History Interview for Personality Disorders (28), and direct interviews with relatives using the SCID and the Personality Disorder Examination. Lifetime best estimate diagnoses were derived for each relative by using all available information (29).
As described elsewhere (20), family history scores were estimated with hierarchical linear modeling (30) to adjust for differences between families in the number of relatives, gender of relatives, and type of diagnostic data available. A two-level model was used, treating relatives as repeated observations (level 1) nested within families (level 2), with gender and type of diagnostic data treated as covariates. For each proband, family history scores were derived for major depressive disorder, dysthymic disorder, alcohol abuse/dependence, drug abuse/dependence, any anxiety disorder, and any personality disorder. Family history scores for bipolar I and II disorders could not be estimated because of their low prevalence; hence, we used the proportion of relatives with the disorder instead.
The interrater reliability of the interviews was generally good to excellent (21–23, 28, 29). The kappas for the SCID ranged from 0.78 to 0.90. The intraclass correlations (ICC) for the Personality Disorder Examination dimensional scores ranged from 0.77 to 0.92. The kappas for the Early Home Environment Interview childhood sexual and physical abuse items were both 0.68, and the ICCs for the maternal and paternal relationship scales were 0.83 and 0.69, respectively. The kappas for best-estimate diagnoses ranged from 0.75 to 0.90.
Inventories
Patients completed a battery of questionnaires, including the Interpersonal Support Evaluation List (31) and the revised Eysenck Personality Questionnaire (32). The Interpersonal Support Evaluation List is a widely used measure of perceived social support consisting of four scales: appraisal, belonging, tangible support, and self-esteem. The self-esteem scale was not included because of its overlap with measures of depressive symptoms. Appraisal assesses the perceived availability of someone to talk with about one’s problems, belonging assesses the perceived availability of people with whom one can do things, and tangible support reflects the perceived availability of material aid. As the subscales were highly intercorrelated, they were summed to yield a total score.
The Eysenck Personality Questionnaire is a widely used personality inventory consisting of four scales: neuroticism, extroversion, psychoticism, and lie (social desirability). Only the neuroticism and psychoticism scales were used in this report.
Follow-Up Evaluations
Follow-up assessments included the Longitudinal Interval Follow-Up Evaluation (33), an abbreviated version of the Interview for Recent Life Events (34), and the Hamilton depression scale. The Longitudinal Interval Follow-Up Evaluation is a semistructured interview assessing the longitudinal course of axis I disorders. It has been used successfully in follow-up intervals as long as 12 years (35). Recovery from dysthymic disorder was defined as a minimum of 8 consecutive weeks with minimal or no symptoms. To assess interrater reliability, 13 randomly selected audiotapes of Longitudinal Interval Follow-Up Evaluation interviews were rated by an independent interviewer. The kappa was 0.83 for recovery from dysthymic disorder. We also found high concordance between ratings made immediately after a 6-month follow-up and ratings made about those same 6 months at the 30-month follow-up (18). The ICC for the Hamilton depression scale was 0.95.
The Interview for Recent Life Events (34) is an investigator-rated measure that assesses the date and objective negative impact of a list of 63 specific life events. To make our lengthy assessment battery more manageable, we reduced the list of specific events to 20 by combining similar events into single items and eliminating events that appeared relatively minor, drawing on data reported by Brugha and Cragg (36). Events were rated as either acute or chronic, with events occurring within a discrete time period deemed acute and ongoing events lasting at least 6 months deemed chronic. For the present report, we focused on chronic stressors in the year before recovery (or the year before the 5-year evaluation), as chronic stress is more likely than acute stressors to play a role in maintaining a disorder. Events were rated on a 6-point severity scale and summed to yield a total score from which the mean for the year was derived. The ICC for mean chronic stress ratings was 0.56.
The follow-up interviews were conducted by doctoral- and master’s-level clinicians and advanced graduate students in clinical psychology with prior experience in diagnostic interviewing. The interviewers were blind to all baseline data.
Data Analysis
We examined the prognostic value of variables from the following domains: descriptive characteristics (age, sex, marital status, education, socioeconomic status, age at onset of dysthymic disorder), familial psychopathology (major depressive disorder, dysthymic disorder, bipolar disorder, anxiety disorder, substance abuse/dependence, personality disorder), early home environment (relationships with mother and father, childhood physical and sexual abuse), personality and personality disorder traits (Eysenck Personality Questionnaire neuroticism and extraversion, cluster A, B, and C, and depressive personality disorder dimensional scores), lifetime axis I comorbidity (major depressive disorder, anxiety disorder, eating disorder, alcohol/drug abuse/dependence), and socioenvironmental factors (chronic stress, social support). We did not include treatment as a predictor, since it was not associated with the course of dysthymic disorder (6). The two dependent variables were recovery from dysthymic disorder and Hamilton depression scale score at 5-year follow-up.
The baseline and follow-up Hamilton depression scale scores were significantly correlated (r=0.31, df=95, p<0.01). Therefore, in all univariate analyses that used the follow-up Hamilton depression scale as the dependent variable, partial correlations were computed by controlling for Hamilton depression scale scores at baseline. Recovery from dysthymic disorder was analyzed with univariate Cox proportional hazards models. As the baseline Hamilton depression scale did not predict recovery (hazard ratio=0.99, χ2=0.94, df=1, p=0.33), we did not include it as a covariate. To take into account the relationships between predictors, multivariate analyses were conducted by using hierarchical Cox proportional hazards and multiple linear regression models. Variables used in the Cox proportional hazards analyses met the assumptions underlying this method. We examined all two-way interactions, but no more were significant than would be expected by chance. All tests were two tailed.
Results
The patients were predominantly white (91.9%, N=79) and female (75.6%, N=65). Their mean age was 32.1 years (SD=9.7). Marital status was as follows: 46.5% (N=40) had never married, 31.4% (N=27) were married, 19.8% (N=17) were separated or divorced, and 2.3% (N=2) were widowed. The patients’ mean score on the Hollingshead’s Four-Factor Index of Social Status (37) was in the mid-range of social class III (mean=34.6, SD=13.6). The subjects were moderately depressed at baseline, with a mean 24-item Hamilton depression scale score of 25.7 (SD=10.4). At 5-year follow-up, the recovery rate from dysthymic disorder was 52.3% (N=45) (6).
None of the descriptive characteristics predicted recovery or Hamilton depression scale scores at 5-year follow-up. Neither a superimposed major depressive disorder episode at baseline nor lifetime history of major depressive disorder was associated with recovery or level of symptoms at follow-up. A history of anxiety disorder, cluster C and depressive personality features, and chronic stress were significantly associated with lower recovery rates (Table 1). In contrast, a family history of bipolar disorder was significantly associated with a higher probability of recovery. After baseline Hamilton depression scale scores were controlled, higher Hamilton depression scale scores at follow-up were predicted by a greater familial loading of dysthymic disorder, poorer maternal and paternal relationships, childhood sexual abuse, history of anxiety disorder and eating disorder, cluster C personality disorder features, higher Eysenck Personality Questionnaire neuroticism scores, and higher levels of chronic stress in the 12 months before follow-up.
Blocks of significant univariate predictors were used to construct a hierarchical Cox proportional hazards model predicting recovery. The order of entry was based on the likely chronological sequence of the impact of each domain: family history of bipolar disorder, cluster C and depressive personality features, comorbid anxiety disorder, and chronic stress in the year before recovery. Family history of bipolar disorder significantly predicted recovery from dysthymic disorder (χ2=4.07, df=1, N=86, p=0.04). Adding cluster C and depressive personality features to the model resulted in a significant change (change in χ2=7.71, df=1, N=86, p=0.02). Comorbid anxiety improved the model further (change in χ2=4.17, df=1, N=86, p=0.04). Finally, chronic stress also contributed a significant increment (change in χ2=4.69, df=1, N=72, p=0.03).
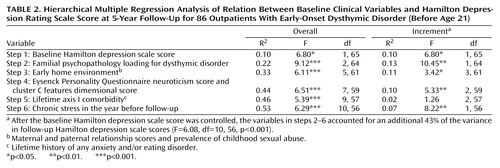
Similarly, we used blocks of the significant univariate predictors from each domain to construct a hierarchical multiple linear regression model predicting Hamilton depression scale scores at follow-up. Baseline Hamilton depression scale scores were entered first, followed by family history of dysthymic disorder, early adversity (early maternal and paternal relationships, childhood sexual abuse), personality (neuroticism and cluster C features), comorbid axis I psychopathology (anxiety and eating disorders), and chronic stress in the year before follow-up, in that order. As Table 2 shows, after the baseline Hamilton depression scale score was controlled, the group of prognostic indicators accounted for an additional 43% of the variance in follow-up Hamilton depression scale scores (F=6.08, df=10, 56, p<0.001). Each block of predictors added a significant increment to the preceding blocks, with the exception of axis I comorbidity.
Discussion
We examined predictors of recovery and depressive symptoms in a 5-year follow-up of outpatients with early-onset dysthymic disorder and found that the domains of familial psychopathology, early adversity, axis I comorbidity, personality, and socioenvironmental factors were all associated with outcome. After the analysis controlled for baseline depressive symptoms, predictors entered in chronological order of their presumed effects accounted for an impressive 43% of the variance in the level of depression at 5-year follow-up. Previous studies, including our own 30-month follow-up of this group of subjects, have been less successful in identifying predictors of the course of dysthymic disorder (13–20). However, these studies have generally examined a limited number of predictors and followed patients for shorter periods of time. The difference suggests that more comprehensive models and longer durations of follow-up are necessary to identify prognostic factors in dysthymic disorder.
Comorbid anxiety disorder, depressive personality features, cluster C traits, and chronic stress were all associated with a lower probability of recovery from dysthymic disorder. In contrast, a family history of bipolar disorder was associated with a greater likelihood of recovery. Akiskal (9) has suggested that some patients with dysthymic disorder may have bipolar spectrum conditions. If family history of bipolar disorder is a marker for this subgroup, it is not surprising that these patients experience a more cyclic, episodic course with a faster rate of recovery. However, given that family history of bipolar disorder had a low base rate in the study group and the confidence interval was large, this finding should be taken with caution.
Higher levels of depression at follow-up were predicted by a greater familial loading for dysthymic disorder, poorer maternal and paternal relationships, childhood sexual abuse, increased neuroticism and cluster C features, a history of anxiety and eating disorders, and a higher level of chronic stress in the previous 12 months. These results are consistent with our previous findings indicating that, at baseline, the variables that best distinguished patients with dysthymic disorder from those with episodic major depressive disorder were rates of dysthymic disorder in relatives, early adversity, and axis II comorbidity (21–23). Thus, it appears that the same variables that distinguish dysthymic disorder from episodic major depressive disorder are also among the best predictors of a poor course and outcome for patients with dysthymic disorder.
Chronic stress was one of the strongest predictors of both failure to recover and depressive symptoms at 5-year follow-up. Although the results are not presented here, we conducted further analyses examining the temporal relationship between chronic stress and recovery from dysthymic disorder. Patients who recovered had lower levels of chronic stress throughout the entire follow-up period, rather than a reduction in stress at a particular point before recovery. This pattern suggests that chronic stress is a relatively stable attribute of poor-outcome patients. High levels of chronic stress may, in part, be due to other poor prognostic factors such as early adversity, personality disturbance, and comorbidity (38). For example, in this study group, there were low, but significant, correlations between the quality of the maternal relationship (r=0.22, df=77, p<0.02), childhood sexual abuse (r=0.25, df=77, p<0.01), cluster C dimensional scores (r=0.23, df=77, p<0.02), and lifetime anxiety disorder (r=0.22, df=77, p=0.03) assessed at baseline and the level of chronic stress in the year before follow-up. These data suggest the need for a more detailed examination of the complex links between early adversity, comorbidity, chronic stress, and the course of dysthymic disorder.
We have reported elsewhere that acute stressors may precipitate superimposed major depressive disorder episodes in the course of dysthymic disorder (39). As acute stress is more likely to contribute to relapse than to maintenance of depression, we did not examine the role of acute stressors in recovery and symptoms at follow-up. However, other authors have proposed that positive, neutralizing, or “fresh-start” events play an important role in recovery (40). Although we did not assess these events, they may be worth examining in future studies of the course of dysthymic disorder.
Fewer variables predicted recovery than predicted Hamilton depression scale scores in this study, perhaps because recovery is a heterogeneous outcome in dysthymic disorder, with some patients experiencing a sustained recovery and others having a relatively brief recovery in the context of a generally chronic course (6). Combining these subgroups may obscure important predictors. We did not analyze predictors of relapse in this article, owing to the relatively small number of patients who had recovered and relapsed at this point in the follow-up.
Our study group was representative of patients with dysthymic disorder in most clinical settings in that many patients had a superimposed major depressive disorder episode and others had a past history of major depressive disorder. Although we cannot be certain that our findings would generalize to “pure” dysthymic disorder patients, we have found few differences between patients with double depression and those with dysthymic disorder alone in familial psychopathology, early adversity, and comorbidity (21–23). Moreover, in the present report, superimposed major depressive disorder episodes (current and lifetime) did not predict recovery from dysthymic disorder or Hamilton depression scale scores at follow-up.
The strengths of our study include its prospective design, relatively lengthy follow-up period, and use of an extensive assessment battery, semistructured interviews, and blind follow-up evaluations. However, the study also has several limitations. We conducted a large number of statistical tests without adjusting significance levels, raising the possibility that some findings might be due to chance. Our study group was modest in size, limiting our power to detect small effects. Many of our family history variables had low base rates and large confidence intervals, suggesting that these analyses should be taken cautiously. Relative to the instances of recovery, the number of predictors examined was large. Patients were asked to report about relatively lengthy follow-up intervals. Finally, the size of the significant effects was moderate; hence, their clinical utility may be limited. Nonetheless, our findings suggest the value of conceptualizing the course and outcome of dysthymic disorder within a multifactorial framework, with family history of psychopathology, early adversity, personality, axis I comorbidity, and chronic stress all making important contributions.
 |
 |
Received Nov. 27, 2000; revision received June 6, 2001; accepted July 9, 2001. From the Department of Psychology and the Department of Psychiatry and Behavioral Science, State University of New York at Stony Brook. Address correspondence to Dr. Klein, Department of Psychology, SUNY at Stony Brook, Stony Brook, NY 11794-2500; [email protected] (e-mail). Supported by grant MH-45757 from NIMH. The authors thank Suzanne Rose, M.A., and Julie B. Leader, Ph.D., for help with interviewing and Joseph E. Schwartz, Ph.D., for help with data analysis.
1. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8-19Crossref, Medline, Google Scholar
2. Weissman MM, Leaf PJ, Bruce ML, Florio L: The epidemiology of dysthymia in five communities: rates, risks, comorbidity, and treatment. Am J Psychiatry 1988; 145:815-819Link, Google Scholar
3. Klein DN, Dickstein S, Taylor EB, Harding K: Identifying chronic affective disorders in outpatients: validation of the General Behavior Inventory. J Consult Clin Psychol 1989; 57:106-111Crossref, Medline, Google Scholar
4. Markowitz JC, Moran ME, Kocsis JH, Francis AJ: Prevalence and comorbidity of dysthymic disorder among psychiatric outpatients. J Affect Disord 1992; 24:63-71Crossref, Medline, Google Scholar
5. Keller MB, Shapiro RW: “Double depression”: superimposition of acute depressive episodes on chronic depressive disorders. Am J Psychiatry 1982; 139:438-442Link, Google Scholar
6. Klein DN, Schwartz JE, Rose S, Leader JB: Five-year course and outcome of dysthymic disorder: a prospective, naturalistic follow-up study. Am J Psychiatry 2000; 157:931-939Link, Google Scholar
7. Kovacs M, Akiskal HS, Gatsonis C, Parrone PL: Childhood-onset dysthymic disorder: clinical features and prospective naturalistic outcome. Arch Gen Psychiatry 1994; 51:365-374Crossref, Medline, Google Scholar
8. Horwath E, Johnson J, Klerman GL, Weissman MM: Depressive symptoms as relative and attributable risk factors for first-onset major depression. Arch Gen Psychiatry 1992; 49:817-823Crossref, Medline, Google Scholar
9. Akiskal HS: Dysthymic disorder: psychopathology of proposed chronic depressive subtypes. Am J Psychiatry 1983; 140:11-20Link, Google Scholar
10. Friedman RA: Social and occupational adjustment in chronic depression, in Diagnosis and Treatment of Chronic Depression. Edited by Kocsis JH, Klein DN. New York, Guilford, 1995, pp 89-102Google Scholar
11. Hays RD, Wells KB, Sherbourne CD, Rogers W, Spritzer K: Functioning and well-being outcomes of patients with depression compared with chronic general medical illnesses. Arch Gen Psychiatry 1995; 52:11-19Crossref, Medline, Google Scholar
12. Leader JB, Klein DN: Social adjustment in dysthymia, double depression and episodic major depression. J Affect Disord 1996; 37:91-101Crossref, Medline, Google Scholar
13. Keller MB, Lavori PW, Endicott J, Coryell W, Klerman GL: “Double depression”: two-year follow-up. Am J Psychiatry 1983; 140:689-694Link, Google Scholar
14. Kovacs M, Feinberg TL, Crouse-Novak MA, Pausauskas SL, Finkelstein R: Depressive disorders in childhood, I: a longitudinal prospective study of characteristics and recovery. Arch Gen Psychiatry 1984; 41:229-237Crossref, Medline, Google Scholar
15. Kovacs M, Obrosky DS, Gatsonis C, Richards C: First-episode major depressive and dysthymic disorder in childhood: clinical and sociodemographic factors in recovery. J Am Acad Child Adolesc Psychiatry 1997; 36:777-784Crossref, Medline, Google Scholar
16. Kovacs M, Paulsauskas S, Gatsonis C, Richards C: Depressive disorders in childhood, III: a longitudinal study of comorbidity with and risk for conduct disorders. J Affect Disord 1988; 15:205-217Crossref, Medline, Google Scholar
17. Kovacs M, Gatsonis C, Paulsauskas SL, Richards C: Depressive disorders in childhood, IV: a longitudinal study of comorbidity with and risk for anxiety disorders. Arch Gen Psychiatry 1989; 46:776-782Crossref, Medline, Google Scholar
18. Klein DN, Norden KA, Ferro T, Leader JB, Kasch KL, Klein LM, Schwartz JE: Thirty-month naturalistic follow-up study of early onset dysthymic disorder: course, stability, and prediction of outcome. J Abnorm Psychol 1998; 107:338-348Crossref, Medline, Google Scholar
19. Klein DN, Shih JH: Depressive personality: associations with DSM-III-R mood and personality disorders and negative and positive affectivity, 30-month stability, and prediction of course of axis I depressive disorders. J Abnorm Psychol 1998; 107:319-327Crossref, Medline, Google Scholar
20. Durbin CE, Klein DN, Schwartz JE: Predicting the 2-year outcome of dysthymic disorder: the roles of childhood adversity and family history of psychopathology. J Consult Clin Psychol 2000; 68:57-63Crossref, Medline, Google Scholar
21. Klein DN, Riso LP, Donaldson SK, Schwartz JE, Anderson RL, Ouimette PC, Lizardi H, Aronson TA: Family study of early-onset dysthymia: mood and personality disorders in relatives of outpatients with dysthymia and episodic major depression and normal controls. Arch Gen Psychiatry 1995; 52:487-496Crossref, Medline, Google Scholar
22. Lizardi H, Klein DN, Ouimette PC, Riso LP, Anderson RL, Donaldson SK: Reports of the childhood home environment in early-onset dysthymia and episodic major depression. J Abnorm Psychol 1995; 104:132-139Crossref, Medline, Google Scholar
23. Pepper CM, Klein DN, Anderson RL, Riso LP, Ouimette PC, Lizardi H: DSM-III-R axis II comorbidity in dysthymia and major depression. Am J Psychiatry 1995; 152:239-247Link, Google Scholar
24. Spitzer RL, Williams JBW, Gibbon M, First MB: User’s Guide for the Structured Clinical Interview for DSM-III-R (SCID). Washington, DC, American Psychiatric Press, 1990Google Scholar
25. Miller IW, Bishop S, Norman WH, Maddever H: The Modified Hamilton Rating Scale for Depression: reliability and validity. Psychiatry Res 1985; 14:131-142Crossref, Medline, Google Scholar
26. Loranger AW, Susman VL, Oldham JM, Russakoff M: The Personality Disorder Examination (PDE) Manual. Yonkers, NY, DV Communications, 1988Google Scholar
27. Andreasen NC, Endicott J, Spitzer RL, Winokur G: The family history method using diagnostic criteria: reliability and validity. Arch Gen Psychiatry 1977; 34:1229-1235Crossref, Medline, Google Scholar
28. Ferro T, Klein DN, Norden KA, Donaldson SK, Lizardi H: Development and reliability of the Family History Interview for Personality Disorders. J Personal Disord 1995, 9:169-177Google Scholar
29. Klein DN, Ouimette PC, Kelly HS, Ferro T, Riso LP: Test-retest reliability of team consensus best-estimate diagnoses of axis I and II disorders in a family study. Am J Psychiatry 1994; 151:1043-1047Link, Google Scholar
30. Bryk AS, Raudenbush SW: Hierarchical Linear Models: Applications and Data Analysis Methods. Newbury Park, Calif, Sage Publications, 1992Google Scholar
31. Cohen S, Mermelstein R, Kamarck T, Hoberman HM: Measuring the functional components of social support, in Social Support: Theory, Research and Applications. Edited by Sarason IG, Sarason BR. Dordrecht, the Netherlands, Martinus Nijhoff, 1985, pp 73-94Google Scholar
32. Eysenck SBG, Eysenck HJ, Barrett P: A revised version of the Psychoticism Scale. Personality and Individual Differences 1985; 6:21-29Crossref, Google Scholar
33. Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC: The Longitudinal Interval Follow-Up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry 1987; 44:540-548Crossref, Medline, Google Scholar
34. Paykel ES: The Interview for Recent Life Events. Psychol Med 1997; 27:301-310Crossref, Medline, Google Scholar
35. Surtees PG, Barkley C: Future imperfect: the long-term outcome of depression. Br J Psychiatry 1994; 164:327-341Crossref, Medline, Google Scholar
36. Brugha TS, Cragg D: The list of threatening experiences: the reliability and validity of a brief life events questionnaire. Acta Psychiatr Scand 1990; 82:77-81Crossref, Medline, Google Scholar
37. Hollingshead AB: Four-Factor Index of Social Status. New Haven, Conn, Yale University, Department of Sociology, 1975Google Scholar
38. Brown GW, Moran P: Clinical and psychosocial origins of chronic depressive episodes, I: a community survey. Br J Psychiatry 1994; 165:447-456Crossref, Medline, Google Scholar
39. Moerk KM, Klein DN: The development of major depressive episodes during the course of dysthymic and episodic major depressive disorders: a retrospective examination of life events. J Affect Disord 2000; 58:117-123Crossref, Medline, Google Scholar
40. Brown GW, Adler Z, Bifulco A: Life events, difficulties and recovery from chronic depression. Br J Psychiatry 1988; 152:487-498Crossref, Medline, Google Scholar



