Violence and Leveraged Community Treatment for Persons With Mental Disorders
Abstract
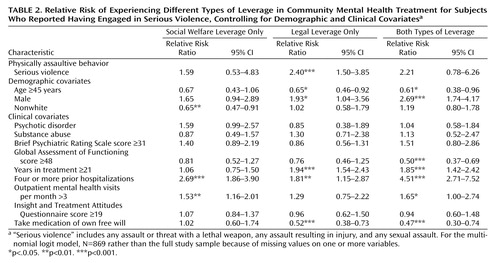
Objective: This article explores the link between violence and the practice of legally mandating treatment in the community or leveraging benefits from the social welfare system, such as subsidized housing and disability income support, to ensure adherence to treatment. Method: Data are presented from a survey of 1,011 persons with psychiatric disorders receiving treatment in public mental health service systems in five U.S. cities. Multinomial logit analysis was used to examine the association between physically assaultive behavior and experience of social welfare leverage, legal leverage, or both types of leverage, with the analyses controlling for demographic and clinical characteristics. Results: Across study sites, 18% to 21% of participants reported having committed violent acts in the past 6 months; 3% to 9% reported having used or made threats with a lethal weapon, committed sexual assault, or caused injury. About three-quarters of subjects who reported such serious violence also reported having experienced some form of leveraged treatment, compared with about one-half of subjects who did not report serious violence. Demographic and clinical factors that were independently associated with the likelihood of experiencing both types of leverage included younger age, male gender, poorer clinical functioning, more years in treatment, more frequent hospitalizations, higher frequency of outpatient visits, and negative attitudes toward medication adherence. Among participants who did not voluntarily take psychotropic medication, even minor assaultiveness was associated with having experienced legal leverage. Conclusions: A combination of concerns about safety and treatment nonadherence may influence decisions by clinicians and judges to apply legal leverage.
Over the past two decades, the debate over involuntary psychiatric intervention has followed the path of deinstitutionalization into the realm of community-based treatment. In that context, arguments about coercion and violence have become intertwined. On the one hand, the “dangerousness” criterion for inpatient civil commitment—rooted in the police powers of the state—has metamorphosed into a rationale for preventive outpatient commitment, which is justified as a means of preventing future dangerousness (2) . On the other hand, the putative absence of risk of violence in the large majority of persons with serious mental illness has been used to combat stigma, justify less restrictive alternatives to hospitalization, and promote independent community living for people with psychiatric disabilities (3 , 4) .
Most of the controversy over involuntary treatment in the community has focused on outpatient commitment, where the issue of violence appears in several roles. Attitudinal surveys reliably document the popular belief that mental illness causes violence (5) and the strong correlation of this belief with the public’s endorsement of policies that restrict the liberties of, or allow coercion of, persons with mental disorders (6 , 7) . Drawing on this well of public opinion, political advocates of outpatient commitment in recent years have capitalized on publicity generated by sensational acts of violence committed by people with mental disorders, explicitly promoting involuntary outpatient treatment as a measure that is necessary to ensure public safety (1) .
At the same time, in some states, outpatient commitment laws have been rewritten to be inapplicable to the most seriously violent persons with mental disorders—that is, those who would meet the dangerousness criteria for involuntary inpatient hospitalization. In states whose laws do require a finding of dangerousness for outpatient commitment, application of these laws has been limited. As Appelbaum (8) observed, “Clinicians and courts alike have a difficult time determining which patients are sufficiently impaired to meet dangerousness criteria for inpatient commitment and yet might be appropriate candidates for enforced outpatient care. . . . Having declared a patient dangerous for purposes of commitment, many clinicians understandably shy away from recommending outpatient treatment, fearing that they will be held responsible for any harm that occurs to the patient or to other people” (p. 349).
Concern about legal liability, specifically with respect to the clinician’s obligation to prevent patients from harming themselves or others, is perhaps the principal reason that efforts to implement outpatient commitment often exclude patients who have a history of serious violence (2) . For similar reasons, the two randomized clinical trials of outpatient commitment that have been conducted in the United States excluded patients who had a documented history of serious violence (9 , 10) , although one of the studies conducted a parallel observation of outcomes for the violent patients who were screened out of the randomized trial (11) .
Outpatient commitment, however, is only one of several tools derived from the social welfare and judicial systems that have gained widespread use as forms of leverage to ensure treatment adherence among persons with severe mental illness (1 , 12) . In mandated community treatment, negative events, such as incarceration, or positive events, such as placement in subsidized housing, can be made contingent on whether the patient adheres to treatment in the community. With each type of leverage, the issue of violence takes on different emphases.
One common form of leverage is exerted through the representative payeeship system: appointed money managers for patients’ disability funds may make a patient’s access to funds contingent on treatment adherence (13 , 14) . Research indicates that for people with severe mental illness, the risk of violence is significantly higher among those who receive disability or other entitlement payments (15) and among those who are financially dependent on family members (16 , 17) . One study found a significant association between the occurrence of physical fights and warnings from family members or case managers that money would be withheld if the person failed to attend mental health treatment appointments and take prescribed medications (13) . Thus, on the one hand, it seems clear that in some instances, violence could result from the mix of money disputes, poverty, disability, and conflicted family relationships. On the other hand, some representative payees may consider it one of their responsibilities to help prevent violence by using the contingency of financial control to ensure patients’ treatment compliance.
In another form of leverage, access to subsidized housing is made conditional on treatment adherence (18) . With affordable housing for people with psychiatric disabilities in short supply, managers of subsidized housing units may choose not to rent to patients they consider high-risk tenants—perhaps those with a comorbid substance use problem and a history of violence—or, if they do rent to such patients, they may do so on the condition that the tenants adhere to psychiatric treatment. In this regard, Monahan et al. (19) found that patients with comorbid substance use problems were significantly less likely than others to have had subsidized housing used as leverage to secure their adherence to treatment. This finding may be related to the fact that people with mental illness who have comorbid substance use problems tend to incite a greater fear of violence in the public mind (7) , and this fear may in turn result in their exclusion from subsidized housing. Ironically, patients with comorbid substance use diagnoses have a particularly high risk of homelessness—and homelessness, in turn, greatly increases the risk of violent behavior (20) .
Finally, several forms of leverage have developed within the criminal justice system. A judge may offer a mentally ill defendant a lenient sentence on the condition that the person participate in treatment or may make adherence to treatment a condition of probation (21 , 22) . Also, specialty mental health courts have emerged, explicitly linking criminal sanctioning and community-based treatment (23 , 24) . People with serious mental disorders who come into contact with the criminal justice system have a higher risk of future violence than those with no history of such contact (1) . In that light, persons who engage in violent behavior as a result of untreated mental illness might seem to be appropriate candidates for the use of criminal justice system leverage, and reduction of the risk of violence might seem to be an appropriate goal of such programs. While early mental health courts tended to focus on defendants charged with nonviolent misdemeanors, newer courts have focused on those charged with felonies, including violent felonies (23) .
Each of these types of leverage might rationally be applied to persons with mental illness who have a history of violent behavior. However, there are also reasons to expect that individuals considered dangerous might be excluded from some programs involving leveraged community treatment. The empirical association between violence and leveraged treatment is unknown. To date, there has been no systematic study of the prevalence of violent behavior in persons with mental disorders who have received leveraged treatment compared with those who have not. Information is also lacking about whether alternative forms of leverage are being withheld from people with mental illness who have acted violently, or whether the effect of violence history on the use of leverage may be conditioned by other variables, such as voluntary adherence to treatment. We address these issues by analyzing data from a survey conducted in 2002–2003 of 1,011 persons receiving treatment for psychiatric disorders in the public mental health service systems of five U.S. cities (19) .
Method
Study Design
The study method is described in detail elsewhere (19) . In brief, approximately 200 outpatients were recruited at publicly funded mental health treatment programs in each of five cities: Chicago, Durham, N.C., San Francisco, Tampa, Fla., and Worcester, Mass. The inclusion criteria for participation in the study were age 18–65 years, speaker of English or Spanish, first mental health treatment episode at least 6 months ago, and at least one outpatient treatment encounter with a publicly supported mental health service provider within the past 6 months. Persons receiving treatment only for substance use disorders and not for any other psychiatric disorder were excluded.
At the Worcester, Tampa, and San Francisco sites, potential subjects were recruited sequentially in the waiting rooms of outpatient clinics of the community mental health centers. In Durham, a list of potentially eligible subjects was created from management information system data, and patients from the list were randomly selected to be approached for participation in the study. The Chicago site used both sampling methods, enrolling about half the sample using the waiting room approach and the other half using the eligibility list approach. Participants were enrolled after receiving a complete description of the study and providing written informed consent. All sites received approval from their respective institutional review boards. Refusal rates varied from 2% to 13% across sites. A single structured interview, lasting about 90 minutes, was administered in person by a trained lay interviewer. Participants were paid $25 for the interview.
Measures
Our dependent variable, leverage, had four categories: no leverage; social welfare leverage only (i.e., leverage involving money or housing); legal leverage only (outpatient commitment or leverage applied through the criminal justice system); and both types of leverage.
We used the MacArthur Community Violence Interview (3 , 25) to assess violent and aggressive behavior on the part of study participants during the previous 6 months. Violent acts were then categorized into two levels of severity: “serious violence,” which included any assault that resulted in injury or in which a lethal weapon was used, any threat made with a lethal weapon in hand, and any sexual assault; and “other aggressive acts,” which included simple assault without injury or use of a weapon. We also created a summary variable, “any physically assaultive behavior,” which includes both serious violence and other aggressive acts.
Chart diagnoses were used to record participants’ primary psychiatric disorder. In our analyses, we compared psychotic disorders with all other disorders. Substance use was assessed with the four-item CAGE questionnaire (26) on alcohol use, and the same questions were adapted to ask about drug use. In our analyses, we combined alcohol and drug abuse into a single dichotomous variable to indicate either “one or more symptoms of a substance use disorder” or “no symptoms of a substance use disorder.”
The Brief Psychiatric Rating Scale (BPRS) (27) was used to assess current psychiatric symptoms; possible scores range from 0 to 126, with higher scores indicating more symptoms and greater severity. The Global Assessment of Functioning scale (GAF) was used to assess current functioning; possible scores range from 0 to 100, with higher scores indicating higher levels of functioning. The Insight and Treatment Attitudes Questionnaire (28) , an 11-item rating scale, was used to measure awareness of mental health problems and acknowledgment of the need for treatment in the past, currently, and in the future; possible scores range from 0 to 22, with higher scores indicating greater awareness of illness and acceptance of need for treatment. An item from the Drug Attitudes Inventory asked whether respondents took psychiatric medication of their own free choice. Continuous variables were dichotomized into high and low categories (above the median and less than or equal to the median) because of skewed distributions and to capture nonlinear associations (29) . Our selection of independent variables and grouping of covariates into domains were based on prior clinical and epidemiological studies of risk factors related to violence and other outcomes for persons with severe mental illness (3 , 15 , 30 , 31) .
Statistical Analysis
Multinomial logit analysis was used to examine the association between physically assaultive behavior and experience of social welfare leverage, legal leverage, or both types of leverage, controlling for a variety of demographic and clinical characteristics. Relative risk ratios were computed for each category of violence to express the likelihood of subjects’ being in each leverage category compared with no leverage. All statistical tests were adjusted to account for our pooled sample. Site was modeled as a fixed effect, with a robust variance estimator to account for clustering of observations by site. Stata 8.2 (32) was used for all analyses.
Results
Participant Characteristics
Across the five sites, 1,011 participants were included in the study. The proportion of all respondents who reported having engaged in serious violence during the previous 6 months ranged from 3.4% to 8.5% across the sites, and the proportion who reported having engaged in any physically assaultive behavior ranged from 18.3% to 21.0%. Participants’ mean age ranged from 41.3 to 46.7 years across the sites. The proportion of male participants ranged from 32.4% to 64.5%, and the proportion of nonwhite racial groups ranged from 28.5% to 64.0%. Schizophrenia or another psychotic disorder was the primary psychiatric chart diagnosis for 41.5% to 49.5% of respondents. Rates of comorbid substance use ranged from 13.9% to 35.5%. Mean BPRS scores ranged from 31 to 33, indicating that, on average, these were moderately symptomatic patients. Meant GAF scores were in the range of 42 to 56, indicating moderate to serious impairment of functioning on average. Mean scores on the Insight and Treatment Attitudes Questionnaire were consistent across sites, with relatively high levels of awareness of need for treatment and for medication.
The average number of years in treatment ranged from 19 to 23 years across sites; 47.6% to 63.3% of respondents reported four or more lifetime hospitalizations, and 24.6% to 85.2% of respondents had more than three outpatient visits per month. Large majorities of respondents (74.4% to 87.2%) indicated that they took medication of their own free will.
Types of Leverage Reported
The proportion of respondents reporting no experience of the various types of leverage ranged from 41.0% to 55.9% across the sites. Experience of social welfare leverage alone was reported by 15.7% to 26.3% of respondents, legal leverage alone by 11.2% to 17.0%, and both types by 12.8% to 18.5%.
Correlates of Leverage Types
Table 1 presents the participants’ assaultive, demographic, and clinical characteristics by type of leverage, along with the statistical significance of associations as determined by chi-square tests. A Bonferroni adjustment for multiple comparisons reduced the threshold for statistical significance to a p value of 0.001. Participants who had experienced legal leverage only and those who had experienced both legal and social welfare leverage had significantly higher rates of serious violence than those who had experienced no leverage. We found no associations between any of the leverage categories and the category of other aggressive acts only.
Prevalence of Leveraged Treatment by Violent Behavior
Leveraged treatment was significantly more common among the 56 participants who reported serious violence than among the 955 respondents who did not report serious violence (73.1% versus 50.1%; Fisher"s exact test, p 0.001). However, the prevalence of leveraged treatment did not significantly differ between the 143 participants reporting only other aggressive acts and the 812 participants reporting no violence or other aggressive acts (50.0% versus 50.1%).
Multivariable Models
We used multinomial logit regression to test multivariable associations. Tables 2 , 3 , and 4 present models assessing the effects on type of leverage associated with serious violence, with other aggressive acts only, and with any physically assaultive behavior, respectively. Models also controlled for site and the clustering of observations within sites. Participants who reported any physically assaultive behavior were significantly more likely to have experienced both legal and social welfare leverage, compared with no leverage. However, neither type of leverage alone was associated with the category of any physically assaultive behavior ( Table 4 ). Serious violence was significantly associated with having experienced legal leverage alone but not with experience of social welfare leverage alone or of both types of leverage ( Table 2 ).
These models also permit examination of the net effects on leverage associated with demographic and clinical covariates, with the effects of violence held constant. The effects of covariates were consistent across analyses, irrespective of the severity of violence, as shown in Tables 2 , 3 , and 4 . Significant predictors of social welfare leverage alone included white race, four or more prior hospitalizations, and more than three outpatient mental health visits per month. For legal leverage alone, significant effects were younger age, male gender, longer time in treatment (21 years or more), four or more prior hospitalizations, and not taking psychiatric medication voluntarily. For both leverages together, significant effects were younger age, male gender, a low GAF score (≤47), longer time in treatment, four or more prior hospitalizations, more than three outpatient mental health visits per month, and not taking psychiatric medication voluntarily.
Voluntary Medication Adherence, Violence, and Leveraged Treatment
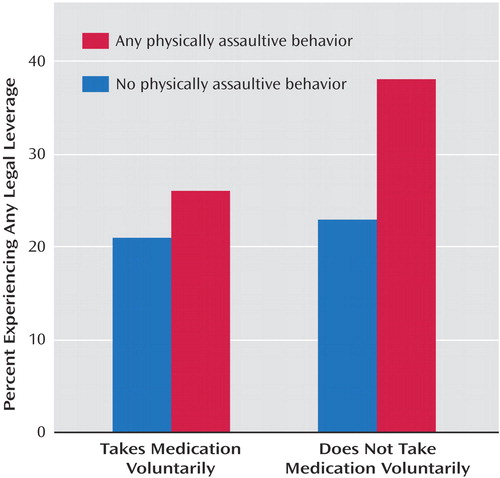
Does voluntary adherence to medication moderate the effect of any physically assaultive behavior on the likelihood of experiencing treatment leverage? Is the combination of medication refusal and any physically assaultive behavior more likely to result in the application of leverage than either of these conditions alone? To test this potential interaction, we coded respondents into four groups according to whether they reported any physically assaultive behavior and whether they reported that they took psychiatric medication of their own free choice: not violent, takes medication voluntarily; not violent, does not take medication voluntarily; violent, takes medication voluntarily; and violent, does not take medication voluntarily. We then examined the relative risk of having experienced any legal leverage and any social welfare leverage in the latter three groups compared with the first group (results not shown). (We were unable to examine the combination of having experienced legal and social welfare leverage in this interaction model because of inadequate statistical power.)
Among respondents who reported that they took medication voluntarily, assaultive behavior was not associated with a significantly greater likelihood of having experienced legal or social welfare leverage. Likewise, among respondents who did not report any physically assaultive behavior, not taking medication voluntarily was not associated with a greater likelihood of having experienced either type of leverage. However, those who reported any physically assaultive behavior and also did not take medication voluntarily were more than twice as likely to have experienced legal leverage (odds ratio=2.6, p<0.001), although they were not more likely to have experienced social welfare leverage. Figure 1 illustrates the interaction effect of any physically assaultive behavior with voluntary medication adherence on experience of legal leverage.
Discussion
In this study, we explored the link between risk of violence and use of legal and social welfare system leverage to improve adherence to community-based treatment among people with mental illness. We found that serious violence was infrequent among psychiatric patients who were subjected to mandated community treatment and other forms of leveraged treatment. However, in our multivariable analysis, we found that serious violence was associated with a significantly greater likelihood of having experienced legal leverage. We also found that any physically assaultive behavior—a summary variable that included serious violence as well as any other aggressive acts (defined as any simple assault without a weapon or causing injury)—was associated with a greater likelihood of having experienced both legal and social welfare leverage. Committing other aggressive acts only was not associated with experience of leveraged treatment.
An interaction model showed that committing any physically assaultive behavior was significantly associated with having experienced legal leverage, but only among participants who did not voluntarily take psychotropic medication. This finding suggests that a combination of concerns about safety and nonadherence to treatment may influence clinicians and judges to apply legal leverage; even minor assaultiveness may raise concern about psychiatric patients who are unwilling to take prescribed medication.
We also found that certain demographic and clinical factors were independently associated with a greater likelihood of having experienced both types of leverage. These include younger age, male gender, poorer clinical functioning, more years in treatment, more frequent hospitalizations, higher frequency of outpatient visits, and negative attitudes toward medication adherence.
Whether leveraged community treatment may be suitable for violence-prone individuals with mental disorders may depend on what forms of leverage are available; and whether a given type of leverage is appropriate may in turn depend on the nature and severity of the violent behavior. In any case, the application of leverage is intended primarily to improve the effectiveness of treatment, not to reduce the risk of violence per se, and hence the mandated treatment should address the needs of the person involved.
This study had several limitations. The five sites were not randomly sampled, and thus our findings cannot be generalized to all persons in treatment for mental disorders. Also, in a cross-sectional survey, it is impossible to determine temporal or causal ordering in associations between recent violence (past 6 months) and lifetime experience of leveraged treatment. Likewise, we cannot make inferences about the specific pathways leading to the application of leverage and the role of violence in these pathways. However, our results at least suggest that the combination of a risk of violence and a negative attitude toward medication adherence play an important synergistic role in the application of leverage. Persons with mental illness in whom these two problems occur jointly may be particularly challenging to engage in effective treatment, which may lead to attempts to apply leverage to encourage treatment adherence.
Because our findings also indicate that a number of other clinical characteristics are associated with experience of leverage, we would caution against overinterpreting the association of violence and leverage; violent behavior may serve as a proxy measure for other factors related to clinical acuity, social-environmental barriers to care, or unspecified difficulties with treatment engagement. Alternatively, it is possible that the experience of leverage, in combination with other risk factors, increases the risk of assaultive behavior. Research has shown that among persons with severe mental illness who have frequent contact with their families, a family representative payee arrangement is associated with a nearly threefold increase in risk of violence (17) .
The finding that individuals who report violent behavior are more likely to have experienced legal leverage is not surprising, given that involuntary outpatient commitment, one form of legal leverage, has drawn the attention of policy makers seeking an effective mechanism for reducing the risk of violence among persons with severe mental illness. Insofar as self-reported recent violence stands as a rough indicator of lifetime history of violence, it would appear that violence-prone individuals account for only a small proportion of all cases of legal leverage. Any such conclusion must remain tentative, however, because we do not know how many of the respondents who reported having experienced leveraged treatment were also violent at some time in the past, but not in the past 6 months—perhaps as a result of having received leveraged community treatment. For example, Swanson and colleagues (11) found that sustained outpatient commitment with regular use of outpatient services was associated with a 50% reduction in the probability of any violent behavior in a sample of involuntarily hospitalized patients released under outpatient commitment. In any case, the advantages and drawbacks of using legal leverage must be evaluated with a broader range of persons with severe mental illness—not only those who have recently been violent.
The notion that people with mental illness are almost never violent is a core tenet of the movement to destigmatize psychiatric illness, to treat it like any other serious medical problem, and to resist any abridgment of the human rights of psychiatric patients. That people with mental illness occasionally do commit violent acts as a result of untreated serious psychopathology—often with grim consequences to themselves and others—is a core tenet of the movement to extend legally mandated outpatient psychiatric treatment. At the intersection of these two arguments about civil rights and public safety, a moderate position might hold that in community-based mental health care, leverage, like violence, is not entirely avoidable but should be rare.
1. Monahan J, Bonnie RJ, Appelbaum PS, Hyde PS, Steadman HJ, Swartz MS: Mandated community treatment: beyond outpatient commitment. Psychiatr Serv 2001; 52:1198–1205Google Scholar
2. Swartz MS, Swanson JW: Involuntary outpatient commitment in the United States: practice and controversy, in Care for the Mentally Disordered Offender in the Community. Edited by Buchanan A. Oxford, UK, Oxford University Press, 2002, 199–221Google Scholar
3. Steadman HJ, Mulvey EP, Monahan J, Robbins PC, Appelbaum PS, Grisso T, Roth LH, Silver E: Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry 1998; 55:393–401Google Scholar
4. Phelan JC, Link BG: Fear of people with mental illnesses: the role of personal and impersonal contact and exposure to threat or harm. J Health Soc Behav 2004; 45:68–81Google Scholar
5. Van Dorn RA, Swanson JW, Elbogen EB, Swartz MS: A comparison of stigmatizing attitudes toward persons with schizophrenia in four stakeholder groups: perceived likelihood of violence and desire for social distance. Psychiatry 2005; 68:152–163Google Scholar
6. Corrigan PW, Watson AC, Warpinski AC, Gracia G: Implications of educating the public on mental illness, violence, and stigma. Psychiatr Serv 2004; 55:577–580Google Scholar
7. Pescosolido BA, Monahan J, Link BG, Stueve A, Kikuzawa S: The public’s view of the competence, dangerousness, and need for legal coercion of persons with mental health problems. Am J Public Health 1999; 89:1339–1345Google Scholar
8. Appelbaum P: Thinking carefully about outpatient commitment. Psychiatr Serv 2001; 52:347–350Google Scholar
9. Steadman HJ, Gounis K, Dennis D, Hopper K, Roche B, Swartz M, Robbins PC: Assessing the New York City involuntary outpatient commitment pilot program. Psychiatr Serv 2001; 52:330–336Google Scholar
10. Swartz MS, Swanson JW, Wagner HR, Burns BJ, Hiday VA, Borum R: Can involuntary outpatient commitment reduce hospital recidivism? findings from a randomized trial with severely mentally ill individuals. Am J Psychiatry 1999; 156:1968–1975Google Scholar
11. Swanson JW, Swartz MS, Borum R, Hiday VA, Wagner HR, Burns BJ: Involuntary out-patient commitment and reduction of violent behaviour in persons with severe mental illness. Br J Psychiatry 2000; 176:324–331Google Scholar
12. Monahan J, Swartz MS, Bonnie R: Mandated treatment in the community for people with mental disorders. Health Aff 2003; 22:28–38Google Scholar
13. Elbogen EB, Swanson JW, Swartz MS: Psychiatric disability, the use of financial leverage, and perceived coercion in mental health services. Int J Forensic Ment Health 2003; 2:119–127Google Scholar
14. Elbogen EB, Soriano C, Van Dorn RA, Swartz MS, Swanson JW: Consumer views of representative payee use of disability funds to leverage treatment adherence. Psychiatr Serv 2005; 56:45–49Google Scholar
15. Swanson J, Estroff S, Swartz M, Borum R, Lachicotte W, Zimmer C, Wagner R: Violence and severe mental disorder in clinical and community populations: the effects of psychotic symptoms, comorbidity, and lack of treatment. Psychiatry 1997; 60:1–22Google Scholar
16. Estroff SE, Swanson JW, Lachicotte WS, Swartz M, Bolduc M: Risk reconsidered: targets of violence in the social networks of people with serious psychiatric disorders. Soc Psychiatry Psychiatr Epidemiol 1998; 33(suppl 1):S95–S101Google Scholar
17. Elbogen EB, Swanson JW, Swartz MS, Van Dorn RA: Family representative payeeship and violence risk in severe mental illness. Law Hum Behav 2005; 29:563–574Google Scholar
18. Allen M: Waking Rip Van Winkle: why developments in the last 20 years should teach the mental health system not to use housing as a tool of coercion. Behav Sci Law 2003; 21:503–521Google Scholar
19. Monahan J, Redlich A, Swanson JW, Robbins PC, Appelbaum PS, Petrila J, Steadman HJ, Swartz MS, Angell B, McNiel DE: Use of leverage to improve adherence to psychiatric treatment in the community. Psychiatr Serv 2005; 56:37–44Google Scholar
20. Swanson JW, Swartz MS, Essock SM, Osher FC, Wagner HR, Goodman LA, Rosenberg SD, Meador KG: The social-environmental context of violent behavior in persons treated for severe mental illness. Am J Public Health 2002; 92:1523–1531Google Scholar
21. Skeem J, Petrila J: Problem-solving supervision: specialty probation for individuals with mental illness. Court Rev 2004; 40:8–15Google Scholar
22. Skeem JL, Encandela J, Eno-Louden J: Experiences of mandated mental health treatment in traditional and specialty probation programs. Behav Sci Law 2003; 21:429–458Google Scholar
23. Redlich AD, Steadman HJ, Monahan J, Petrila J, Griffin PA: The second generation of mental health courts. Psychol Public Policy Law 2005; 11:527–538Google Scholar
24. Griffin PA, Steadman HJ, Petrila J: The use of criminal charges and sanctions in mental health courts. Psychiatr Serv 2002; 53:1285–1289Google Scholar
25. Monahan J, Steadman H, Silver E, Appelbaum P, Robbins P, Mulvey E, Roth L, Grisso T, Banks S: Rethinking Risk Assessment: The MacArthur Study of Mental Disorder and Violence. New York: Oxford University Press, 2001Google Scholar
26. Allen JP, Eckardt MJ, Wallen J: Screening for alcoholism: techniques and issues. Public Health Rep 1988; 103:586–592Google Scholar
27. Moerner MG, Mannuzza S, Kane JM: Anchoring the BPRS: an aid to improved reliability. Psychopharmacol Bull 1988; 24:112–117Google Scholar
28. McEvoy JP, Apperson LJ, Appelbaum PS, Ortlip P, Brecosky J, Hammill K, Geller JL, Roth L: Insight in schizophrenia: its relationship to acute psychopathology. J Nerv Ment Dis 1989; 177:43–47Google Scholar
29. Farrington DP, Loeber R: Some benefits of dichotomization in psychiatric and criminological research. Crim Behav Ment Health 2000; 10:100–122Google Scholar
30. Monahan J, Steadman H (eds): Violence and Mental Disorder: Developments in Risk Assessment. Chicago, University of Chicago Press, 1994Google Scholar
31. Swanson JW, Swartz MS, Van Dorn RA, Elbogen EB, Wagner HR, Rosenheck RA, Stroup TS, McEvoy JP, Lieberman JA: A national study of violent behavior in persons with schizophrenia. Arch Gen Psychiatry 2006; 63:490–499Google Scholar
32. StataCorp: Stata Statistical Software, Release 8.0. College Station, Tex, StataCorp, 2003Google Scholar