The Importance of Routine for Preventing Recurrence in Bipolar Disorder
A 41-year-old divorced woman with a 17-year history of bipolar I disorder is receiving outpatient treatment consisting of lithium pharmacotherapy and psychotherapy. She is currently living with her sons, ages 7 and 9. Her history is notable for several onsets of mania during or immediately following vacation travel. By the time the patient entered treatment with her current therapist, she was vacation phobic. Yet, as the now-single mother of two active young boys, she also recognized how much she would benefit from a change of scenery and some relief from the constant responsibility for her children and her home. Her brother and sister-in-law had offered to send to her a ticket out to the West Coast for a visit. As much as the idea of a vacation with them appealed to her, it also terrified her. When she mentioned the possibility to her psychiatrist, he agreed that there were some risks involved but that if she planned carefully, she might be able to minimize those risks.
The Scope and Nature of the Problem
How important is regularity of routine for patients with bipolar disorder? What risks are associated with disruption in normal routines or changes in the level of external stimulation and novelty? How can planned changes in routine be managed so as not to destabilize the patient?
Risk of Recurrence in Bipolar Disorder
Far from being psychiatry’s “good prognosis disorder,” bipolar disorder is characterized by frequent recurrence (1 , 2) , incomplete interepisode recovery (3 , 4) , and poor interepisode functioning (4) . The challenges associated with the management of bipolar disorder are not simply the treatment of acute episodes of mania and depression but also prevention of syndromal recurrence and assurance of full interepisode recovery—both symptomatic and functional. For example, a man suffering from bipolar disorder who quits a highly stressful full-time job may then demonstrate only minimal depressive symptoms. However, he may then be left with chronic understimulation (as opposed to stress and overstimulation) and lack of any daily routine. This, coupled with lower quality of life as a result of reduced economic circumstances and reduced self-esteem as a result of the loss of a defining social role can lay the groundwork for a long and unremitting period of minor depression associated with marked functional impairment across all life roles. Remaining mindful of the need to prevent episodes, while encouraging patients to strive for fully satisfying lives, is a challenge confronting most clinicians working with patients who suffer from bipolar disorder.
Association of Bipolar Recurrence With Disruption in Routine
In their classic textbook on manic-depressive illness, Goodwin and Jamison (5) argued that an integrated theory of bipolar disorder can be based on an “instability model.” Indeed, they postulate that instability is “the fundamental dysfunction in manic depressive illness” (p. 594).
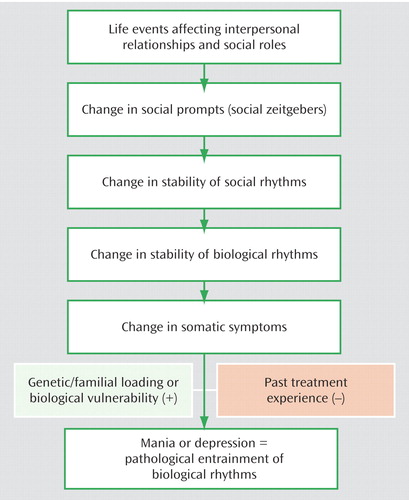
A key component implicating rhythm disruption in the pathophysiology of bipolar episodes is empirical data relating the changes in duration and architecture of sleep observed in both depression and mania to the pathophysiology of the disorder (6 , 7) . In formulating their model of bipolar disorder, both Wehr and Goodwin (6) and Kupfer et al. (7) sought to place these sleep changes in the broader context of the pervasive circadian disturbance hypothesized in bipolar disorder, which includes changes in 24-hour patterns of cortisol and other neurohormones. They also noted the importance of exogenous challenges to the circadian system—such as travel across time zones—in the precipitation of new episodes of illness. The work of Ehlers et al. (8 , 9) therefore emphasized the relationship between psychosocial stressors (and, equally important, non-“stressful” alterations in the patterning of daily life) and changes in biological rhythms. Changes in an individual’s routines that are apparently benign from a psychological stress standpoint can place considerable stress on the body’s attempt to maintain synchronized sleep/wake, appetite, energy, and alertness rhythms. A weekend vacation or starting a regular exercise program typically alters usual routines in ways that clearly affect what Ehlers et al. refer to as social rhythms and may, in turn, affect circadian rhythms.
Environmental factors that set the circadian clock are referred to as zeitgebers or “time givers” (10) . The primary and most powerful zeitgeber is the rising and setting of the sun, a physical zeitgeber. However, especially in urban, industrialized society, social factors such as the timing of work, meals, and other daily routines play an important role in establishing circadian rhythms. According to the social zeitgeber hypothesis, in vulnerable individuals (i.e., those with a mood disorder diathesis), changes in social time cues can lead to disruptions in circadian rhythms and ultimately to new mood episodes (9 , 10) . It is also argued that certain kinds of life events, such as having friends come to stay for the weekend or bringing a new baby into the family, act as a zeitstörer, or active disrupter of one’s social and, probably, circadian rhythms (9) .
How the body’s clock becomes disrupted in patients with mood disorders remains unclear. Exposure to light or day length appears to play a role in the etiology and treatment of seasonal affective disorders (11) , possibly through their capacity to synchronize rhythms. However, studies in nonseasonal depression have not demonstrated that light is a primary synchronizing force in these patients’ illnesses (12) . To date, little is known about how physical zeitgebers such as light exposure and social zeitgebers might interact, making it difficult to assess the relative importance of their roles in biological rhythm regulation.
In the Ehlers et al. model of the illness, individuals who are at high risk for mood disorder, as a result of either a family or personal history of affective disorder, are more likely to move along the theoretical path, illustrated in Figure 1 , to the manic or depressed state that is its endpoint. Subsequent to the publication of this hypothesis, Malkoff-Schwartz et al. (13 , 14) conducted studies demonstrating that life events that disrupt social rhythms are strongly associated with the onset of manic episodes and more modestly associated with depressive onsets in individuals with a history of bipolar I disorder. More recently, Frank et al. have shown that, as predicted, those who engage in treatment aimed specifically at helping patients with a history of bipolar disorder to maintain regular routines in the face of such events are protected from new onsets of mania and depression (15) .
Treatment and Management
Risk Factors for Recurrence
Disruption in routines represents only one of a host of risk factors for recurrence of mania or depression. Each individual patient who suffers from bipolar disorder appears to have his or her own particular complex of risk factors, many of which may interact with one another. For example, nonadherence to mood stabilizing medication is a key risk factor for recurrence in almost all individuals who suffer from bipolar I disorder. However, both psychosocial stress and disruption in normal routines are often associated with a failure or inability to adhere to an established pharmacotherapy regimen. Cognitive and interpersonal overstimulation, of the kind that is likely to occur in situations such as starting a new job or a new relationship, attending a conference or convention, or taking part in a family vacation, can be a risk factor for onset of mania in some individuals. Likewise, lack of stimulation, such as that experienced during the summer by someone who has a 9-month school-year job or by someone who is laid off from work, can lead to depression onset.
Treatment Aimed at Recurrence Prevention: Psychoeducation and Psychotherapy
In the last decade of the 20th century, clinical investigators were finding high rates of recurrence in the newer studies of pharmacotherapy alone (1) and began to explore the potential benefits of adding a psychoeducational or psychotherapeutic intervention to pharmacotherapy in the prevention of bipolar recurrence. The assumption was that, if nothing else, psychotherapy might improve the generally poor adherence to pharmacotherapy observed in this patient population. The hope was, however, that a psychotherapeutic approach might have benefits, including enhancing social and occupational functioning, enhancing capacity to manage stressors in the social/occupational milieu, enhancing the protective effects of family and other social supports, decreasing denial and disorder-associated trauma, and encouraging acceptance of the disorder.
Data from controlled clinical trials now exist supporting individual psychoeducation (16) , group psychoeducation (17) , several variants of cognitive therapy (18 – 20) , family-focused treatment (21 , 22) , and an adaptation of interpersonal psychotherapy (15 , 23) as adjuncts to pharmacotherapy in the prevention of recurrence. The psychoeducational approaches tend to emphasize education about the disorder itself and about the treatments used to manage it along with a strong focus on the recognition of early warning signs of impending episodes and the development of an action plan when these early warning signs are present. The cognitive approaches have tended to adhere fairly closely to Beck et al.’s model (24) in the treatment and prevention of depressive episodes, with additional components to address the cognitive distortions associated with mania and hypomania and negative cognitions related to “dependence” on medication. The family-focused approach of Miklowitz and Goldstein (25) grew out of data indicating the negative impact of a family environment characterized by criticism and emotional overinvolvement in provoking bipolar recurrences. The treatment, therefore, emphasizes education of all family members regarding the disorder and training in positive and productive communication.
Our own research group, with its strong interest in the relationship of the circadian system to mood disorders, developed an intervention aimed at prevention of recurrence that we called interpersonal and social rhythm therapy (23) . Our idea was that a behavioral approach aimed at increasing the regularity of patients’ daily routines, and especially their sleep/wake cycles, could shore up what we viewed as their vulnerable circadian systems. In the behavioral component of this intervention we first assess, using a self-report charting device called the Social Rhythm Metric, the extent to which a patient’s routines vary in their timing from day to day (see Figure 2 ). We put particular emphasis on the timing of going to bed, rising, work, meals, and social contact. Then, again using the Social Rhythm Metric as a guide, we work with the patient to help him or her to make those routines more regular in their timing. Using behavioral strategies such as chain analysis and successive approximation, we seek to have the timing of those key activities vary by no more than an hour. We also search the “landscape” of the patient’s life for potential triggers to rhythm disruption, such as having house guests or taking a vacation. We then problem-solve with the patient about how to maintain the maximum regularity of routine possible in the face of such disruptions. By weaving this approach together with work on the four problem areas (grief, role transitions, role disputes, and interpersonal deficits) specified in interpersonal psychotherapy as developed for unipolar disorder by Klerman and colleagues (26) , we hoped to protect the vulnerable circadian systems of individuals with bipolar disorder, improve their acceptance of the illness, decrease interpersonal and social role distress, and improve social role functioning. In a controlled trial of 175 patients with bipolar I disorder, we have now shown that acute treatment with interpersonal and social rhythm therapy is associated with significantly reduced risk of recurrence of both depression and mania over a subsequent 2-year period (23) . Furthermore, we found that the protective effect of the treatment was directly related to the extent to which patients increased the regularity of their social rhythms.

Summary and Recommendations
Using the approach formulated in interpersonal and social rhythm therapy (15 , 23) as it might apply to the case of the patient described in the opening vignette, one would first have to establish the importance of regularity in the patient’s daily routines, especially her sleep/wake cycle, in prevention of new episodes of illness. She would then be encouraged to address planned changes in her routine, such as the vacation under discussion, with clear knowledge of the importance of maintaining her social rhythms, adequate sleep, and appropriate levels of stimulation in addition to careful adherence to her pharmacotherapy. The specific aspects of vacation-taking and resultant effects on routine that may have precipitated her past manic episodes should be examined. For the patient in question, it seems to have been a combination of travel across time zones and overstimulation. For other individuals, it may be the stress associated with the interpersonal intensity and criticism that sometimes accompanies a family vacation, rather than a shift in routine, that precipitates new mood episodes.
Risk of recurrence must be considered ever present in patients with well-established histories of bipolar I disorder. The psychiatrist’s role in preventing recurrence includes taking a careful history that elucidates the individual patient’s unique risk factors for new episodes, educating the patient about those risk factors and how to recognize them, providing appropriate prophylactic pharmacotherapy, and, if not offering a bipolar disorder-specific form of psychotherapy, at least problem-solving with the patient about how to manage his or her own particular risks of new episodes.
1. Markar HR, Mander AJ: Efficacy of lithium prophylaxis in clinical practice. Br J Psychiatry 1989; 155:496–500Google Scholar
2. Angst J, Gamma A, Sellaro R, Lavori P, Zhang H: Recurrence of bipolar disorders and major depression: a life-long perspective. Eur Arch Psychiatry Clin Neurosci 2003; 253:236–240Google Scholar
3. Coryell W, Keller M, Endicott J, Andreasen NC, Clayton P, Hirschfeld R: Bipolar II illness: course and outcome over a five-year period. Psychol Med 1989; 19:129–141Google Scholar
4. Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser J, Solomon D, Leon AC, Rice JA, Keller MB: The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry 2002; 59:530–537Google Scholar
5. Goodwin FK, Jamison KR: Manic-Depressive Illness, Oxford University Press, 1990Google Scholar
6. Wehr TA, Goodwin FK: Biological rhythms in manic-depressive illness, in Circadian Rhythms in Psychiatry, Psychobiology and Psychopathology, vol 2. Edited by Wehr TA, Goodwin FK. Pacific Grove, Calif, Boxwood Press, 1983, pp 129–184Google Scholar
7. Kupfer DJ, Foster FG, Detre TP: Sleep continuity changes in depression. Dis Nerv Syst 1973; 34:192–195Google Scholar
8. Ehlers CL, Frank E, Kupfer DJ: Social zeitgebers and biological rhythms: a unified approach to understanding the etiology of depression. Arch Gen Psychiatry 1988; 45:948–952Google Scholar
9. Ehlers CL, Kupfer DJ, Frank E, Monk TH: Biological rhythms and depression: the role of zeitgebers and zeitstorers. Depression 1993; 1:285–293Google Scholar
10. Aschoff J: Handbook of Behavioral Neurobiology. New York, Plenum Press, 1981Google Scholar
11. Lewy AJ, Sack RL, Singer CM: Treating phase typed chronobiological sleep and mood disorders using appropriately timed bright artificial light. Psychopharmacol Bull 1985; 21:368–372Google Scholar
12. Mendelson WB, James SP, Rosenthal NE, Sack DA, Wehr TA, Garnett D, Weingartner H: The experience of insomnia, in Biological Psychiatry 1985: Proceedings of the IVth World Congress of Biological Psychiatry. Edited by Shagass C, Josiassen RC, Bridger WH, Weiss KJ, Stoff D, Simpson GM. New York, Elsevier, 1986, pp 1005–1006Google Scholar
13. Malkoff-Schwartz S, Frank E, Anderson B, Sherrill JT, Siegel L, Patterson D, Kupfer DJ: Stressful life events and social rhythm disruption in the onset of manic and depressive bipolar episodes: a preliminary investigation. Arch Gen Psychiatry 1998; 8:702–707Google Scholar
14. Malkoff-Schwartz S, Frank E, Anderson BP, Hlastala SA, Luther JF, Sherrill JT, Houck PR, Kupfer DJ: Social rhythm disruption and stressful life events in the onset of bipolar and unipolar episodes. Psychol Med 2000; 30:1005–1016Google Scholar
15. Frank E, Kupfer DJ, Thase ME, Mallinger AG, Swartz H, Fagiolini AM, Grochocinski V, Houck P, Scott J, Thompson W, Monk T: Two year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Arch Gen Psychiatry 2005; 62:996–1004Google Scholar
16. Perry A, Tarrier N, Morriss R, McCarthy E, Limb K: Randomized controlled trial of efficacy of teaching patients with bipolar disorder to identify early symptoms of relapse and obtain treatment. BMJ (clinical research ed) 1999; 318(7177):149–153Google Scholar
17. Colom F, Vieta E, Martinez-Aran A, Reinares M, Goikolea JM, Benabarre A, Torrent C, Comes M, Corbella B, Parramon G, Corominas J: A randomized trial on the efficacy of group psychoeducation in the prophylaxis of recurrences in bipolar patients whose disease is in remission. Arch Gen Psychiatry 2003; 60:402–407Google Scholar
18. Lam DH, Jones SH, Hayward P, Bright JA: Cognitive Therapy for Bipolar Disorder. Chichester, John Wiley & Sons, 1999Google Scholar
19. Lam DH, Watkins ER, Hayward P, Bright J, Wright K, Kerr N, Parr-Davis G, Sham P: A randomized controlled study of cognitive therapy for relapse prevention for bipolar affective disorder: outcome of the first year. Arch Gen Psychiatry 2003; 60:145–152Google Scholar
20. Scott J, Garland A, Moorhead S: A pilot study of cognitive therapy in bipolar disorders. Psychol Med 2001; 31:459–467Google Scholar
21. Miklowitz DJ, Simoneau TL, George EL: Family-focused treatment of bipolar disorder: 1-year effects of a psychoeducational program in conjunction with pharmacotherapy. Biol Psychiatry 2000; 48:582–592Google Scholar
22. Rea MM, Tompson M, Miklowitz DJ, Goldstein MJ, Hwang S, Mintz J: Family-focused treatment versus individual treatment for bipolar disorder: results of a randomized clinical trial. J Consult Clin Psychol. 2003; 71:482–492Google Scholar
23. Frank E: Treating Bipolar Disorder: A Clinician’s Guide to Interpersonal and Social Rhythm Therapy. New York, Guilford, 2005Google Scholar
24. Beck AT, Rush AJ, Shaw BF, Emery G: Cognitive Therapy of Depression: A Treatment Manual. New York, Guilford, 1979Google Scholar
25. Miklowitz DJ, Goldstein MJ: Behavioral family treatment for patients with bipolar affective disorder. Behav Modif 1990; 14:457–489Google Scholar
26. Klerman GL, Weissman M, Rounsaville BJ, Chevron ES: Interpersonal Psychotherapy of Depression. New York, Basic Books, 1984Google Scholar



