Neuroscience in Psychiatry Training: How Much Do Residents Need To Know?
Abstract
Objective: With the explosion of research in psychiatric neuroscience, the extent and means by which neuroscientific progress will translate into clinical care remains largely uncertain. The authors sought to determine how this dilemma is currently being played out in residency training programs, in which training directors must decide how best to integrate neuroscience teaching in a rapidly changing clinical landscape. Method: The authors surveyed U.S. and Canadian psychiatry residency training directors to characterize current and future trends in neuroscience education and to examine training directors’ views on the relevance of neuroscience to clinical practice. Results: The amount of neuroscience in residency curricula has increased significantly over the past 5 years, and further increases are expected in each specific neuroscience content area examined. While most training directors agreed that training in neuroscience was important for all residents, even those becoming primarily psychotherapists, relevance to future (but not current) practice was consistently cited as a motivating factor. Conclusions: While psychiatric residency programs continue to increase the neuroscience content of their curricula, it remains unclear how this added training will influence clinical work. Reframing current practices, including psychotherapy, into a neuroscientific context may ultimately prove more useful to trainees.
Psychiatry residency training programs face the difficult burden of balancing a wide-ranging curriculum while preparing trainees for practice in a rapidly evolving field. The history of psychiatry is replete with examples of philosophical changes in the field substantially preceding changes in clinical practice (1 – 4) . As a consequence, the pendulum of research and technique has often swung to an opposite pole with each new strong influence. Training directors must often predict which changes will be most important to teach and must do so in the setting of limited time for study and didactics. For instance, in the 1970s, some training programs apologized to residents when they took time away from psychotherapy education to teach psychopharmacology (5) .
We are presently in the midst of another strong paradigm change, one that stems from the many advances in neuroscience. Neuroimaging research has begun to elucidate the biological basis of complex behaviors in both healthy individuals and those with psychiatric disorders (6 , 7) . Pharmacologists have provided cellular and molecular contexts for psychopathology and have suggested targeted approaches for treatment (8 , 9) . While still in its infancy, psychiatric genomics shows significant promise for anticipating disease risk and planning treatment (10) . However, not all findings from such preclinical and clinical neuroscience studies are relevant for the practice of psychiatry now (11) , and many may not be in the future (12) .
Furthermore, psychiatry’s focus is more than the sum of its molecules. Several scientifically rigorous randomized controlled studies and meta-analyses have upheld the clinical utility and efficacy of various forms of psychotherapy (13 – 15) , even without detailed knowledge about their effects on brain function (16) . Training directors must struggle with this mind/brain balance in the setting of limited time for didactic training.
From the perspective of psychiatry residents, the disconnect between theory and practice can be equally frustrating. Residents frequently question the clinical utility of neuroscience-related lectures. While it is easy for them to understand that brain and behavior are related through physiology, biochemistry, and neuroanatomy, it is often difficult to appreciate how these relationships come into play when sitting with a patient. The common refrain, “We know it is important, we just do not know why ,” is heard after many neuroscience talks. In the same vein, residents are expected to become increasingly familiar with the neuroscientific principles described in clinical journals. However, it remains unclear whether residents have sufficient knowledge and experience to stay abreast of the literature after they complete their training. Furthermore, discussions among the 20 U.S. and Canadian residents comprising the APA/GlaxoSmithKline Fellowship (formerly the Falk Fellowship) revealed substantial variation in what each respective training program deemed important in the neuroscience curriculum, and why.
Given the varied scope of psychiatric practice today (where the same training programs will produce psychopharmacologists, therapists, and researchers across a host of specialties) as well as the uncertain future of practice patterns in psychiatry, we were interested in how residency training directors decide which neuroscientific concepts are appropriate and relevant. To better define the present role of neuroscience education in psychiatry residency curricula, we surveyed training directors in the United States and Canada with the following four domains in mind. First, who teaches residents about the neurosciences, and in what settings? Second, what themes comprise the focus of neuroscience teaching, and how have these themes changed over time? Third, does the need to convey an ever increasing amount of neuroscientific knowledge draw educational resources away from other areas in psychiatry? Last, how do training directors view neuroscience as relevant to clinical practice for all psychiatric practitioners, both at present and in the future?
Method
Surveys were created and distributed to directors of all 182 psychiatric residency training programs in the U.S. and Canada. Hard copies of surveys were disseminated via U.S. mail; 1 month subsequent to this mailing, to improve response rate, an identical electronic version of the survey was sent to training directors via the American Association of Directors of Psychiatric Residency Training listserv. Training directors were given the option of returning the surveys electronically or via mail. Surveys were anonymous, although general characteristics of training programs were requested. Responses were coded upon receipt to ensure that only one response was received from each training program.
The survey consisted of 28 multiple-choice and free-response style questions (a copy of the survey used for this study accompanies the online version of this article). The instructions indicated that the purpose of the survey was to capture the current state, as well as recent and anticipated trends, of neuroscience education in psychiatric residency training programs. It was understood that neuroscience fundamentally underlies many aspects of psychiatry, but also that certain areas within the psychiatry curriculum are especially well framed in neuroscientific terms. Because of the importance of a uniform definition of “neuroscience,” we indicated that this term should encompass neuroanatomy, neurodevelopment, neuroimaging, cellular and molecular pathology, genetics, animal models, neuropsychiatry, and basic pharmacology (i.e., neurotransmitter systems, receptors, and neural circuitry). We further stipulated that clinical pharmacology teaching, unless directly related to these topics, should not be included in the definition of “neuroscience.”
Questions were grouped into three sections. The first section, “Description of your program,” addressed program size, hospital setting, availability of neuroscientists, and training directors’ years of experience. In the second section, “Neuroscience in your curriculum,” training directors were asked several questions about the quantity and composition of neuroscience teaching. This section addressed who provided neuroscience teaching, in what setting, and with what content emphasis. Further, training directors were asked to speculate how the content of the curriculum may change over time. We assessed which factors training directors considered important in shaping the neuroscience curriculum as well as the goals of teaching neuroscience to psychiatry residents. This section also contained a comparison to psychotherapy training within the curriculum and asked how many residents in the program completed research in biological psychiatry. The final section, “Neuroscience and clinical practice,” addressed the relevance of neuroscience education to practice patterns, both at present and in the future. In particular, training directors were asked how important neuroscience training will be for those residents who go on to become primarily psychotherapists or psychoanalysts.
Data from multiple-choice questions were analyzed by using SPSS for Windows (version 10.0). Descriptive statistics were used to characterize percent response. The Wilcoxon paired ranks test was used to assess differences in current versus future curriculum content. Linear regression with least squares analysis was used to determine which, if any, curriculum-shaping factors predicted the amount of neuroscience in the overall training curriculum.
Results
Description of Programs
Completed surveys were received from 77 of 182 training directors (42%), representing 1,856 of 4,629 residents (40%). We received 56 surveys by mail, followed by 21 electronically. Programs ranged in size from two to 80 residents, with a mean size of 24. A variety of program settings was represented: 32% of training directors identified their programs as affiliated with a private or tertiary care center, 18% with a city or public hospital, 8% with a community hospital, and 39% with other hospital milieus (e.g., VA hospitals or mixed settings). The remainder (3%) of training directors did not report their program setting.
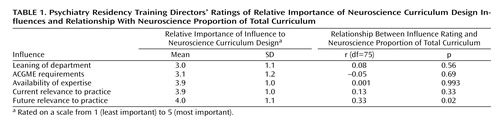
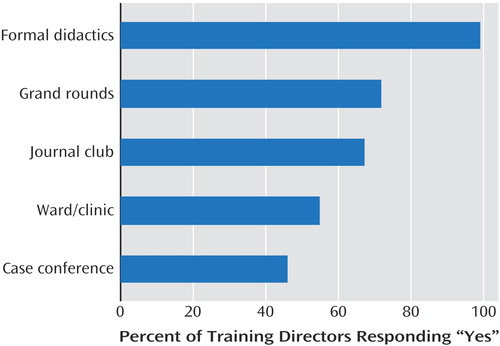
Exposure to neuroscience occurred throughout training in most programs, with 38% of training directors describing longitudinal integration (a single course running alongside other courses for an extended length of time) and 40% reporting both longitudinal and module-oriented curricula. Only 19% of programs relied exclusively on discrete modules (where a course stands alone and is temporally isolated from other courses). An interdisciplinary pattern emerged when training directors were asked to identify the background of their neuroscience educators. While psychiatrists constituted the mainstay of neuroscience education in most programs (92%), they were often joined by clinician scientists (68%) and neurologists (59%). However, when asked about the contexts in which neuroscientific teaching occurs, patient-related settings (case conferences, ward/clinic) were substantially underrepresented relative to didactics and other less clinical milieus ( Figure 1 ).
Despite the breadth of exposure to neuroscientific teaching, surprisingly few residents appear interested in conducting neuroscientific research. Most training directors reported that less than 10% of their residents engaged in biological psychiatry research either during or after residency ( Figure 2 ).

Neuroscience in the Curriculum
Training directors reported that neuroscience content constitutes, on average, 12% (SD=8.6) of their total residency-wide curricula. However, they felt that neuroscience content should ideally comprise 20% (SD=9.7) (t=10.37, df=76, p<0.001). The perceptions of current and anticipated trends in neuroscience content over time are illustrated in Figure 3 . In the past 5 years, the size of the neuroscience curriculum has increased in 70% of programs, with continued growth over the next 5 years anticipated by 86% of training directors.

An interesting comparison is that of analogous trends in psychotherapy education ( Figure 3 ), which strongly point to a perception of stability. Some 79% of training directors reported that their psychotherapy curriculum has remained the same size or increased in the past 5 years. While 73% anticipated the same amount of psychotherapy in the curriculum over the next 5 years, 18% believed that the psychotherapy content will increase.
We asked training directors to weigh the relative importance of five factors that influence curriculum design ( Table 1 ). Although availability of expertise and relevance to practice received somewhat higher ratings, no significant differences emerged. Logistic regression analysis indicated that only future relevance to practice significantly predicted the current amount of neuroscience in the curriculum.
We were also interested in comparing the perceived importance of specific areas within the neuroscience curriculum at present and 5 years from now ( Figure 4 ). While favoring clinical neurology/neuropsychiatry and basic pharmacology at present, training directors predicted significantly increased attention over time to each of the specific areas listed, with the most prominent growth being in neuroimaging and genetics.

*p<0.05. **p<0.005.
Relevance to Practice
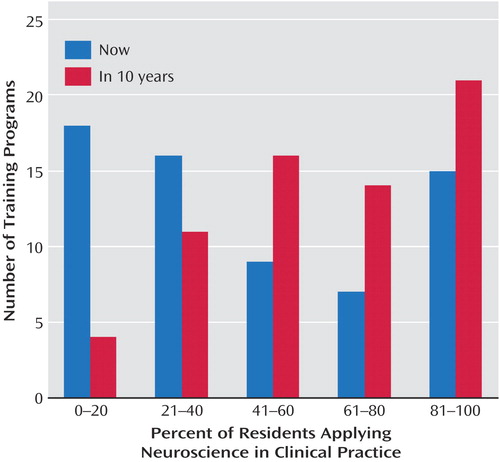
When asked what percentage of their residents would apply their neuroscientific training in their practice, training directors again predicted a changing pattern ( Figure 5 ). At present, there appears to be a bimodal distribution of programs, with peaks at both the low (0–20%) and high (81–100%) ends of the spectrum. However, when asked about the utility of neuroscientific teachings in practice 10 years from now, training directors responded in a more linear fashion, with greater numbers predicting that more of their residents will find neuroscience clinically useful. Moreover, 95% of training directors felt that neuroscience education will be relevant for residents who primarily will be psychotherapists or analysts.
Discussion
Our findings clearly illustrate the increasing prominence of neuroscience education in residency training programs, as well as training directors’ strong endorsement of neuroscience as meaningful to psychiatric practice. At the same time, the results raise some concerns about how well these two themes are connected in current curriculum designs. While neuroscience training may provide residents with important knowledge of theory and investigative tools, how this knowledge will be applied to practice remains an open question.
The great majority of training directors noted that psychiatrists were the primary instructors of neuroscience-related content. The relationship between psychiatry and neuroscience appears intimate enough that training directors need not import educators from other fields (e.g., neurology). However, when we looked at where neuroscience is taught, clinical settings appeared underrepresented. This may reflect the greater cost and labor-intensiveness of bringing neuroscientists to wards, clinics, and case conferences. Formal didactics, grand rounds, and journal clubs, which are logistically easier to arrange, are also intrinsically more variable in content. We are left to wonder how to better impart neuroscience theories to residents in clinical settings.
When we examined how the neuroscience curriculum is organized, most programs employed both longitudinal and modular approaches. This is consistent with the perceived importance of psychiatric neuroscience as a foundational subject matter that underlies theory and practice as well as a discrete subspecialty within psychiatry (17) . At the same time, perhaps this dichotomy underscores much of the confusion about how and where neuroscience should be taught. If training directors foresee increasing the amount of neuroscience taught to their residents, it remains unclear whether they mean to do this primarily within the didactic portion of the curriculum or within clinical settings.
If neuroscience-related content expands as projected, this would continue a trend that has persisted for at least 5 years. Training directors also reported increasing psychotherapy education over the past 5 years. This latter trend may be the result of new Accreditation Council for Graduate Medical Education (ACGME) Residency Review Committee competency requirements (18) , new studies detailing an evidence base for some psychotherapies (14 , 19) , or in response to backlash against a perceived lack of psychotherapy training in the recent past (20) . A significant majority of training directors also predicted that the amount of psychotherapy in their curricula will remain unchanged in the next 5 years. It is interesting, however, that nearly all respondents believed that neuroscience education is relevant even for those residents who will ultimately become primarily therapists or analysts. While at first blush this may seem quite counterintuitive, many recent editorials and articles cite the reciprocal progress that psychotherapy and neuroscience can offer each other (21 – 26) . Fields such as neuropsychoanalysis are rapidly emerging, as a great deal of raw material, theories, and techniques are available for study. Many respondents in our study cited Eric Kandel, who wrote that “Biological analysis is unlikely to diminish the interest in mentation or make mentation trivial by reduction; rather cell and molecular biology have merely expanded our vision, allowing us to perceive previously unanticipated interrelationships between biological and psychological phenomena” (24) . However, our results beg the question of whether neuroscience education is catching up with and surpassing a historically psychotherapy-driven curriculum or whether training directors are really focusing in on an integration of the two.
Of the factors that training directors cited as important in shaping the neuroscience curriculum, the only one that predicted total neuroscience content was a belief in the relevance of neuroscience to clinical practice in the future . It is significant that training directors did not appear to relate the amount of neuroscience content to their beliefs about its current relevance to clinical practice. It is also notable that availability of expertise in neuroscience seemed a nonissue. In contrast, a 1995 survey of neuropsychiatric training in psychiatry residency programs revealed that a major limitation to effective neuropsychiatric teaching was lack of adequate faculty (27) . However, that study described teaching in neuropsychiatry rather than neuroscience, again underscoring our point that framing material as obviously clinically relevant (neuropsychiatry) was more challenging than presenting the information in a relative clinical vacuum. Although we were concerned about the possible effects of fewer teaching resources in smaller institutions, we found no correlation between the size of the residency department and the amount of neuroscience taught (data not shown).
Departmental leanings did not appear to exert significant influence on neuroscience curricula, suggesting that clinical relevance and practice-based beliefs, rather than politics and other external requirements, have shaped neuroscience education. Likewise, ACGME requirements seemed to have little effect. However, it is also worth noting that ACGME requirements with respect to neuroscience training in psychiatry are somewhat vague, mentioning only “instruction in neurobiology, psychopharmacology, and other clinical sciences relevant to psychiatry” (28) . In contrast, ACGME requirements for the neuroscience curriculum in neurology training are far more specific, including “neuroanatomy, neuropathology, neurophysiology, neuroimaging, neuropsychology, neural development, neurochemistry, neuropharmacology, molecular biology, genetics, immunology, epidemiology, and statistics” (29) . Psychiatry training directors appear to recognize that neuroscience underlies clinical psychiatry to a similar extent as it does clinical neurology, which may account for their moving beyond ACGME requirements in their neuroscience curriculum planning.
Training directors believed that all eight of the surveyed neuroscientific elements will increase in their respective import in the next 5 years. However, some were thought to be more important than others, both at present and in the future. The largest increases were predicted to come from genetics, cellular and molecular pathology, and neuroimaging. Some authors believe that the extension of genetic approaches to clinical psychiatry and neurology actually holds greater promise for understanding etiology than any other neuroscientific modality (10 , 30) . These same authors state that genetics research that initially informs clinical work will lead to its transformation of clinical work. It is interesting that training directors predicted an increase in the importance of neuroimaging education that was nearly double that of neuroanatomy training. However, this does not flow logically, since the former relies on an intimate knowledge of the latter. Perhaps this is an attempt to maximize a perception of the clinical utility of neuroimaging. Again, this underscores the original impetus of our project, namely, searching for an obvious clinical utility in neuroscience education.
Most training directors felt that either very few, or very many, of their current residents will incorporate neuroscience into their practice after graduating from residency training. The reasons for this split pattern are unknown; however, it is notable that a single, right-skewed peak emerged when training directors were asked the same question regarding practice 10 years from now. These results again may reflect a disconnect—of note, not only on the part of residents—between the perceived current and future relevance of neuroscience.
Training directors reported that only a small minority of residents perform research in biological psychiatry. The number of residents performing nonbiological research is likely greater (31) , although we did not assess this issue. We were specifically interested in biologically oriented research because it may reflect, to some extent, the degree of influence of neuroscience-oriented faculty and because this pool of trainees will likely drive future translation of neuroscience to clinical psychiatry. A number of factors may underlie the small number of residents performing biological research (32 , 33) . Neuroscience research during residency is not always smiled upon by administrations, which in many cases prefer an emphasis on teaching and clinical service. There is often not enough time in the busy training schedule for residents to complete meaningful research projects. Moreover, training in research methodologies may be lacking and may depend more on training that one received in medical school. Of note, although the need for enhanced training resources is cited by the Institute of Medicine’s Report on Research Training in Psychiatry Residency (33) , the National Institute of Mental Health has not yet offered new funding initiatives for such training during residency.
Training directors felt that the neuroscience curriculum in most medical schools was insufficient preparation for the practice of psychiatry. This only serves to underscore the necessity of a well planned neuroscience curriculum for residency training. It also suggests that nonpsychiatrists and non-neurologists may be undereducated regarding the nervous system. This is troubling, given that so much of clinical medicine is tied to the brain. As other authors have suggested (32 , 34 , 35) , it is incumbent upon medical educators to ensure that physicians in other specialties learn more about brain function and dysfunction.
Our study has several important limitations. Foremost of these is the possibility of responder bias, since we received responses from slightly less than half of training directors. Recently published surveys of psychiatry residency training directors have reported highly variable response rates (27%–72%) despite using similar survey distribution methodologies (31 , 36–40) . The length of our survey, while broadening its scope, may also have dissuaded some training directors from responding. While we cannot claim with certainty that our data were also representative of training directors who chose not to respond, we did receive responses from a diverse range of program sizes and milieus. The average number of residents represented by training directors responding to our study (mean=24, SD=17) is similar to the national average of 27 (SD=14) among all psychiatry training programs (as reported by the ACGME and described by Greenberg and colleagues [41] ).
The distribution of residency program settings represented in this study is similar to those reported in other investigations of psychiatry education. Characterizing directors of medical student education in psychiatry, Balon and Riba (42) reported that 38% of programs received funding from university sources, 20% from state sources, and 42% from mixed or other sources. Similarly, drawing from National Mental Health Facilities Survey data (43) , Stroup and associates (44) reported that 35% of psychiatric residencies operated in academic medical centers. Although the milieu categories in our survey were not identical, the distribution in the present study was 32% private or tertiary, 18% city or public hospital, and 46% other or mixed.
Another possible source of responder bias relates to the variable neuroscience backgrounds of training directors, which we did not directly assess. However, given Balon and Riba’s finding that only 8% of psychiatry education directors belong primarily to a research or clinical research track (42) , and that presumably only a fraction of these conduct neuroscience research, it seems unlikely that the small number of training directors with a more formidable neuroscience background could have influenced the results of the present study.
With the use of a broad survey, this study was designed primarily for hypothesis-generating rather than hypothesis-testing. Moreover, some of our questions were more qualitative, making it hard to draw conclusions from these data. Our findings would benefit from replication, although they appeared to be internally consistent (especially with regard to current versus future relevance of neuroscience). Last, although conversations among residents from a multitude of U.S and Canadian programs formed the impetus for this study, it also would have been useful to issue a formal survey to current residents; this may have further highlighted that residents and training directors share similar concerns about the current relevance of neuroscience.
Despite these limitations, our survey firmly documents training directors’ belief in the importance of neuroscience training. Given the perceived future clinical utility of neuroscience, and the anticipated increase in curricular time devoted to it, educators will have to find space in an already crowded curriculum. How can this be achieved? A good first step would be to better integrate neuroscience education with clinical teaching. This may help residents appreciate the clinical relevance of neuroscience and may also allow them to explain disease processes to their patients in more vivid terms (45) . It would also force teachers and residents alike to think about the brain in a more integrated fashion. Unfortunately, many residents have been conditioned, whether through medical school or some other source, to think categorically and not integratively. This trend echoes mainstream psychiatry’s history of fluctuations between seemingly divergent positions. The challenge for educators, and for psychiatry as a whole, will be how to change this pattern of thinking. By introducing neuroscience selectively as the “glue” to integrate mind and brain, and by extension, psychotherapeutic and somatic treatments, residency programs will produce psychiatrists who are both fluent in the language of neuroscience and better prepared to apply it in clinical practice.
1. Kendler KS: Toward a philosophical structure for psychiatry. Am J Psychiatry 2005; 162:433–440Google Scholar
2. Wilson WP, Wells CE, Irigaray PJ: Should psychiatry and neurology integrate? Am J Psychiatry 1971; 128:617–622Google Scholar
3. Shorter E: A History of Psychiatry: From the Era of the Asylum to the Age of Prozac. New York, John Wiley & Sons 1997Google Scholar
4. Pardes H: Neuroscience and psychiatry: marriage or coexistence? Am J Psychiatry 1986; 143:1205–1212Google Scholar
5. Detre T: The future of psychiatry. Am J Psychiatry 1987; 144:621–625Google Scholar
6. Andreasen NC: Linking mind and brain in the study of mental illnesses: a project for a scientific psychopathology. Science 1997; 275:1586–1593Google Scholar
7. Davidson RJ, Irwin W: The functional neuroanatomy of emotion and affective style. Trends Cogn Sci 1999; 3:11–21Google Scholar
8. Lieberman JA: Dopamine partial agonists: a new class of antipsychotic. CNS Drugs 2004; 18:251–267Google Scholar
9. Swanson CJ, Bures M, Johnson MP, Linden AM, Monn JA, Schoepp DD: Metabotropic glutamate receptors as novel targets for anxiety and stress disorders. Nat Rev Drug Discov 2005; 4:131–144Google Scholar
10. Merikangas KR, Risch N: Will the genomics revolution revolutionize psychiatry? Am J Psychiatry 2003; 160:625–635Google Scholar
11. Gould TD, Manji HK: The molecular medicine revolution and psychiatry: bridging the gap between basic neuroscience research and clinical psychiatry. J Clin Psychiatry 2004; 65:598–604Google Scholar
12. Pulver SE: On the astonishing clinical irrelevance of neuroscience. J Am Psychoanal Assoc 2003; 53:755–772Google Scholar
13. Bradley R, Greene J, Russ E, Dutra L, Westen D: A multidimensional meta-analysis of psychotherapy for PTSD. Am J Psychiatry 2005; 162:214–227Google Scholar
14. Perry JC, Banon E, Ianni F: Effectiveness of psychotherapy for personality disorders. Am J Psychiatry 1999; 156:1312–1321Google Scholar
15. Mufson L, Dorta KP, Wickramaratne P, Nomura Y, Olfson M, Weissman MM: A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Arch Gen Psych 2004; 61:577–584Google Scholar
16. Beutel ME, Stern E, Silbersweig DA: The emerging dialogue between psychoanalysis and neuroscience: neuroimaging perspectives. J Am Psychoanal Assoc 2003; 51:773–801Google Scholar
17. Gordon E: Integrative neuroscience. Neuropsychopharmacology 2003; 28(suppl 1):S2–S8Google Scholar
18. Mellman LA, Beresin E: Psychotherapy competencies: development and implementation. Acad Psychiatry 2003; 27:149–153Google Scholar
19. Gabbard GO: Empirical evidence and psychotherapy: a growing scientific base. Am J Psychiatry 2001; 158:1–3Google Scholar
20. Clemens NA: Keeping the psyche in psychiatry. J Psychiatr Pract 2001; 7:53–54Google Scholar
21. Westen D, Gabbard GO: Developments in cognitive neuroscience, I: conflict, compromise, and connectionism. J Am Psychoanal Assoc 2002; 50:53–98Google Scholar
22. Solms M, Lechevalier B: Neurosciences and psychoanalysis. Int J Psychoanal 2002; 83(Pt 1):233–237Google Scholar
23. Wong PS: Anxiety, signal anxiety, and unconscious anticipation: neuroscientific evidence for an unconscious signal function in humans. J Am Psychoanal Assoc 1999; 47:817–841Google Scholar
24. Kandel ER: Biology and the future of psychoanalysis: a new intellectual framework for psychiatry revisited. Am J Psychiatry 1999; 156:505–524Google Scholar
25. Roffman JL, Marci CM, Glick DM, Dougherty DD, Rauch SL: Neuroimaging and the functional neuroanatomy of psychotherapy. Psychol Med 2005; 35:1385–1398Google Scholar
26. Pardes H: Lecture by Kandel E, “Cellular neurobiology, cognitive psychology, and the renaissance of a psychoanalytic perspective in the study of the brain” cited in neuroscience and psychiatry: marriage or coexistence? Am J Psychiatry 1986; 143:1205–1212Google Scholar
27. Duffy JD, Camlin H: Neuropsychiatric training in American psychiatric residency training programs. J Neuropsychiatry Clin Neurosci 1995; 7:290–294Google Scholar
28. Accreditation Council for Graduate Medical Education: Program requirements for residency training in psychiatry. (http://www.acgme.org/, accessed Sept 5, 2005)Google Scholar
29. Accreditation Council for Graduate Medical Education: Program requirements for residency education in neurology. (http://www.acgme.org/, accessed Sept 5, 2005)Google Scholar
30. Cowan WM, Harter DH, Kandel ER: The emergence of modern neuroscience: some implications for neurology and psychiatry. Ann Rev Neurosci 2000; 23:343–391Google Scholar
31. Fitzgerald MJ, Kablinger A, Manno B, Carter OS, Caldito G, Smith S: Psychiatry residents’ participation in research: a survey of attitudes and experience. Acad Psychiatry 2001; 25:42–47Google Scholar
32. Kupfer DJ, Hyman SE, Schatzberg AF, Pincus HA, Reynolds CF: Recruiting and retaining future generations of physician scientists in mental health. Arch Gen Psychiatry 2002; 59:657–660Google Scholar
33. Institute of Medicine: Research Training in Psychiatry Residency: Strategies for Reform. Washington, DC, The National Academies Press, 2003Google Scholar
34. Resnick DK, Ramirez LF: Neuroscience education of undergraduate medical students, part II: outcome improvement. J Neurosurg 2000; 92:642–645Google Scholar
35. Haines DE, Hutchins JB, Lynch JC: Medical neurobiology: do we teach neurobiology in a format that is relevant to the clinical setting? Anat Rec 2002; 269:99–106Google Scholar
36. King R, Koopman C, Millis D: Training on ethnic and gender issues in psychiatry residency training programs. Acad Psychiatry 1999; 23:20–29Google Scholar
37. Sudak DM, Beck JS, Gracely EJ: Readiness of psychiatry residency training programs to meet the ACGME requirements in cognitive-behavioral therapy. Acad Psychiatry 2002; 26:96–101Google Scholar
38. Ingels M, Marks D, Clark RF: A survey of medical toxicology training in psychiatry residency training programs. Acad Psychiatry 2003; 27:50–53Google Scholar
39. McQuistion HL, Ranz JM, Gillig PM: A survey of American psychiatric residency programs concerning education in homelessness. Acad Psychiatry 2004; 28:116–121Google Scholar
40. Varley CK, Jibson MD, McCarthy M, Benjamin S: A survey of the interactions between psychiatry residency programs and the pharmaceutical industry. Acad Psychiatry 2005; 29:40–46Google Scholar
41. Greenberg WM, Ritvo JL, Fazzio L, Bridgeford D, Fong T: A survey of addiction training programming in psychiatry residencies. Acad Psychiatry 2002; 26:105–109Google Scholar
42. Balon R, Riba M: Characteristics of directors of medical student education in psychiatry. Acad Psychiatry 1998; 22:162–169Google Scholar
43. Dorwart RA, Schlesinger M, Davidson H, Epstein S, Hoover C: A national study of psychiatric hospital care. Am J Psychiatry 1991; 148:204–210Google Scholar
44. Stroup TS, Dorwart RA, Hoover CW, Yeung E, Ostacher M: Clinical and community-service activities of psychiatric teaching hospitals. Acad Psychiatry 1999; 23:123–127Google Scholar
45. Green R, Clark A, Hickey W, Hutsler J, Gazzaniga M: Braincutting for psychiatrists: the time is ripe. J Neuropsychiatry Clin Neurosci 1999; 11:301–306Google Scholar