The Persistence of Mind-Brain Dualism in Psychiatric Reasoning About Clinical Scenarios
Abstract
Objective: Despite attempts in psychiatry to adopt an integrative biopsychosocial model, social scientists have observed that psychiatrists continue to operate according to a mind-brain dichotomy in ways that are often covert and unacknowledged and suggest that the same intuitive cognitive schemas that people use to make judgments of responsibility lead to dualistic reasoning among clinicians. The goal of this study was to confirm these observations. Method: Self-report questionnaires were sent to the 270 psychiatrists and psychologists in the Department of Psychiatry at McGill University. In response to clinical vignettes, the participants rated the level of intentionality, controllability, responsibility, and blame attributable to the patients, as well as the importance of neurobiological, psychological, and social factors in explaining the patients’ symptoms. Results: A total of 136 faculty members (50.4%) responded, and 127 were included in the analysis. Factor analysis revealed a single dimension of responsibility regarding the patients’ illnesses that correlated positively with ratings of psychological etiology and negatively with ratings of neurobiological etiology. Psychological and neurobiological ratings were inversely correlated. Multivariate analyses of variance supported these results. Conclusions: Mental health professionals continue to employ a mind-brain dichotomy when reasoning about clinical cases. The more a behavioral problem is seen as originating in “psychological” processes, the more a patient tends to be viewed as responsible and blameworthy for his or her symptoms; conversely, the more behaviors are attributed to neurobiological causes, the less likely patients are to be viewed as responsible and blameworthy.
Mind-brain dualism is the idea that the mind is somehow distinct from the brain and that its essence cannot be reduced to purely material and deterministic neurological mechanisms. This form of dualism has a long and venerable history in Western tradition (1) . Although many continue to support the view that mental phenomena result from emergent levels of organization of the brain (2 – 4) , the idea that mind and brain are different entities is no longer credible in medical science. Indeed, the last few decades have seen efforts to develop integrative models (4 – 12) heralded by claims that dualism in psychiatry has finally been overcome (4 , 6–10) .
Despite these efforts to adopt integrative approaches, ethnographic studies of psychiatric practice have found that psychiatrists continue to operate dualistically in ways that are often covert and unacknowledged (13 – 15) . The goal of the present study was to use a survey method to investigate the hypothesis that North American psychiatrists and psychologists reason dualistically about clinical problems.
The mind-brain dichotomy may persist among mental health professionals because it reflects a basic cognitive schema that is used intuitively to understand human behavior and, in particular, to make sense of troubling events. In these specific situations, people make “judgments of responsibility” (16 , 17) to determine whether a troubling event was caused by the actions of another person and, if so, whether that person acted intentionally. These attributions influence the subsequent emotional response to a troubling event; we experience anger and a desire for retribution toward individuals who intentionally caused the disturbing event and pity and compassion for victims who neither intended nor caused it (16 , 17) . This pattern of attribution and response is illustrated in Figure 1 .
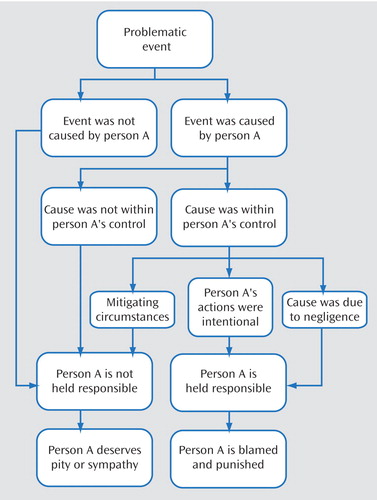
a Adapted with the permission of Guilford Press ©1995 from Weiner (16). Mitigating circumstances include such possibilities as person A being coerced, being incapable of appreciating the wrongfulness of his or her actions, or causing the problematic event to achieve a greater good (16, 17).
The tendency to make judgments in this way is thought to stem from an even more basic set of cognitive systems that guides human reasoning. Developmental psychologists have shown that as early as the first year of life infants demonstrate the ability to divide the world according to entities with and without agency and to use different intuitive rules to predict these perceptually different phenomena (18 – 20) . Infants use a “naive” or “intuitive physics” to predict the movements of inanimate objects that are propelled by external forces and an “intuitive psychology” to anticipate the behaviors of beings who act intentionally (21 – 27) . Over the course of human development, these cognitive systems become increasingly sophisticated, but it would seem that the basic dichotomy between intentional and unintentional events remains entrenched (28) and that it underlies the implicit reasoning involved in making judgments of responsibility (16) . Intentional events tend to be explained in psychological terms and to be associated with attributions of personal causality and responsibility, whereas unintentional events are seen as following physical laws and to be beyond the range of human responsibility (16 , 17) .
An illness is always a troubling event, and so it is not surprising that people tend to make judgments of responsibility when reasoning about its causes. Weiner demonstrated that lay adult subjects, when asked to rate various medical conditions, judged the symptoms of “mental-behavioral” illnesses, such as obesity and drug abuse, to be more intentional and viewed the sufferers of these conditions as more responsible and more blameworthy for their symptoms compared to those with “physical” conditions, such as cancer and heart disease (29) . In another study, it was found that lay respondents’ own ratings of the extent to which illnesses are behavioral were correlated with how much personal responsibility, blame, and social rejection they attributed to these conditions (30) . There is some evidence that the distinction between voluntary and involuntary forms of illness occurs across diverse cultures and leads people to blame and stigmatize those who are found responsible for their conditions (31) .
The goal of this study was to determine whether this same process of judgment making operates in the clinical reasoning of mental health professionals. The hypothesis was that when rating clinical vignettes, symptoms seen as being biologically determined would be associated with lower ratings of intentionality, controllability, responsibility, and blame; that symptoms rated as psychological would be correlated with high ratings on these dimensions; and that ratings of biological and psychological etiology would be inversely correlated.
Method
Participants
The study group was drawn from the 270 psychiatrists and psychologists on the faculty of the Department of Psychiatry at McGill University, which includes clinicians and researchers from a wide range of backgrounds representative of academic psychiatry in North America. Questionnaires were sent to faculty members, followed 1 month later by a second mailing. A description of the study, without explicit reference to the actual hypothesis, was included in a cover letter, and consent to participate was inferred by virtue of respondents completing and returning the questionnaire. A total of 136 faculty members responded, yielding a rate of response of 50.4%. Nine questionnaires were returned incomplete and thus were excluded, giving a final group size of 127 participants.
Of these 127 participants, 60.6% were men, and the average age was 52.7 years (SD=11.8); 70.9% were psychiatrists, and 29.1% were psychologists; 73.2% had training in pharmacotherapy, 96.1% in psychotherapy, 32.3% in psychoanalysis, and 61.4% in research. In terms of their practice, 70.1% provided pharmacotherapy, 87.4% psychotherapy, 15.7% psychoanalysis, 53.5% clinical research, and 7.1% basic science research. Information on the ages, genders, and professions (psychiatrists or psychologists) of all 270 potential subjects was obtained in an anonymous format from the Department of Psychiatry at McGill University so that a comparison of participants with nonresponders was possible. There were no significant differences in these basic demographic factors between these two groups.
Measures
A series of nine brief clinical vignettes was developed by crossing three common psychiatric conditions with three troubling behaviors to generate nine fictitious vignettes. The three conditions were 1) a manic episode induced by selective serotonin reuptake inhibitors, 2) narcissistic personality disorder, and 3) heroin dependence. It was anticipated that the manic episode would be viewed principally as a biologically determined process, the personality disorder would be seen as psychological in nature, and the heroin dependence would fall somewhere between those two extremes. Each of these conditions was then used to provide the context for three problematic behaviors: 1) a man spending all of his money to the point of bankruptcy, 2) a man knowingly engaging in high-risk sexual behavior leading him to contract HIV, and 3) a man stabbing his wife. To keep the vignettes consistent in all other respects, they were constructed according to a common plot with the character in each case a man in his 30s. The phrases used were kept as similar as possible across vignettes without compromising the flow and plausibility of the stories. For example, the “Personality Disorder Plus Bankruptcy” vignette reads as follows:
Dave is 37 years old. He prides himself on being extremely intelligent and important and finds it crucial to present himself as rich and successful and to associate with people of “high caliber.” However, he has never been able to maintain a job for very long because he always finds his employers to be “incompetent,” and he refuses to heed their suggestions. As a result, he does not earn much money and secretly he feels angry, empty, and degraded. Three months ago, he met Allan—the CEO of a large company—at a fitness club, and they became friends. Within a short while, Dave managed to go bankrupt by spending all his money on expensive dinners with Allan and on joining Allan’s golf club.
The respondents each received a set of three unlabeled vignettes, chosen and ordered randomly, except that each respondent saw only one of each condition and each behavior. After the respondents read each vignette, a uniform set of 10 questions tapped their attributions:
Did Dave intentionally go bankrupt?
Could Dave have stopped himself from going bankrupt?
Is Dave to be held responsible for going bankrupt?
Were the causes of Dave’s bankruptcy under his control?
How much monetary support or compensation does Dave deserve to help him out now?
How much is Dave to blame for going bankrupt?
Do you think Dave might learn from this experience to avoid similar events in the future?
How important are neurobiological factors in explaining why Dave went bankrupt?
How important are psychological factors in explaining why Dave went bankrupt?
How important are social factors in explaining why Dave went bankrupt?
Each question was rated on a 7-point Likert scale anchored at the extremes. Questions 1–6 assessed perceived intentionality, controllability, responsibility, and blame and were borrowed directly from the model by Weiner (16 , 17) . Question 7, measuring “competence,” was included based on suggestions in the literature (13 , 14) that patients who are seen as being responsible for their own symptoms might be further stigmatized as being somehow incompetent, unintelligent, or unable to learn from their errors. Questions 8–10 assessed causal attributions to biological, psychological, and social factors, respectively. At the end of the questionnaire, the respondents were asked to provide demographic information and to write what hypothesis they thought the questionnaire was trying to assess.
Data Analysis
To assess whether the order of appearance of the vignettes in the questionnaire packs had any effects on the responses, one-way repeated-measures analyses of variance (ANOVAs) were conducted for each of the 10 question items, irrespective of the vignette type, with the order of appearance of these items in the questionnaire as the single within-subject factor. Not one of these tests yielded a significant difference at the p<0.05 level. With a 5% test of significance, the power estimates ranged from 0.58 to 0.92, with six of these tests at values greater than p=0.80. Therefore, although for some of the questionnaire items the power was not adequate to reject the null hypothesis, any order effects appeared to be negligible.
The first step of the data analysis examined the dimensionality of judgments of responsibility (16) . Principal components analysis with varimax rotation was performed on the responses to the seven questionnaire items measuring intentionality, self-control, controllability, responsibility, compensation, blame, and competence. So as not to confound this procedure with repeated measures from respondents, three separate factor analyses were performed based on the order of appearance of the vignettes in the questionnaire packs. Before performance of the factor analyses, all variables were examined for skewness and corrected with square root transformations whenever the skewness statistic was greater than three times the standard error. In no instance did skewness statistic values exceed 1.0, and because the results of the factor analyses were virtually identical with or without the transformations, only the analyses of the raw data were used. For each of these three factor analyses, the main factor was then transformed into a single variable, referred to as the “responsibility” score, by averaging the scores of the individual items of this factor. Scale analysis was performed on these responsibility scores to compute Cronbach’s alpha values. Pearson’s correlations were then performed between the responsibility scores and the ratings of biological, psychological, and social etiology; again, these correlation analyses were performed in three separate tests based on the order of appearance of the vignettes in the questionnaire packs.
With data from all vignettes in one data set, multivariate repeated-measures ANOVAs were performed to test whether the three conditions (mania, narcissistic personality disorder, and heroin addiction) or the three behaviors (declaring bankruptcy, contracting HIV, stabbing a wife) that were described in the vignettes were associated with different mean values of the responsibility score and on the items measuring biological, psychological, and social etiology. Post hoc analyses were performed with least significant difference t tests with Bonferroni correction.
To determine whether any of the participants’ demographic factors influenced their responses, values of the responsibility scores and of the ratings of biological, psychological, and social etiology were averaged across the three vignettes for each subject, and these mean scores were used as the dependent variables for multivariate ANOVAs and analyses of covariance (ANCOVAs) with the various demographic variables as the independent variables. Because of the exploratory nature of these tests, each of the demographic variables was first tested individually and then combined into more complex models. A separate multivariate ANOVA was performed to test whether the participants’ awareness of the nature of the study’s hypothesis influenced their ratings of the responsibility scores and the scores of biological, psychological, and social etiology. Again, the respondents’ scores for these three dependent variables were averaged across their three vignettes, and the dependent variable was established by dichotomizing their written responses as to their guesses of the hypothesis into correct or incorrect categories.
Results
Responsibility
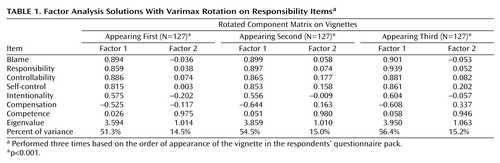
Factor analysis revealed that the items measuring intentionality, self-control, controllability, responsibility, compensation, and blame loaded highly onto one factor, explaining over 50% of the variance, with eigenvalues above 3.5, termed “responsibility,” whereas responses to the “competence” item were nearly completely orthogonal and constituted a second factor, with eigenvalues slightly above 1.00 ( Table 1 ). These results strongly support Weiner’s finding (16) that responsibility comprises a single dimension of causal reasoning. The fact that the item on competence was orthogonal to this factor further supports this conclusion because this item was not derived from Weiner’s model.
A Mind-Brain Dichotomy
The responsibility factors derived from these three analyses were then averaged into single variables, referred to here as the responsibility score. Scale analysis revealed Cronbach’s alpha values of 0.85 or above for the responsibility scales derived from this factor. Pearson’s correlations ( Table 2 ) indicated that responsibility scores correlated in a positive direction with ratings of psychological etiology (r=0.44, 0.56, and 0.57) and in an inverse direction with ratings of biological etiology (r=–0.53, –0.56, and –0.60) and that ratings of psychological etiology were also inversely correlated with biological etiology (r=–0.35, –0.46, and –0.50). Ratings of psychological etiology were correlated with scores of social etiology (r=0.34, 0.40, and 0.50), and social etiology was also correlated, albeit modestly, with ratings of responsibility (r=0.14, 0.27, and 0.31).
Multivariate repeated-measures ANOVA performed with the vignette condition (mania, narcissistic personality disorder, and heroin addiction) as the independent factor was significant at the p<0.001 level with Pillai’s trace, and highly significant differences were found among the three conditions for the mean scores of responsibility (F=147.7, df=2, 224, p<0.001), biological etiology (F=211.2, df=2, 224, p<0.001), psychological etiology (F=89.5, df=2, 224, p<0.001), and social etiology (F=32.3, df=2, 224, p<0.001). Post hoc least significant difference tests with Bonferroni correction revealed highly significant pairwise differences among all three vignette conditions for responsibility score, psychological etiology, and biological etiology ( Figure 2 ). Post hoc tests on the social etiology responses failed to show any significant difference between the addiction (mean=4.62, 95% confidence interval [CI]=4.40–4.84) and personality disorder (mean=4.42, 95% CI=4.26–4.67) conditions, although these did differ significantly (p<0.001) from the mania condition (mean=3.40, 95% CI=3.13–3.68).

a Post hoc least significant difference tests with Bonferroni correction.
Although the multivariate repeated-measures ANOVA for the vignette behaviors (declaring bankruptcy, contracting HIV, stabbing a wife) was also significant (Pillai’s trace p<0.001), only the responsibility score yielded a significant effect (F=4.9, df=2, 224, p<0.01), and a post hoc test revealed that the only significant difference (p<0.05) was between the means for the HIV (mean=3.92, 95% CI=3.62–4.23) and the wife-stabbing (mean=4.55, 95% CI=4.30–4.80) behaviors.
Confounders
When multivariate analyses were performed for each of the demographic variables separately (see Participants section) on the respondents’ mean ratings of biological, psychological, and social etiologies and the responsibility score, only gender was found to be significant (Pillai’s trace p<0.01) and only with respect to differences in the responsibility score (F=7.15, df=1, 111, p<0.01); the female respondents tended to give slightly lower responsibility scores overall (mean=3.96, 95% CI=3.76–4.16) than the male respondents (mean=4.31, 95% CI=4.15–4.47). However, when gender was combined with the other demographic variables into larger multivariate analyses, these differences no longer remained significant.
Regarding the respondents’ guesses of the study’s hypothesis, 36.2% (N=46) correctly guessed the hypothesis. Nevertheless, multivariate ANOVAs found no significant differences in the respondents’ ratings of biological, psychological, and social etiologies and responsibility score based on whether their guesses were correct or incorrect (Pillai’s trace p=0.85).
Discussion
The results of this study support the hypothesis that mental health professionals tend to use a mind-brain dichotomy in their reasoning about clinical vignettes and suggest that this dualistic thinking reflects, at least in part, the implicit judgments of responsibility that they make regarding patients’ symptoms. The clinicians in our study associated the psychological causation of mental illness with attributions of intentionality, controllability, responsibility, and blameworthiness on the part of the patient, and they tended to view behaviors with a biological etiology as unintentional, uncontrollable, not within the patient’s sphere of personal responsibility, and less blameworthy. As predicted by our hypothesis, these ratings were related to the underlying conditions of the vignettes, with behaviors of different types rated as mainly biological if they occurred in the context of mania, as psychological if they occurred in the context of a narcissistic personality disorder, and as midway between these poles if they appeared to be due to heroin addiction.
The fact that these clinicians attributed high degrees of responsibility for pathological behaviors resulting from a personality disorder when it is well known that such behaviors are, in fact, difficult to change through conscious effort reveals the respondents’ intuitive bias. Furthermore, given that the findings of this study closely resemble the kind of reasoning found among lay populations (16 , 29 , 30) and that they were not affected by the respondents’ level or type of professional training and background or even by the respondents’ explicit awareness of the study’s hypothesis suggests that the results reflect persistent patterns of dualistic thinking. However, these findings do not necessarily cover the whole domain of mind-brain dualism in psychiatry because other factors besides judgments of responsibility may also contribute to dualistic thinking (14) .
For the vignettes dealing with heroin addiction, ratings of biological and psychological etiology were roughly equivalent and midrange. The design of this study did not allow us to assess whether the participants held an integrated view of the neurobiological and psychological aspects of heroin addiction or whether they ambivalently vacillated between two opposing notions in tandem. However, the continuing debates in the literature about whether substance addictions are more biological or psychological (32) , combined with the fact that the ratings for the addiction vignettes followed precisely the predictions of the hypothesis and that neither psychological nor biological etiologies rated highly for this condition, favor the view that the respondents vacillated between the two opposing poles.
In all of our analyses, social etiology showed patterns of association similar to those found for psychological etiology, although in every instance, its associations were more modest statistically and more of its variance was attributable to unmeasured factors and error. It may be that some respondents viewed social etiology as part of a broader “psychosocial” factor, whereas others gave a different meaning to this concept or simply viewed social etiology as irrelevant to the clinical vignettes.
This study did not address the empirical issue of the actual intentionality or controllability of psychiatric symptoms or disorders. Given that there is little empirical research measuring the extent of intentionality of various psychiatric conditions, we must consider that, like lay persons, the participants in this study reasoned about the clinical vignettes using an intuitive logic. In general, there may be nothing problematic about attributing greater responsibility for actions that are more volitional. Indeed, some have argued that these sorts of causal appraisals may reflect evolutionary adaptations in cognition that help us to predict more accurately our social environments (33 , 34) . What remains questionable is the basis upon which the clinicians in our study viewed one psychiatric disorder as more controllable than another and whether further advances in the scientific understanding of behavioral disorders could ever fully supplant clinicians’ tendency to employ dualistic reasoning.
Instead of assuming that medicine and psychiatry have transcended dualism, it may prove more useful for clinicians to acknowledge its continuing influence on their thinking and to consider carefully the potential implications of this kind of reasoning. For example, in some instances, clinicians may want to relieve patients’ and families’ feelings of guilt and shame regarding mental illness by stressing the biological dimensions of the condition, whereas in other cases, the goal might be to foster a sense of control in the patient’s approach to his or her symptoms and thus stress a more psychological model. In every case, the meanings of these attributions draw from basic cognitive distinctions as well as subsequent cultural elaboration. Cultural meanings may change the implications of basic attributions so that biological disorders, for example, are viewed as intrinsic to the person and hence highly stigmatized (35) . Future research should examine the interaction of these basic distinctions with broader cultural notions of the cause and nature of psychiatric symptoms and disorders (36) .
1. Priest S: Theories of the Mind. London, Penguin Books, 1991Google Scholar
2. Kauffman S: At Home in the Universe: The Search for the Laws of Self-Organization and Complexity. New York, Oxford University Press, 1993Google Scholar
3. Henningsen P, Kirmayer LJ: Mind beyond the net: implications of cognitive neuroscience for cultural psychiatry. Transcult Psychiatry 2000; 37:467–494Google Scholar
4. Kendler KS: Toward a philosophical structure for psychiatry. Am J Psychiatry 2005; 162:433–440Google Scholar
5. Engel GL: The need for a new medical model: a challenge for biomedicine. Science 1977; 196:129–135Google Scholar
6. Andreasen NC: Linking mind and brain in the study of mental illness: a project for a scientific psychopathology. Science 1997; 275:1586–1593Google Scholar
7. Damasio AR, Harrington A, Kagan J, McEwen BS, Moss H, Shaikh R (eds): Unity of knowledge: the convergence of natural and human science, in the Annals of the New York Academy of Sciences, vol 935. New York, New York Academy of Sciences, 2001, pp 39–41Google Scholar
8. Kandel ER: A new intellectual framework for psychiatry. Am J Psychiatry 1998; 155:457–469Google Scholar
9. Maunder R: Implications of mind-body theory for integration into psychiatry. Psychiatry 1995; 58:85–97Google Scholar
10. Gabbard GO: Mind, brain, and personality disorders. Am J Psychiatry 2005; 162:648–655Google Scholar
11. Bennett MR, Hacker PMS: Philosophical Foundations of Neuroscience. Malden, Mass, Blackwell Scientific, 2003Google Scholar
12. Bolton D, Hill J: Mind, Meaning and Mental Disorder: The Nature of Causal Explanation in Psychology and Psychiatry. Oxford, UK, Oxford University Press, 1996Google Scholar
13. Luhrmann TM: Of Two Minds: The Growing Disorder in American Psychiatry. New York, Alfred A Knopf, 2000Google Scholar
14. Kirmayer LJ: Mind and body as metaphors: hidden values in biomedicine, in Biomedicine Examined (Culture, Illness, and Healing). Edited by Lock M, Gordon D. Boston, Kluwer Academic Press, 1988Google Scholar
15. Kirmayer LJ: Improvisation and authority in illness meaning. Cult Med Psychiatry 1994; 18:183–214Google Scholar
16. Weiner B: Judgments of Responsibility: A Foundation for a Theory of Social Conduct. New York, Guilford, 1995Google Scholar
17. Weiner B: Responsibility for social transgressions: an attributional analysis, in Intentions and Intentionality: Foundations of Social Cognition. Edited by Malle BF, Moses LJ, Baldwin DA. Cambridge, Mass, MIT Press, 2001, pp 331–344Google Scholar
18. Blakemore SJ, Decety J: From the perception of action to the understanding of intention. Nat Rev Neurosci 2001; 2:561–567Google Scholar
19. Woodward AL: Infants’ ability to distinguish between purposeful and non-purposeful behaviours. Infant Behav Dev 1999; 22:145–160Google Scholar
20. Premack D, Premack AJ: Intention as psychological cause, in Causal Cognition: A Multidisciplinary Debate. Edited by Premack D, Premack AJ. Oxford, UK, Clarendon Press, 1995, pp 185–199Google Scholar
21. Premack D: The infant’s theory of self-propelled objects. Cognition 1990; 36:1–16Google Scholar
22. Legerstee M: The role of person and object in eliciting early imitation. J Exp Child Psychol 1991; 51:423–433Google Scholar
23. Legerstee M: A review of the animate-inanimate distinction in infancy: implications for models of social and cognitive knowing. Early Dev Parenting 1992; 3:71–80Google Scholar
24. Spelke ES, Phillips A, Woodward AL: Infants’ knowledge of object motion and human action, in Causal Cognition: A Multidisciplinary Debate. Edited by Premack D, Premack AJ. Oxford, UK, Clarendon Press, 1995, pp 44–77Google Scholar
25. Woodward AL, Sommerville JA, Guajardo JJ: How infants make sense of intentional action, in Intentions and Intentionality: Foundations of Social Cognition. Edited by Malle BF, Moses LJ, Baldwin DA. Cambridge, Mass, MIT Press, 2001, pp 149–170Google Scholar
26. Povinelli DJ: On the possibilities of detecting intentions prior to understanding them, in Ibid., pp 225–250Google Scholar
27. Wellman HM, Phillips AT: Developing intentional understandings, in Ibid., pp 125–148Google Scholar
28. Malle BF: How people explain behavior: a new theoretical framework. Pers Soc Psychol Rev 1999; 3:23–48Google Scholar
29. Weiner B, Perry RP, Magnusson J: An attributional analysis of reactions to stigmas. J Pers Soc Psychol 1988; 55:738–748Google Scholar
30. Crandall CS, Moriarty D: Physical illness stigma and social rejection. Br J Soc Psychol 1995; 34(part 1):67–83Google Scholar
31. Shweder RA, Much NC, Mahapatra M, Park L: The “big three” of morality (autonomy, community, divinity) and the “big three” explanations of suffering, in Morality and Health. Edited by Brandt A, Rozin P. New York, Routledge, 1997, pp 119–172Google Scholar
32. Kalivas PW: Choose to study choice in addiction. Am J Psychiatry 2004; 161:193–194Google Scholar
33. Malle BF, Moses LJ, Baldwin DA (eds): Intentions and Intentionality: Foundations of Social Cognition. Cambridge, Mass, MIT Press, 2001Google Scholar
34. Mithen S: Paleoanthropological perspectives on the theory of mind, in Understanding Other Minds: Perspectives From Developmental Cognitive Neuroscience. Edited by Baron-Cohen S, Tager-Flusberg H, Cohen J. Oxford, UK, Oxford University Press, 2000, pp 488–502Google Scholar
35. Angermeyer MC, Matschinger H: Causal beliefs and attitudes to people with schizophrenia: trend analysis based on data from two population surveys in Germany. Br J Psychiatry 2005; 186:331–334Google Scholar
36. Kirmayer LJ, Young A: Culture and context in the evolutionary concept of mental disorder. J Abnorm Psychol 1999; 108:446–452Google Scholar