Effectiveness of Olanzapine, Quetiapine, Risperidone, and Ziprasidone in Patients With Chronic Schizophrenia Following Discontinuation of a Previous Atypical Antipsychotic
Abstract
Background: In the treatment of schizophrenia, changing antipsychotics is common when one treatment is suboptimally effective, but the relative effectiveness of drugs used in this strategy is unknown. This randomized, double-blind study compared olanzapine, quetiapine, risperidone, and ziprasidone in patients who had just discontinued a different atypical antipsychotic. Method: Subjects with schizophrenia (N=444) who had discontinued the atypical antipsychotic randomly assigned during phase 1 of the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) investigation were randomly reassigned to double-blind treatment with a different antipsychotic (olanzapine, 7.5–30 mg/day [N=66]; quetiapine, 200–800 mg/day [N=63]; risperidone, 1.5–6.0 mg/day [N=69]; or ziprasidone, 40–160 mg/day [N=135]). The primary aim was to determine if there were differences between these four treatments in effectiveness measured by time until discontinuation for any reason. Results: The time to treatment discontinuation was longer for patients treated with risperidone (median: 7.0 months) and olanzapine (6.3 months) than with quetiapine (4.0 months) and ziprasidone (2.8 months). Among patients who discontinued their previous antipsychotic because of inefficacy (N=184), olanzapine was more effective than quetiapine and ziprasidone, and risperidone was more effective than quetiapine. There were no significant differences between antipsychotics among those who discontinued their previous treatment because of intolerability (N=168). Conclusions: Among this group of patients with chronic schizophrenia who had just discontinued treatment with an atypical antipsychotic, risperidone and olanzapine were more effective than quetiapine and ziprasidone as reflected by longer time until discontinuation for any reason.
Antipsychotic drugs are the cornerstone of treatment for schizophrenia but have limited effectiveness (1) . A common treatment strategy when a drug is not adequately efficacious or tolerable is to switch medicines in an attempt to obtain greater effectiveness, but it is not known if any second-generation antipsychotic drugs other than clozapine have advantages over others when used in this situation.
For patients with symptoms that fail to respond adequately to antipsychotic treatment, only clozapine has consistently been shown to be more effective than other drugs (2 – 4) . However, clozapine is not commonly used because of the risk of severe side effects, including agranulocytosis, and because of its substantial level of intolerability and complexity of administration. Instead, other second-generation antipsychotics are commonly recommended when one drug is not effective, but clinicians and patients have little to guide them in this situation. On the basis of the assumption that other antipsychotics are similarly efficacious, practice guidelines have suggested that treatment choice should be made according to patient preference and side effect risks (5) .
However, a growing body of evidence suggests that second-generation drugs are not homogeneous in their effects and may have substantial differences in efficacy, including relapse prevention, and in the incidence of side effects (1 , 6–8) . In addition, adverse metabolic effects, including an increased risk of diabetes, dyslipidemias, and coronary heart disease, have been associated with second-generation antipsychotics (9 , 10) .
We report the primary outcomes of a double-blind clinical trial that compared the effectiveness of atypical antipsychotics among schizophrenia patients who had just discontinued treatment with a different atypical antipsychotic randomly assigned during phase 1 of the long-term Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) investigation. This phase 2 study was recommended to individuals who poorly tolerated their previous treatment, but it also included 1) patients who discontinued their previous treatment because of inefficacy and did not want to consider treatment with clozapine, and 2) patients who discontinued their previous treatment independently of their doctor’s recommendation.
Method
Study Setting and Design
The CATIE investigation was initiated by the National Institute of Mental Health (NIMH) to determine the comparative effectiveness of antipsychotic drugs. Its rationale, design, and methods have been previously described in detail (1 , 11–14) . The study was conducted between January 2001 and December 2004 at 57 U.S. clinical sites. In phase 1, patients were randomly assigned to receive olanzapine, perphenazine, quetiapine, risperidone, or ziprasidone under double-blind conditions and were followed for up to 18 months or until treatment was discontinued for any reason. Patients whose assigned phase 1 treatment was discontinued could enter phase 2 (12) . If the treatment received during phase 1 was perphenazine, patients entered phase 1B in which they were randomly assigned to receive double-blind treatment with olanzapine, quetiapine, or risperidone. If patients again discontinued treatment in phase 1B, they then entered phase 2.
In phase 2, patients and their study doctor could choose between two randomization pathways. The “efficacy” pathway (phase 2E), recommended to individuals who discontinued the previous treatment because of inefficacy, compared open-label clozapine to double-blind treatment with olanzapine, quetiapine, or risperidone. The “tolerability” pathway (phase 2T), recommended to individuals who discontinued the previous treatment because of intolerability, compared double-blind treatment with olanzapine, quetiapine, risperidone, or ziprasidone. The choice between pathways was meant to simulate everyday practice in which many patients do not accept the recommendation to try clozapine.
The present report is limited to results from the phase 2 tolerability pathway. Patients were assigned to a treatment they had not received in phase 1. Patients eligible to receive ziprasidone were randomly assigned to ziprasidone or one of the other atypical antipsychotics not previously received in a 2:1:1 ratio. Those who enrolled in phase 2 before the availability of ziprasidone were assigned to a drug not previously received in a 1:1 ratio. Patients who received ziprasidone during phase 1 were randomly assigned to olanzapine, quetiapine, or risperidone treatment in a 1:1:1 ratio. If the assigned treatment worked adequately, patients could continue receiving it until the completion of either 18 months of study treatment across phases 1 and 2 or until 6 months of treatment in phase 2 (if the 6-month period extended beyond the original 18 months).
Participants
Initial inclusion criteria required age between 18 and 65 years, a diagnosis of schizophrenia (determined by the Structured Clinical Interview for DSM-IV), and appropriateness for oral antipsychotic medication. Exclusion criteria were diagnosis of schizoaffective disorder, mental retardation, or other cognitive disorders; past serious adverse reactions to any of the proposed treatments; the current episode of schizophrenia being the patient’s first; history of treatment resistance, defined by persistence of severe symptoms despite adequate trials of one of the proposed treatments or prior treatment with clozapine for treatment resistance; current pregnancy or breast-feeding; or serious and unstable medical condition.
The study was approved by an institutional review board at each site, and written informed consent was obtained from each patient or their legal guardian.
Interventions
Identical capsules contained olanzapine, 7.5 mg; quetiapine, 200 mg; risperidone, 1.5 mg; or ziprasidone, 40 mg. (Ziprasidone was approved for use by the Food and Drug Administration after the study began and was added to the study in January 2002.) Medications were flexibly dosed (within one to four capsules daily) on the basis of the study doctor’s judgment. Overlap in the administration of the phase 1 and phase 2 antipsychotics was permitted for the first 4 weeks to allow for gradual transition to the new medication. Concomitant medications were permitted throughout the trial except additional antipsychotics. Patients had monthly visits with study doctors.
The drug package inserts for quetiapine and ziprasidone specify that these drugs are to be given twice daily, whereas olanzapine and risperidone may be given once daily. To protect blinding, half the patients assigned to olanzapine and risperidone were assigned to twice daily dosing and the other half to once daily dosing. To minimize initial side effects, patients assigned to quetiapine began treatment by receiving one 100-mg capsule on days 1 and 2, one twice daily on day 3, and one for the first dose of day 4. All patients assigned to twice-a-day dosing received five identical capsules to begin treatment.
Objectives and Outcomes
We hypothesized that there would be significant differences in the overall effectiveness of olanzapine, quetiapine, risperidone, and ziprasidone in treating schizophrenia. Because we expected many discontinuations in phase 1 to be due to weight gain, and because ziprasidone was expected to cause little or no weight gain, we also hypothesized that ziprasidone would be more effective than the other drugs.
The primary outcome measure was time until treatment discontinuation for any reason, a discrete outcome selected because stopping or changing medication is a frequent occurrence and major problem in the treatment of schizophrenia. Medication discontinuation integrates patient and clinician judgments of efficacy, safety, and tolerability into a global measure of effectiveness and signals the need for a new treatment strategy. A key secondary outcome was the reason for treatment discontinuation as judged by the study doctor. Additional secondary efficacy outcomes included Positive and Negative Syndrome Scale (PANSS) scores and Clinical Global Impression (CGI) ratings, which were collected during the study visits at baseline and months 1, 3, 6, 9, 12, 15, and 18. Secondary safety and tolerability outcomes included incidence of serious adverse events, incidence of treatment-emergent adverse events, and changes in weight, neurologic side effects, and laboratory analytes.
Statistical Methods
Ziprasidone was added to the trial after 24% of phase 2 enrollment. Because the main aim of phase 2 was the evaluation of ziprasidone, all effectiveness evaluations were limited to the cohort of patients who received at least one dose of study medication and entered the phase after ziprasidone became available. (A series of confirmatory analyses including all phase 2 patients were consistent with the planned analyses.) In order to best characterize side effect profiles, safety outcomes are reported for all patients assigned to a treatment condition.
Time until phase 2 treatment discontinuation was estimated by Kaplan-Meier survival curves. Treatment groups were compared with Cox proportional hazards regression models (15) that adjusted for 1) whether the patient had an exacerbation in the 3 months before entering the study, 2) tardive dyskinesia status at study baseline, and 3) whether the patient was initially assigned to perphenazine (and thus had an additional treatment phase prior to entering phase 2). The overall difference between treatments was evaluated with the use of a test with three degrees of freedom (df). If significance was reached at a level of p≤0.05, ziprasidone was then compared with each of the other antipsychotics by a Hochberg adjustment for multiple comparisons (16) , in which the largest p value was compared with a value of 0.05 and the smallest p value was compared with a value of 0.017 (0.05/3). In addition, the three atypical groups were compared with each other via step-down testing: pairwise comparisons were evaluated only if the p value from the 2 df test was ≤0.05. Subgroup analyses were planned in order to compare treatments separately for those who had previously discontinued due to lack of efficacy and intolerability.
A sensitivity analysis of the Cox model for treatment discontinuation evaluated the effects of potentially important baseline covariates and their interaction with treatment group. Covariates evaluated included demographic and baseline characteristics as well as treatment received in phase 1 and reasons for discontinuation from phase 1.
Treatment groups were compared in terms of PANSS scores and CGI severity ratings over time with a mixed model that adjusted for the same fixed covariates as for time until discontinuation, plus baseline value, time, and baseline-by-time interactions. Treatment-by-time interactions were not significant, so treatment groups were compared across the average of all timepoints. Time was classified into quarterly intervals, represented by months 3, 6, 9, and 12. End-of-phase assessments were assigned to the next interval. Months 15 and 18 were excluded from analyses because of small sample sizes. The correlation of the repeated measures was modeled via a random subject intercept and an unstructured covariance matrix.
Treatment groups were compared for baseline characteristics on the basis of analysis of variance (ANOVA) or chi-square tests with 3 df. Overall treatment comparisons for safety outcomes are presented for descriptive purposes. The p values were based on Poisson regression or an analysis of covariance (ANCOVA), both of which adjusted for differential duration of phase 2 study drug in addition to the covariates used in the primary analysis. Fisher’s exact test was used in cases of small group sizes. For laboratory parameters, exposure-adjusted ANCOVA least squares means are presented, but because of skewed distributions, p values are from a rank ANCOVA.
The study was funded by NIMH. The pharmaceutical companies whose drugs were included donated the drugs and provided input on the dosage range only for their own drug; they had no other input in study design, analyses, or interpretation of results. The manuscript was written solely by the listed authors.
Results
Patient Characteristics and Disposition
Figure 1 depicts the enrollment, allocation, and follow-up of study patients; 1,493 patients were enrolled in the study and randomly assigned to a phase 1 treatment. Of the 1,052 patients who were eligible for phase 2, 99 patients (9%) entered the efficacy pathway (phase 2E), 444 patients (42%) entered the tolerability pathway (phase 2T) described in this article, and 509 patients (48%) did not enter phase 2.
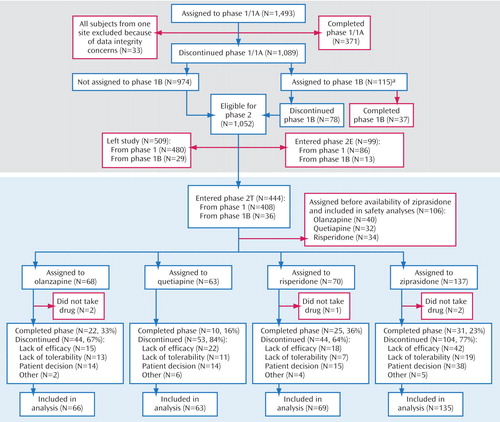
a Phase 1B: double-blind treatment with olanzapine, quetiapine, or risperidone for those patients first assigned to perphenazine.
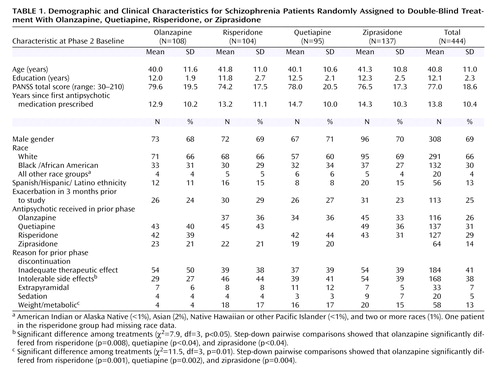
The demographic and clinical characteristics of the sample at the beginning of phase 2 are shown in Table 1 . The characteristics of patients in each of the groups were similar with the following exception: because the phase 1 discontinuation reasons and rates differed among the treatments, and the study design did not allow individuals to be reassigned to the drug they received in phase 1, the reasons for phase 1 discontinuation were variably represented across treatments in phase 2. Patients who were assigned to olanzapine during phase 2 had the lowest rates of phase 1 discontinuation because of intolerable side effects and the lowest rates of discontinuation due to weight gain or metabolic side effects.
The demographic and clinical characteristics of patients who entered phase 2 were generally representative of the original phase 1 sample, except that a low proportion of patients who discontinued the previous phase because of “patient decision” continued to phase 2T (18%, N=81 of 448). In contrast, higher proportions of patients who discontinued the previous phase because of inefficacy or intolerability entered phase 2T (intolerability: 87% [N=168 of 193]; inefficacy: 58% [N=184 of 318]).
There were no substantial differences in concomitant medications added during the phase between the study drugs.
Treatment Discontinuation
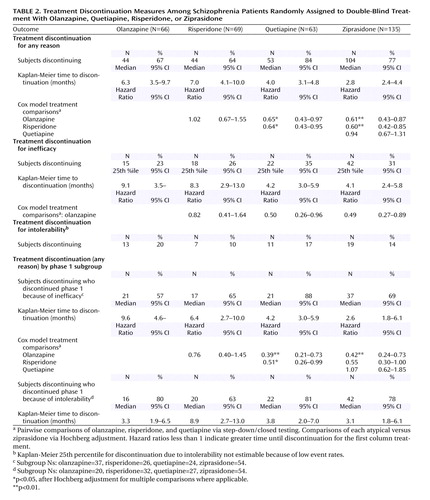
In phase 2, 74% of the 333 patients in the intent-to-treat cohort (i.e., excluding the 106 patients assigned before the availability of ziprasidone) discontinued treatment before completion of the study. Median treatment duration was 4 months.
Discontinuation outcomes are presented in Table 2 and Figure 2 . There was an overall treatment group difference in time until discontinuation for any reason (p=0.004). The time was longer for olanzapine and risperidone (median 6.3 and 7.0 months, respectively) relative to quetiapine and ziprasidone (4.0 and 2.8 months). Pairwise comparisons showed significant differences between olanzapine and quetiapine, olanzapine and ziprasidone, risperidone and quetiapine, and risperidone and ziprasidone.
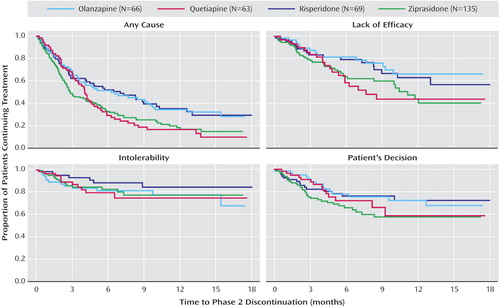
There was an overall treatment group difference in time until discontinuation because of lack of efficacy (p<0.05), but no comparisons were statistically significant after adjustment for multiple comparisons. There were no overall treatment group differences for time until discontinuation because of intolerable side effects.
Discontinuation by reason for phase 1 discontinuation
Discontinuation rates for the patients who discontinued their previous treatment because of intolerability or lack of efficacy are presented in Table 2 and Figure 3 . There was an overall treatment group difference among the 184 patients who discontinued their previous treatment because of inefficacy (p=0.004). The olanzapine group had a significantly longer median time until treatment discontinuation for any reason compared with quetiapine and ziprasidone but not risperidone. Risperidone had a significantly longer time until treatment discontinuation for any reason compared with quetiapine but not ziprasidone. Quetiapine did not significantly differ from ziprasidone.
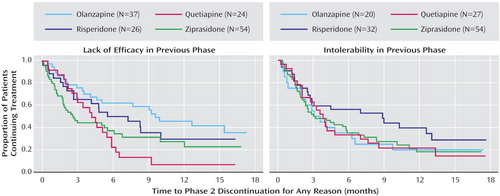
Among the 168 patients who discontinued their previous treatment because of intolerability, the median time until phase 2 treatment discontinuation was longest for risperidone relative to olanzapine, quetiapine, and ziprasidone, but the differences among groups were not significant.
Adjustment for covariates and interactions
An exploratory analysis of time until phase 2 treatment discontinuation for any reason found that patients who discontinued their previous treatment because of weight gain or metabolic effects stayed in phase 2 longer than other patients (hazard ratio=0.59, 95% CI=0.40–0.85 [p=0.005]). Results of the primary treatment comparisons were unchanged after adjusting for this covariate, both overall and for the subgroup of patients who previously discontinued for intolerability. Exploratory analyses also identified a significant interaction between olanzapine and whether the patient had discontinued the previous phase for lack of efficacy. As reported in the subgroup analyses, patients receiving olanzapine stayed in phase 2 longer if they had discontinued phase 1 due to lack of efficacy versus other reasons (hazard ratio=0.44, 95% CI=0.24–0.81 [p=0.008]).
Efficacy Measures
Figure 4 shows the mixed model estimated mean change in PANSS scores over time by treatment group. The olanzapine group improved more than the quetiapine (estimated mean difference=–6.8, SE=2.4 [p=0.005]) and ziprasidone (difference=–5.9, SE=2.1 [p=0.005]) groups but not the risperidone group.
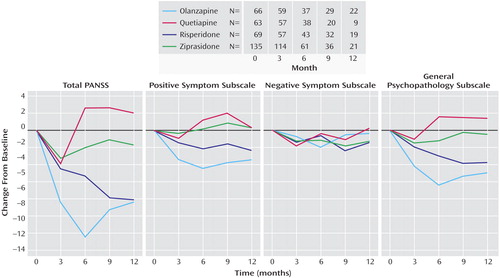
a Estimates of change from baseline are least squares means from a mixed model which assumed that data were missing at random.
Results for the PANSS positive symptom subscale were similar to the total score. Significant pairwise differences were found for olanzapine versus ziprasidone (estimated mean difference=–3.4, SE=0.7 [p<0.001]), quetiapine (difference=–3.3, SE=0.8 [p<0.001]), and risperidone (difference=–1.9, SE=0.7 [p<0.02]). The risperidone group improved more than the ziprasidone group (difference=–1.5, SE=0.6 [p<0.03]). No treatment differences were found for PANSS negative symptoms, and results for the PANSS general psychopathology subscale mirrored the total score. No treatment group differences were identified for change in CGI severity ratings.
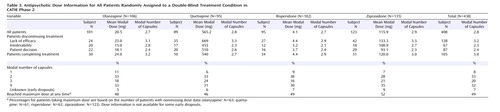
Dose and Discontinuation Rates
Table 3 shows the proportion of patients assigned to each drug whose modal dose was 1, 2, 3, and 4 capsules during phase 2. The table also shows the modal doses of subjects according to the reasons for leaving the phase. For each drug, the highest mean modal doses among patients who discontinued early were for those who stopped because of inefficacy.
Adverse Events and Safety Outcomes
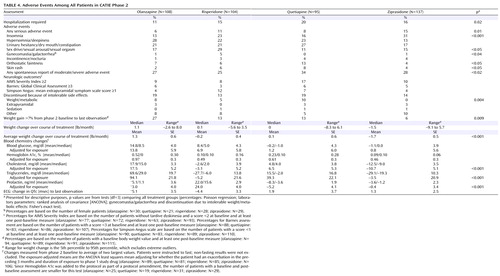
Adverse events and side effects rates are listed in Table 4 . Accounting for multiple hospitalizations and for the differential time in treatment, the number of hospitalizations for exacerbation of schizophrenia per person-years of exposure was lower in the olanzapine group (0.28) than in those receiving risperidone (0.40), ziprasidone (0.48), or quetiapine (0.70).
Significantly lower rates of insomnia were seen in patients receiving olanzapine (13%) and quetiapine (16%) relative to patients receiving risperidone (23%) or ziprasidone (31%). Patients receiving risperidone experienced higher rates of adverse effects involving sexual functioning (29%) relative to the other groups (11%–17%). Risperidone was also associated with higher rates of gynecomastia or galactorrhea (5%) relative to the other groups (<1%). More patients receiving quetiapine experienced orthostatic faintness (13%) relative to the other groups (4%–7%). Patients receiving quetiapine also spontaneously reported other adverse events more often than did those in the other treatment groups (34% versus 25%–28%).
Neurologic side effects
There were no differences in the incidence of extrapyramidal side effects, akathisia, or abnormal movements between the drugs as reflected by rating scale measures of severity or reasons for discontinuing treatment.
Weight gain and metabolic changes
Patients receiving olanzapine gained more weight than did patients receiving any of the other drugs, with a mean of 1.3 pounds per month. Patients receiving ziprasidone had a mean loss of 1.7 pounds per month. Those receiving risperidone and quetiapine had negligible mean changes in weight over the course of phase 2. A larger proportion of patients receiving olanzapine gained over 7% of their baseline body weight compared with risperidone, quetiapine, and ziprasidone. No patients receiving ziprasidone discontinued treatment because of weight gain or metabolic side effects as opposed to patients receiving risperidone (5%), olanzapine (8%), or quetiapine (10%).
Among the 61 patients who gained over 7% of their body weight in the previous phase, 42% of those assigned to ziprasidone lost over 7% of their body weight as compared to 20% for risperidone, 7% for quetiapine, and none for olanzapine. Mean weight change in pounds among this group who gained substantial weight in the previous phase was –11.3 (SE=4.6) for ziprasidone, –1.4 (SE=3.5) for risperidone, 0.0 (SE=3.1) for quetiapine, and 2.1 (SE=2.9) for olanzapine.
Olanzapine was associated with substantial increases in total cholesterol and triglycerides, whereas risperidone and ziprasidone were associated with decreases in these parameters, even after we adjusted for drug exposure ( Table 4 ). Only risperidone was associated with a substantial increase in prolactin levels.
Other adverse events
The medications exhibited no substantially different effects on the electrocardiographic QTc interval or incidence of new cataracts. Ziprasidone was associated with more serious adverse events other than hospitalizations for schizophrenia than the other treatments (15% versus 6–11%). Although no clear pattern of serious adverse events was noted, there were two completed suicides among patients receiving ziprasidone. The only other completed suicide was in a patient taking risperidone.
Discussion
In this group of patients with chronic schizophrenia who were randomly assigned to a new antipsychotic after discontinuing a previous antipsychotic drug within the context of a multiphase randomized clinical trial, olanzapine and risperidone were more effective than quetiapine and ziprasidone as reflected by longer time until discontinuation for any reason.
Our hypothesis that ziprasidone would be most effective in this “tolerability pathway” was not confirmed, although ziprasidone was associated with weight loss and favorable changes in lipid parameters. Risperidone was also associated with modest improvements in weight and lipid parameters.
This study had broad inclusion and minimal exclusion criteria and allowed comorbid conditions and concomitant medications. Study participants had chronic schizophrenia, with an average duration since first treatment with an antipsychotic drug of almost 14 years. The study was designed to mimic usual practice. It was conducted at an array of clinical settings in which people with schizophrenia are treated, and when one antipsychotic drug was discontinued a subsequent antipsychotic drug trial followed. However, because treatment was double-blind, patient and clinician discomfort with not knowing what treatment was given may have led to a higher rate of discontinuations in this study than would be expected in typical practice settings. It is important to note that in the study, as in usual treatment, discontinuation of a drug does not mean that treatment has failed. Doctors and patients often work together in multiple drug trials before one is found that is adequately efficacious, safe, and acceptable for an individual.
This study did not include aripiprazole, which was approved by the FDA in November 2002, or any first-generation antipsychotics. First-generation drugs were omitted because we had hypothesized that they were less effective than the second-generation drugs and less well tolerated. We tested this hypothesis in phase 1 and found that the representative first-generation drug, perphenazine, was similar in effectiveness to quetiapine, risperidone, and ziprasidone, and only modestly less effective than olanzapine (1) .
The main outcome measure, treatment discontinuation for any reason, was selected as a global measure of a drug’s acceptability and effectiveness. The different characteristics of drugs, patients, and clinicians may lead to variation in how decisions to discontinue treatment are made. For example, if unpleasant side effects like sedation or akathisia occur they might lead to early discontinuation, while weight gain or changes in laboratory chemistries might be less noticeable initially and could lead to later discontinuations. Similarly, poor control of positive symptoms may lead to relatively early discontinuation, whereas negative symptoms may be better tolerated early in treatment.
The results of this study are highly consistent with the results of phase 1 of the CATIE investigation (1) except for the fact that risperidone was somewhat more effective in this phase. We compared the characteristics of patients entering this phase to those in phase 1 to understand the reasons for this difference. The most striking difference was that most individuals who discontinued phase 1 due to “patient decision,” indicating a lack of agreement between doctor and patient to continue the medication, did not enter phase 2. Further, 99 patients who discontinued the previous phase due to inefficacy entered the phase 2 efficacy pathway, which included clozapine rather than ziprasidone. Thus, the group of patients enrolled in the currently reported study had an enhanced proportion of individuals who poorly tolerated their previous treatment and who were adherent with their doctor’s recommendations relative to those in phase 1.
The doses used in the study may have affected the results because the dose ranges for quetiapine, risperidone, and ziprasidone may not have been optimal (17 , 18) . However, dose ranges in this study were based on input from the manufacturer of each drug and knowledge of clinical practice patterns. Moreover, the average prescribed doses of these drugs in the U.S. for patients with schizophrenia during the period in which the study was conducted (olanzapine, 14 mg/day; risperidone, 3.8 mg/day; quetiapine, 388 mg/day; ziprasidone, 125 mg/day) (19) were generally comparable to those in the present study. The dosing data, which showed that doses associated with discontinuations due to lack of efficacy were higher in the available range than were doses associated with discontinuations due to intolerability or patient decision, suggests that doses were raised in response to inadequate therapeutic response.
Patients with chronic schizophrenia discontinued antipsychotic study medications at a high rate in both the first and second phases of the CATIE study, indicating substantial limitations of the drugs studied. Among the individuals who discontinued olanzapine, quetiapine, risperidone, or ziprasidone immediately before entering the second phase reported here, olanzapine and risperidone appeared more effective than quetiapine and ziprasidone as reflected by longer time until treatment discontinuation for any reason. Olanzapine was the most effective medication for those who stopped their previous treatment because of inefficacy but not for patients who stopped their previous treatment because of intolerability or other reasons. Risperidone was similarly effective among patients who discontinued their previous treatment because of intolerability and those who discontinued because of inefficacy.
1. Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, Keefe RS, Davis SM, Davis CE, Lebowitz BD, Severe J, Hsiao JK: Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005; 353:1209–1223Google Scholar
2. Chakos M, Lieberman J, Hoffman E, Bradford D, Sheitman B: Effectiveness of second-generation antipsychotics in patients with treatment-resistant schizophrenia: a review and meta-analysis of randomized trials. Am J Psychiatry 2001; 158:518–526Google Scholar
3. Tuunainen A, Wahlbeck K, Gilbody S: Newer atypical antipsychotic medication in comparison to clozapine: a systematic review of randomized trials. Schizophr Res 2002; 56(1–2):1–10Google Scholar
4. Wahlbeck K, Cheine M, Essali A, Adams C: Evidence of clozapine’s effectiveness in schizophrenia: a systematic review and meta-analysis of randomized trials. Am J Psychiatry 1999; 156:990–999Google Scholar
5. Lehman AF, Lieberman JA, Dixon LB, McGlashan TH, Miller AL, Perkins DO, Kreyenbuhl J: Practice guideline for the treatment of patients with schizophrenia, 2nd ed. Am J Psychiatry 2004; 161(Feb suppl):1–56Google Scholar
6. Davis JM, Chen N, Glick ID: A meta-analysis of the efficacy of second-generation antipsychotics. Arch Gen Psychiatry 2003; 60:553–564Google Scholar
7. Leucht S, Pitschel-Walz G, Abraham D, Kissling W: Efficacy and extrapyramidal side-effects of the new antipsychotics olanzapine, quetiapine, risperidone, and sertindole compared to conventional antipsychotics and placebo: a meta-analysis of randomized controlled trials. Schizophr Res 1999; 35:51–68Google Scholar
8. Leucht S, Wahlbeck K, Hamann J, Kissling W: New generation antipsychotics versus low-potency conventional antipsychotics: a systematic review and meta-analysis. Lancet 2003; 361:1581–159Google Scholar
9. Henderson DC, Cagliero E, Copeland PM, Borba CP, Evins E, Hayden D, Weber MT, Anderson EJ, Allison DB, Daley TB, Schoenfeld D, Goff DC: Glucose metabolism in patients with schizophrenia treated with atypical antipsychotic agents: a frequently sampled intravenous glucose tolerance test and minimal model analysis. Arch Gen Psychiatry 2005; 62:19–28Google Scholar
10. Koro CE, Fedder DO, L’Italien GJ, Weiss S, Magder LS, Kreyenbuhl J, Revicki D, Buchanan RW: An assessment of the independent effects of olanzapine and risperidone exposure on the risk of hyperlipidemia in schizophrenic patients. Arch Gen Psychiatry 2002; 59:1021–1026Google Scholar
11. Keefe RS, Mohs RC, Bilder RM, Harvey PD, Green MF, Meltzer HY, Gold JM, Sano M: Neurocognitive assessment in the clinical antipsychotic trials of intervention effectiveness (CATIE) project schizophrenia trial: development, methodology, and rationale. Schizophr Bull 2003; 29:45–55Google Scholar
12. Stroup TS, McEvoy JP, Swartz MS, Byerly MJ, Glick ID, Canive JM, McGee MF, Simpson GM, Stevens MC, Lieberman JA: The National Institute of Mental Health Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) project: schizophrenia trial design and protocol development. Schizophr Bull 2003; 29:15–31Google Scholar
13. Swartz MS, Perkins DO, Stroup TS, McEvoy JP, Nieri JM, Haak DC: Assessing clinical and functional outcomes in the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia trial. Schizophr Bull 2003; 29:33–43Google Scholar
14. Davis SM, Koch GG, Davis CE, LaVange LM: Statistical approaches to effectiveness measurement and outcome-driven re-randomizations in the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) studies. Schizophr Bull 2003; 29:73–80Google Scholar
15. Cox D: Regression models and life tables. J R Statist Soc 1972; B34:187–220Google Scholar
16. Hochberg Y: A sharper Bonferroni procedure for multiple tests of significance. Biometrika 1988; 75:800–802Google Scholar
17. Citrome L, Volavka J: Optimal dosing of atypical antipsychotics in adults: a review of the current evidence. Harv Rev Psychiatry 2002; 10:280–291Google Scholar
18. Davis JM, Chen N: Dose response and dose equivalence of antipsychotics. J Clin Psychopharmacol 2004; 24:192–208Google Scholar
19. IMS Health Inc: International Medical Systems National Disease and Therapeutic Index. Plymouth Meeting, Pa, IMS Health, Jan 2001-Dec 2004Google Scholar